Abstract
Objective
To investigate the usefulness of cardiac biomarkers in the evaluation of prognosis and cardiac involvement (CI) in patients with acute aortic syndrome (AAS).
Methods
A total of 260 AAS patients with the measurements of cardiac biomarkers were divided into 2 groups; the survived (n=215, 60.6±13.7 years, 110 males) vs the dead (n=45, 64.5±13.6 years, 19 males). N-terminal pro-B-type natriuretic peptide (NT-proBNP), cardiac specific troponin-I (cTnI), C-reactive protein (CRP), creatinine kinase (CK), MB fraction of CK (CK-MB), and D-dimer were compared.
Results
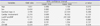
NT-proBNP and D-dimer were significantly elevated in the dead group than in the survived group (3558.7±5497.2 vs 949.9±2307.3 pg/mL, p<0.001, 4.5±5.1 vs 2.0±3.2 ug/mL, p<0.001, respectively). CI was observed in 59 patients (22.7%), and NT-proBNP was significantly elevated in patients with CI than in patients without CI (2497.7±4671.3 vs 722.5±1489.1 pg/mL, p=0.034). In univariate analysis, Stanford type A, CI, NT-proBNP, and D-dimer were significantly associated with mortality, but NT-proBNP was the only significant independent predictor of mortality in multivariate analysis. By receiver operating characteristic curve analysis, the optimal cut-off value to predict mortality was 517.0 pg/mL for NT-proBNP (area under the curve 0.797, sensitivity 86.7%, specificity 71.7%).
Figures and Tables
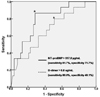 | Fig. 1Receiver operating characteristic curve analysis to predict mortality in acute aortic syndrome. Asterisk indicates the optimal cut-off value. NT-proBNP; N-terminal pro B-type natriuretic peptide. |
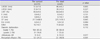
Table 1
Baseline clinical characteristics between the groups

Table 2
Echocardiographic findings between the groups
Values are means±SD.
LVEDD; left ventricular end-diastolic dimension, LVESD; left ventricular end-systolic dimension, LVEF; left ventricular ejection fraction, E; early diastolic mitral inflow velocity, A; late diastolic mitral inflow velocity, DT; deceleration time, Em; early diastolic velocity of septal annulus, AR; aortic regurgitation
Table 3
Cardiac biomarkers and mortality between the groups

Table 4
Differences of cardiac biomarkers according to the Stanford classification of acute aortic syndrome

Table 5
Differences of cardiac biomarkers according to the cardiac involvement in patients with acute aortic syndrome

Table 6
Cardiac involvement and Stanford classification
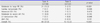
Table 7
Cardiac involvement between the survived and the dead
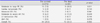
Table 8
Independent predictor of mortality in acute aortic syndrome
References
2. Song JK, Kang SJ, Song JM, Kang DH, Song H, Chung CH, et al. Factors associated with in-hospital mortality in patients with acute aortic syndrome involving the ascending aorta. Int J Cardiol. 2007; 115:14–18.

3. Vasan RS. Biomarkers of cardiovascular disease: molecular basis and practical considerations. Circulation. 2006; 113:2335–2362.
4. McLean AS, Huang SJ. Cardiac biomarkers in the intensive care unit. Ann Intensive Care. 2012; 2:8–18.

6. Wen D, Zhou XL, Li JJ, Hui RT. Biomarkers in aortic dissection. Clin Chim Acta. 2011; 412:688–695.

7. Sugano Y, Anzai T, Yoshikawa T, Satoh T, Iwanaga S, Hayashi T, et al. Serum C-reactive protein elevation predicts poor clinical outcome in patients with distal type acute aortic dissection: association with the occurrence of oxygenation impairment. Int J Cardiol. 2005; 102:39–45.

8. Linder N, Treitl M, Nikolaou K, Juchem G, Pichlmaier M, Reiser MF, et al. Acute aortic syndrome. Radiologe. 2012; 52:844–848.
9. Parthenakis F, Koutalas E, Patrianakos A, Koukouvas M, Nyktari E, Vardas P. Diagnosing acute aortic syndromes: the role of specific biochemical markers. Int J Cardiol. 2010; 145:3–8.

10. Tokita Y, Kusama Y, Kodani E, Tadera T, Nakagomi A, Atarashi H, et al. Utility of rapid D-dimer measurement for screening of acute cardiovascular disease in the emergency setting. J Cardiol. 2009; 53:334–340.

12. D'Aloia A, Faggiano P, Brentana L, DeiCas L. D-dimer serum levels in a case of type B aortic dissection A rapid test for the early diagnosis of acute aortic disease? J Cardiovasc Med (Hagerstown). 2006; 7:216–218.
13. Wen D, Wu HY, Jiang XJ, Zhang HM, Zhou XL, Li JJ, et al. Role of plasma C-reactive protein and white blood cell count in predicting in-hospital clinical events of acute type A aortic dissection. Chin Med J (Engl). 2011; 124:2678–2682.
14. Sbarouni E, Georgiadou P, Marathias A, Geroulanos S, Kremastinos DT. D-dimer and BNP levels in acute aortic dissection. Int J Cardiol. 2007; 122:170–172.

15. Sodeck G, Domanovits H, Schillinger M, Janata K, Thalmann M, Ehrlich MP, et al. Pre-operative N-terminal pro-brain natriuretic peptide predicts outcome in type A aortic dissection. J Am Coll Cardiol. 2008; 51:1092–1097.

16. Cho JR, Shin S, Kim JS, Ko YG, Hong MK, Jang Y, et al. Clinical characteristics of acute aortic syndrome in Korean patients: from the Korean multi-center registry of acute aortic syndrome. Korean Circ J. 2012; 42:528–537.

18. Yamashita T, Seino Y, Ogawa A, Ogata K, Fukushima M, Tanaka K, et al. N-terminal pro-BNP is a novel biomarker for integrated cardio-renal burden and early risk stratification in patients admitted for cardiac emergency. J Cardiol. 2010; 55:377–383.

19. Emdin M, Vittorini S, Passino C, Clerico A. Old and new biomarkers of heart failure. Eur J Heart Fail. 2009; 11:331–335.

20. Tschöpe C, Kasner M, Westermann D, Gaub R, Poller WC, Schultheiss HP. The role of NT-proBNP in the diagnostics of isolated diastolic dysfunction: correlation with echocardiographic and invasive measurements. Eur Heart J. 2005; 26:2277–2284.

21. Kehl DW, Iqbal N, Fard A, Kipper BA, De La Parra Landa A, Maisel AS. Biomarkers in acute myocardial injury. Transl Res. 2012; 159:252–264.

22. Bonnefoy E, Godon P, Kirkorian G, Chabaud S, Touboul P. Significance of serum troponin I elevation in patients with acute aortic dissection of the ascending aorta. Acta Cardiol. 2005; 60:165–170.

24. Imoto K, Uchida K, Karube N, Yasutsune T, Cho T, Kimura K, et al. Risk analysis and improvement of strategies in patients who have acute type A aortic dissection with coronary artery dissection. Eur J Cardiothorac Surg. 2013; 44:419–424.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download