Abstract
Left-sided portal hypertension and consequent gastric varices can occur in patients with isolated splenic vein thrombosis. It is a rare but clinically significant and curable cause of gastrointestinal hemorrhage. Our patient, a 20-year-old woman, with left flank pain was diagnosed with having idiopathic splenic vein thrombosis with resultant splenic infarction. Thorough workups for the possible etiologies of splenic vein thrombosis were all negative. After six months of anticoagulation, follow-up computed tomography revealed formation of gastric varices; one month following the discovery, she developed gastrointestinal bleeding. Splenectomy was performed, resulting in the resolution of gastric varices.
Isolated splenic vein thrombosis is a rare cause of gastrointestinal bleeding. Left-sided portal hypertension and resultant formation of isolated fundal varices are the main mechanisms for variceal bleeding.1,2
Left-sided portal hypertension secondary to isolated splenic vein thrombosis is important because it can be cured with splenectomy, especially in cases complicated by gastric variceal bleeding.3,4,5,6
We report on a female patient with gastric variceal bleeding secondary to idiopathic splenic vein thrombosis successfully treated with laparoscopic splenectomy.
A 20-year-old female patient visited our emergency department for left flank pain. She was suffering from postprandial fullness and dyspepsia for a week, and abruptly developed severe left flank pain. She did not have a significant medical or surgical history and did not take any medication. The vital signs were stable and the physical examination was unremarkable except for left upper quadrant tenderness. The hemoglobin level was 13.6 g/dL and the platelet count was 267,000/µL. Biochemical profiles, including amylase and lipase levels, were within normal limits. Abdominal computed tomography (CT) scan, and splanchnic artery CT angiography taken on the next day, revealed splenic vein thrombosis at the splenic hilum with splenic infarction (Fig. 1). However, there were no specific lesions in the pancreas. Workups for the etiology of venous thrombosis included testing for hereditary thrombophilia, fluorescent antinuclear antibody test, antiphospholipid syndrome, coagulation factor VIII activity, and Janus kinase 2 (JAK2) V617F gene mutation, but all of the tests failed to reveal any abnormalities. Anticoagulation was initiated with heparin and then was switched to warfarin, and the flank pain gradually decreased. Follow-up splanchnic artery CT angiography was taken a week later, and it showed no significant interval change. The patient was discharged with warfarin.
Six months later, follow-up CT angiography was performed at the outpatient clinic. It showed nearcomplete resolution of splenic infarcted area with splenomegaly, but revealed formation of gastric varices (Fig. 2A and 2B). Warfarin was discontinued because of the risk of potential variceal bleeding, and aspirin was prescribed instead.
About a month later, the patient developed melena and underwent endoscopic evaluation at a hospital located in Japan. Endoscopy showed bead-shaped gastric varices with bleeding induced by the gag reflex (Fig. 3A). At the time, the hemoglobin level was 7.9 g/dL and the platelet count was 161,000/µL. She was subsequently referred to our hospital. On arrival to our hospital, her blood pressure was 99/49 mmHg and pulse rate was 68/min. The physical examination revealed pale conjunctivae without any jaundice. The hemoglobin level was 8.6 g/dL and the platelet count was 174,000/µL. The patient's biochemical tests, including liver and kidney function tests, were within normal limits.
The patient underwent laparoscopic splenectomy, and pathological analysis of the resected spleen showed chronic passive congestion. Two weeks later, gastrofiberscopic examination did not reveal any gastric varices (Fig. 3B). Five months later, follow-up CT scan showed complete resolution of gastric varices (Fig. 2C).
Left-sided portal hypertension accounts for less than 5% of all cases with portal hypertension.7 Splenic vein thrombosis, which leads to left-sided portal hypertension and consequent formation of varices, is an uncommon cause of gastrointestinal hemorrhage.
Although there have been numerous reports dealing with cases of splenic vein thrombosis associated with pancreatic diseases, it is difficult to find another instance of idiopathic splenic vein thrombosis with the resultant gastric variceal bleeding after the one report in US in 1984.8 Pancreatic pathologies, including acute and chronic pancreatitis, pancreatic pseudocyst, and pancreatic tumor and abscess, remain the most common causes of splenic vein thrombosis.1,5,7,8 Non-pancreatic disease-associated etiologies of splenic vein thrombosis are traumas, gastric operations, umbilical vein catheterizations, lymphomas and sarcomas, other malignancies, retroperitoneal diseases, splenic artery aneurysms, myeloproliferative diseases, hereditary thrombocythemia, protein S deficiency, and systemic lupus erythematosus.1,7,8 In this patient, there was no history of surgery or trauma. We performed an abdominal CT scan to search for the cause of the splenic vein thrombosis, but the scan did not reveal any pancreatic abnormalities or evidence of malignancy. Complete blood cell count, pancreatic enzyme level, thrombotic disorder profiles, antiphospholipid antibody profiles, coagulation factor VIII activity were also within normal ranges. Fluorescent antinuclear antibody (FANA) and JAK2 V617F gene mutation tests were negative. Thus, we considered her splenic vein thrombosis to be idiopathic. According to a review of English literature from 1900 to 1968 by Sutton et al., 16 patients lacked an established cause among the 53 cases of isolated splenic vein thrombosis.5 Also, to our knowledge, this is the first case reporting idiopathic splenic vein thrombosis and gastric variceal bleeding in Korean literature.
