Abstract
We report a case of a superficial femoral artery pseudoaneurysm in 52-year old patient with a history of having renal allograft. The pseudoaneurysm spontaneously developed while standing up from squatting position after defecation, and it was successfully managed by an endovascular repair with an endograft. This case suggests that an atherosclerotic superficial femoral artery is vulnerable to torsion and tension movement during changing position from squatting to standing, which is repeatedly practiced by the people using the Korean traditional toilet. The endovascular therapy is also recommended for elderly patients with poor clinical conditions such as having a renal allograft and diffuse atherosclerosis of peripheral arteries.
Recently, there have been 0.3% of significant decrease in the incidents of pseudoaneurysms from diagnostic or interventional procedures through a femoral artery.1 However, with eight cases documented in the literature so far, a spontaneous rupturing of the femoral artery is extremely uncommon,2 and there is no clearly known cause yet. We report a rare case of a spontaneous pseudoaneurysm of superficial femoral artery, in a renal allograft patient with chronic rejection and without any diagnostic or therapeutic procedures.
A 52-year-old man complained of a persistent pain and swelling in the left thigh which suddenly developed one month ago, during standing up from the squatting position while he was using the Korean traditional lavatory. The swollen area progressively increased in size over one month. Initially, he visited our outpatient nephrology department and was hospitalized due to a suspicion of rhabdomyolysis. However, the laboratory value of creatine kinase (CK) was within the normal range, and the musculoskeletal sonograph showed a 2.5×1.4×2.1 cmsized subfascial fluid collection, suggesting a hematoma in deep layer of the medial aspect of the left distal thigh. As the pain in the left thigh was alleviated and the circumference of the left thigh was no longer increased, the patient was discharged after a bed rest and the application of an elastic bandage several days later. However, the pain in the thigh mildly continued after the discharge, while the left thigh progressively increased in size. On the date of readmission one month later, the patient had extremely severe pain to the level of immobility.
The patient was diagnosed with hypertension and diabetes mellitus 12 years ago, received a renal allograft due to an End-Stage Renal Disease (ESRD) 3 years ago, and had been taking immunosuppressant and steroid therapy to date. In order to screen the rejection response after an elevated blood creatinine level, a kidney biopsy was carried out 4 months ago and a T cell-mediated chronic rejection was diagnosed.
On presentation, the patient was hemodynamically stable with a pulsatile tender swelling of the medial aspect of the left distal thigh, and the pedal pulses were normal. The neurologic examination showed a mild paresthesia of the left lower limb without motor impairment. No oral or genital ulcers, hypermobile joints, or other physical findings which may suggest a connective tissue disease could be observed.
A rheumatologic evaluation was done and the results were as follows: Ig G of 1,050 mg/dL (standard 700-1,600 mg/dL), Ig A of 252 mg/dL (standard 70-400 mg/dL), Ig M of 54 mg/dL (standard 40-230 mg/dL), and negative antineutrophil cytoplasmic antibody and antinuclear antibody. These values show that there is no evidence of a connective tissue disease or vasculitis.
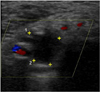
In the Doppler sonography of the left thigh, an increased-sized (11.2×6.8×12 cm) hematoma including 1.8×1.3 cm-sized pseudoaneurysm was shown, which was communicated with the left superficial femoral artery (SFA), suggesting a spontaneous rupturing of the left SFA (Fig. 1A and 1B). A Computed tomography angiography was not performed due to the raised serum creatinine of 2.0 mg/dL. An endovascular treatment was chosen due to the arterial calcification and the patient's age. A 5F introducer sheath was exchanged for a 45-cm 8F long sheath in order to cross the iliac bifurcation, and systemic heparin (100 U/kg) was administered. The angiographic examination showed a pseudoaneurysm at the distal part of the left SFA (Fig. 2A). A hydrophilic guidewire was pushed distally to pass the arterial wall lesion. A nitinol-polytetrafluoroethylene Viabahn® self-expanding stent-graft (8-mm diameter × 150-mm length, W.L. Gore & Associates, Inc.; Flagstaff, Ariz) was placed. After its deployment, the stent-graft was dilated and modeled by an 8-mm balloon (Fig. 2B). In the angiographic examination, a complete exclusion of the pseudoaneurysm was shown (Fig. 2C). In the follow up, vascular ultrasound also showed a complete thrombosis of the pseudoaneurysm (Fig. 3). The pulse at the left dorsalis pedis artery was good. The patient's condition was monitored in the intensive care unit for 24 hours thereafter. The patient's postoperative period was stable without renal deterioration, and the pain and size of the thigh progressively decreased. The patient was discharged from the hospital in good condition 11 days postoperative.
