Abstract
Objective
The aim of this study is to compare the clinical benefits between high-intensity and low-to moderate-intensity statin therapy in patients with acute myocardial infarction (AMI).
Methods
A total of 1,230 patients in the Korea AMI Registry (KAMIR) were enrolled. Patients were divided into two groups according to the dosage of statin for the secondary prevention after AMI.
The primary endpoint was composite of major adverse cardiac events (MACEs) including cardiac death, non-fatal MI, repeat revascularization during the 12 months of clinical follow-up.
Result
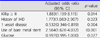
The primary endpoint occurred in 101 patients (11.3%) from the low-to moderate-intensity statin group and 45 patients (13.4%) from the high-intensity statin group. The cumulative incidence of MACEs during 12-month follow-up was not significantly different between the two groups (p=0.323). After multi-variate analysis, MACEs-free survival rate was not significantly different between the two groups.
Figures and Tables
 | Fig. 1Kaplan-Meier curve for 12-month major adverse cardiac event-free survival rates between low-intermediate intensity statin group and high intensity statin group. |
ACKNOWLEDGEMENTS
This study was supported by a grant of the National Research Foundation of Korea Grant funded by the Korean Government (MEST), Republic of Korea (2010-0020261), and the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI12C0199, HI13C1527).
References
1. Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004; 350:1495–1504.

2. Cannon CP, Steinberg BA, Murphy SA, Mega JL, Braunwald E. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol. 2006; 48:438–445.

3. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2889–2934.

4. Arai H, Sasaki J, Teramoto T. Comment on the new guidelines in USA by the JAS guidelines committee. J Atheroscler Thromb. 2014; 21:79–81.

5. Kwon JE, Kim Y, Hyun S, Won H, Shin SY, Lee KJ, et al. Cholesterol lowering effects of low-dose statins in Korean patients. J Lipid Atheroscler. 2014; 3:21–28.

6. Preiss D, Seshasai SR, Welsh P, Murphy SA, Ho JE, Waters DD, et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011; 305:2556–2564.

7. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Circulation. 2012; 126:2020–2035.

8. Vaughan CJ, Gotto AM Jr, Basson CT. The evolving role of statins in the management of atherosclerosis. J Am Coll Cardiol. 2000; 35:1–10.

9. Kavousi M, Leening MJ, Nanchen D, Greenland P, Graham IM, Steyerberg EW, et al. Comparison of application of the ACC/AHA guidelines, Adult Treatment Panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014; 311:1416–1423.

10. Giraldez RR, Giugliano RP, Mohanavelu S, Murphy SA, McCabe CH, Cannon CP, et al. Baseline low-density lipoprotein cholesterol is an important predictor of the benefit of intensive lipid-lowering therapy: a PROVE IT-TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis In Myocardial Infarction 22) analysis. J Am Coll Cardiol. 2008; 52:914–920.

11. Olsson AG, Schwartz GG, Szarek M, Luo D, Jamieson MJ. Effects of high-dose atorvastatin in patients ≥65 years of age with acute coronary syndrome (from the myocardial ischemia reduction with aggressive cholesterol lowering [MIRACL] study). Am J Cardiol. 2007; 99:632–635.

12. Deedwania P, Stone PH, Bairey Merz CN, Cosin-Aguilar J, Koylan N, Luo D, et al. Effects of intensive versus moderate lipid-lowering therapy on myocardial ischemia in older patients with coronary heart disease: results of the Study Assessing Goals in the Elderly (SAGE). Circulation. 2007; 115:700–707.

13. Mills EJ, O'Regan C, Eyawo O, Wu P, Mills F, Berwanger O, et al. Intensive statin therapy compared with moderate dosing for prevention of cardiovascular events: a meta-analysis of >40 000 patients. Eur Heart J. 2011; 32:1409–1415.

14. JCS Joint Working Group. Guidelines for secondary prevention of myocardial infarction (JCS 2011). Circ J. 2013; 77:231–248.
16. Yang J, Li LJ, Wang K, He YC, Sheng YC, Xu L, et al. Race differences: modeling the pharmacodynamics of rosuvastatin in Western and Asian hypercholesterolemia patients. Acta Pharmacol Sin. 2011; 32:116–125.

17. Lee E, Ryan S, Birmingham B, Zalikowski J, March R, Ambrose H, et al. Rosuvastatin pharmacokinetics and pharmacogenetics in white and Asian subjects residing in the same environment. Clin Pharmacol Ther. 2005; 78:330–341.

18. Lee HY, Cho HJ, Kim HY, Jeon HK, Shin JH, Kang SM, et al. Effects of intensive versus mild lipid lowering by statins in patients with ischemic congestive heart failure: Korean Pitavastatin Heart Failure (SAPHIRE) study. Korean J Intern Med. 2014; 29:754–763.

19. Sakamoto T, Ogawa H. "Just make it lower" is an alternative strategy of lipid-lowering therapy with statins in Japanese patients: LDL-cholesterol: the lower, the better; is it true for Asians? (Con). Circ J. 2010; 74:1731–1741.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download