Manifestations of splenic vein thrombosis include splenomegaly, splenic infarction, and gastric varices with left-sided portal hypertension.3,4,5 In patients with splenic vein thrombosis, the possibility of associated gastrointestinal bleeding should be considered. Gastrointestinal bleeding rate is reported to be 15-72% in patients with isolated splenic vein occlusion.2,5,6,9,10 In a review analyzing the natural history of pancreatitis-induced splenic vein thrombosis, the overall rate of associated GI bleeding was 12.3%.11
On the other hand, splenic vein thrombosis should be suspected in patients with gastric varices without evidence of liver disease, especially if splenomegaly is diagnosed.1,8 Splenectomy, which cures isolated gastric varices, has historically been the treatment of choice in the management of bleeding secondary to splenic vein thrombosis. In selected cases, splenic artery embolization has recently been described as therapy.1,4,5,6,10,12 However, there is a lack of verified data supporting the benefit of prophylactic splenectomy in asymptomatic cases with left-sided portal hypertension. Although some studies have recommended concomitant prophylactic splenectomy to be performed during pancreatic resection in patients with asymptomatic splenic vein thrombosis and chronic pancreatitis,10,13 the recommendation does not apply generally to patients that are not having other surgical procedures as there is no consensus on the use of routine prophylactic splenectomy.1,7,14 Nevertheless, splenectomy may be carried on in select groups, such as patients with intractable recurrent gastrointestinal bleeding and/or splenomegaly.2
One of the challenging issues in patients with isolated splenic vein thrombosis is the problem of anticoagulation. In mesenteric venous thrombosis, especially in acute or subacute cases, heparinization should be started immediately as it clearly increases survival and results in a significant decrease in the recurrence rate of thrombosis.15 In that situation, anticoagulation may be used even in the presence of gastrointestinal hemorrhage as long as the benefits of preventing bowel infarction outweigh the risks of bleeding, and the benefits of long-term anticoagulation exceed the risks of bleeding despite the eventual possibilities of formation of varices and resultant bleeding.15 Also, in non-cirrhotic portal hypertensive patients caused by Budd-Chiari syndrome, anticoagulation is generally advised; previous portal hypertension related bleeding is not considered to be a major contraindication for anticoagulation if proper prophylactic measures for recurrent hemorrhage are used.16 Similarly, in cases of acute portal vein thrombosis without cirrhosis, at least three months of anticoagulation is advocated with the stipulation of permanent anticoagulation in patients with ongoing hypercoagulable states.17 Furthermore, long-term anticoagulation should be carried out in patients with chronic portal venous thrombosis with permanent thrombotic risk factors after endoscopic screening for the formation of varices, with the prophylactic use of beta-blocker or endoscopic procedures as needed.17 However, in isolated splenic vein thrombosis, there is a lack of consensus recommendations for or against anticoagulation. Moreover, isolated splenic vein thrombosis, the majority of which is secondary to pancreatitis or pancreatic neoplasm, is differentiated from mesenteric venous thrombosis in that splenic vein thrombosis is usually associated with a local disease of the splenic vein rather than a systemic disease affecting the thrombotic pathway.15 Therefore, it may be reasonable to individualize anticoagulation therapy in patients with isolated splenic vein thrombosis with regard to underlying etiologies, potential risks of gastrointestinal bleeding, and the presence of ongoing ischemia or systemic hypercoagulable status.
In conclusion, splenic vein thrombosis is a rare, but important and curable cause of left-sided portal hypertension, which can manifest as gastric variceal bleeding. The diagnosis of splenic vein thrombosis should be kept in mind when examining patients with gastric varices without liver diseases. Splenectomy or splenic arterial embolization should be considered for cases complicated by variceal bleeding.
Figures and Tables
Fig. 1
Contrast-enhanced CT of the abdomen showing splenic vein thrombosis and splenic infarction. (A) Transverse CT image during the portal-venous phase revealed a wedge-shaped low-density lesion (white arrowhead) on superomedial aspect of the spleen, which is considered to be splenic infarction, (B) Image from the same CT scan also demonstrated splenic vein thrombosis (arrow) at the splenic hilum portion.
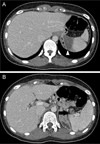
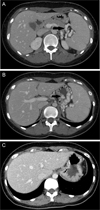
Fig. 2
Follow-up CT images showing venous collaterals and gastric varices. (A) Transverse CT image during the portal-venous phase revealed venous collaterals (arrow) around the splenic hilum, (B) Image from the same CT scan also demonstrated a conglomerate of gastric varices (arrow), (C) Follow-up CT scan taken 5 months after splenectomy showed resolution of gastric varices.
References
1. Köklü S, Köksal A, Yolcu OF, Bayram G, Sakaoğullari Z, Arda K, et al. Isolated splenic vein thrombosis: an unusual cause and review of the literature. Can J Gastroenterol. 2004; 18:173–174.