Pseudoaneurysms of the femoral artery are very rare, and they usually occur due to blunt or a penetrating trauma and also in association with bone fractures, bone tumors, or orthopedic procedures.3,4,5 The pseudoaneurysms from an access to the femoral artery occur in up to 0.7% of the diagnostic procedures and in up to 8% of the interventional procedures.6 Usually, they may be developed by complicated procedures, anticoagulants, arteriovenous fistula formation, and use of a large diameter catheter. The incidence of pseudoaneurysm has been significantly decreased by <0.3%, recently.1 A spontaneous rupturing of the femoral artery without those procedures is extremely uncommon and the cause is not clear.2 For the etiologic factors for the spontaneous pseudoaneurysms, some investigators have considered atherosclerosis in elderly patients and the inherited connective tissue disorders or congenital arterial abnormalities such as the Ehlers-Danlos syndrome in young patients.7,8 Spontaneous rupturing of the arteries, after a low-degree trauma or sport activities, occurring due to the fragility of their arterial walls were reported in subjects with inherited connective tissue disorders.9 In elderly patients, on the other hand, atherosclorosis has been proposed as the most common etiologic factor in the spontaneous perforation of the femoral arteries or its branches.10,11,12 Atherosclerosis and the weakness of the arterial wall can result in an easy rupturing of the plaque and consequently lead to pseudoaneurysms.
In the clinic, pseudoaneurysms usually present as a painful, tender, and pulsatile mass with a continuous bruiting in auscultation. However, a pseudoaneurysm can occur without a history of trauma, the clinical features of a connective tissue disorder or the evidence of atherosclerosis in an angiogram. A color Doppler sonography, which is also a sensitive and specific investigative technique to verify location and size of mass, can be used to screen a pseudoaneurysm or an arteriovenous aneurysm. However, a color Doppler sonography can result in an incomplete or inaccurate diagnosis, if there is a massive hematoma present.13 A Magnetic resonance angiography or a spiral computed tomographic angiography can be helpful in the precise delineation of the site of rupture and the dimensions of the pseudoaneurysm.
Femoral pseudoaneurysm has been traditionally treated with open surgical repair. However, there are other therapeutic options such as ultrasound-guided compression, ultrasound-guided thrombin injection, coil embolization, and the endovascular repair using stent grafts.14 In particular, an appropriate approach in young patients is an open surgical repair with hematoma evacuation, arterial suture, patch angioplasty, or a graft interposition.15 On the other hand, an endovascular exclusion with a covered stent-graft can be considered as the treatment of choice in elderly patients. This should be considered because a severely compromised arterial wall is usually difficult to surgically repair, because there is an increased risk of morbidity and mortality after an open surgery.
In our case report, a spontaneous rupturing of the SFA occurred without any apparent cause or trauma, in a patient with chronic rejection after kidney transplantation. The injury in this case occurred while the patient was changing position from squatting to standing during the use of a traditional Korean lavatory, which is commonly practiced by many elderlies in Korea. The patient was successfully treated with an endovascular self-expandable stent-graft deployment.
Figures and Tables
Fig. 1
Vascular ultrasound of the left thigh before endovascular treatment is shown. (A) The initial vascular ultrasound of the left thigh sonography showed a large (11.2×6.8×12 cm) hematoma including a 1.8×1.3 cm-sized pseudoaneurysm, (B) The pseudoaneurysm was communicated with the left superficial femoral artery, suggesting a spontaneous rupturing of left superficial femoral artery.
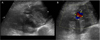
Fig. 2
Endovascular treatment of the pseudonaeurysm of left superficial femoral artery. (A) The peripheral angiography showed a pseudoaneurysm at the distal part of the left superficial femoral artery, (B) A self-expanding stent-graft (Viabahn® self-expanding stent-graft (8-mm diameter × 150-mm length)) was deployed to cover the pseudoaneurysm, and it was dilated and modeled by a 8 mm balloon, (C) The final angiography revealed a complete exclusion of the pseudoaneurysm.

References
1. Applegate RJ, Sacrinty MT, Kutcher MA, Kahl FR, Gandhi SK, Santos RM, et al. Trends in vascular complications after diagnostic cardiac catheterization and percutaneous coronary intervention via the femoral artery, 1998 to 2007. JACC Cardiovasc Interv. 2008; 1:317–326.

2. Kanko M, Ciftci E. Spontaneous pseudoaneurysm of the superficial femoral artery in Behcet's disease endovascular stent-graft treatment combined with percutaneous drainage: a case report. Heart Surg Forum. 2007; 10:E84–E86.
3. Merkus JW, Nieuwenhuijzen GA, Jacobs PP, van Roye SF, Koopman R, Pruszczynski MS, et al. Traumatic pseudoaneurysm of the superficial temporal artery. Injury. 1994; 25:468–471.

4. Blazick E, Keeling WB, Armstrong P, Letson D, Back M. Pseudoaneurysm of the superficial femoral artery associated with osteochondroma--a case report. Vasc Endovascular Surg. 2005; 39:355–358.

5. Yang KH, Park HW, Park SJ. Pseudoaneurysm of the superficial femoral artery after closed hip nailing with a Gamma nail: report of a case. J Orthop Trauma. 2002; 16:124–127.

6. Katzenschlager R, Ugurluoglu A, Ahmadi A, Hülsmann M, Koppensteiner R, Larch E, et al. Incidence of pseudoaneurysm after diagnostic and therapeutic angiography. Radiology. 1995; 195:463–466.

7. Goh BK, Chen CY, Hoe MN. Bilateral spontaneous rupture of the muscular branch of the superficial femoral artery with pseudoaneurysm formation. Ann Vasc Surg. 2004; 18:736–739.

8. Cadier MA, Watkin G, Pope FM, Marston A. Spontaneous rupture of the femoral arteries. J R Soc Med. 1993; 86:54.
9. Calligaro KD, Savarese RP, Goldberg D, Doerr KJ, Dougherty MJ, DeLaurentis DA. Deep femoral artery pseudoaneurysm caused by acute trunk and hip torsion. Cardiovasc Surg. 1993; 1:392–394.
10. Lossef SV, Gomes MN, Barth KH. Hemorrhage from spontaneous rupture of muscular branches of the superficial femoral artery. J Vasc Interv Radiol. 1994; 5:147–148.

11. Origuchi N, Shigematsu H, Nunokawa M, Yasuhura H, Muto T. Spontaneous perforation of a non-aneurysmal atherosclerotic abdominal aorta or femoral artery. Cardiovasc Surg. 1996; 4:351–355.

12. King JN, Kaupp HA. Spontaneous rupture of the superficial femoral artery with formation of a false aneurysm. J Cardiovasc Surg (Torino). 1970; 11:398–400.
13. Helvie MA, Rubin JM, Silver TM, Kresowik TF. The distinction between femoral artery pseudoaneurysms and other causes of groin masses: value of duplex Doppler sonography. AJR Am J Roentgenol. 1988; 150:1177–1180.

14. Corriere MA, Guzman RJ. True and false aneurysms of the femoral artery. Semin Vasc Surg. 2005; 18:216–223.

15. Siani A, Flaishman I, Siani LM, Mounayergi F, Zaccaria A, Schioppa A, et al. Spontaneous rupture of the superficial femoral artery treated via an endovascular approach. Tex Heart Inst J. 2008; 35:66–68.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download