2. Köklü S, Yüksel O, Arhan M, Coban S, Başar O, Yolcu OF, et al. Report of 24 left-sided portal hypertension cases: a single-center prospective cohort study. Dig Dis Sci. 2005; 50:976–982.

3. Muhletaler C, Gerlock AJ Jr, Goncharenko V, Avant GR, Flexner JM. Gastric varices secondary to splenic vein occlusion: radiographic diagnosis and clinical significance. Radiology. 1979; 132:593–598.

4. Sato T, Yamazaki K, Toyota J, Karino Y, Ohmura T, Suga T. Gastric varices with splenic vein occlusion treated by splenic arterial embolization. J Gastroenterol. 2000; 35:290–295.

5. Sutton JP, Yarborough DY, Richards JT. Isolated splenic vein occlusion. Review of literature and report of an additional case. Arch Surg. 1970; 100:623–626.
6. Sakorafas GH, Sarr MG, Farley DR, Farnell MB. The significance of sinistral portal hypertension complicating chronic pancreatitis. Am J Surg. 2000; 179:129–133.

7. Köklü S, Coban S, Yüksel O, Arhan M. Left-sided portal hypertension. Dig Dis Sci. 2007; 52:1141–1149.

8. Goldberg S, Katz S, Naidich J, Waye J. Isolated gastric varices due to spontaneous splenic vein thrombosis. Am J Gastroenterol. 1984; 79:304–307.
9. Little AG, Moossa AR. Gastrointestinal hemorrhage from left-sided portal hypertension. An unappreciated complication of pancreatitis. Am J Surg. 1981; 141:153–158.
10. Agarwal AK, Raj Kumar K, Agarwal S, Singh S. Significance of splenic vein thrombosis in chronic pancreatitis. Am J Surg. 2008; 196:149–154.

11. Butler JR, Eckert GJ, Zyromski NJ, Leonardi MJ, Lillemoe KD, Howard TJ. Natural history of pancreatitis-induced splenic vein thrombosis: a systematic review and metaanalysis of its incidence and rate of gastrointestinal bleeding. HPB (Oxford). 2011; 13:839–845.

12. Cohen DL. Electronic clinical challenges and images in GI. Image 1: gastric variceal hemorrhage owing to splenic vein thrombosis in a patient with idiopathic retroperitoneal fibrosis. Gastroenterology. 2008; 135:e1–e2.
13. Makowiec F, Riediger H, Emmrich J, Kröger J, Hopt UT, Adam U. Prophylactic splenectomy for splenic vein thrombosis in patients undergoing resection for chronic pancreatitis. Zentralbl Chir. 2004; 129:191–195.

14. Zadrozny D. Left-side portal hypertension as a clinical problem. Wiad Lek. 1999; 52:494–499.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download