Abstract
Objective
Low cholesterol is associated with depression among western countries. The objective of this study was to examine the relationship between cholesterol and depression in Korean population with low levels of serum cholesterol.
Methods
The data of about 740,000 individuals, aged 30-64 years at entry in the Korean Cancer Prevention Study, were used. Total cholesterol levels were measured in 1992. Depression was measured using the modified DSM-IV (Diagnostic Criteria of Major Depressive Episode in Diagnostic and Statistical Manual of Mental Disorders-IV) scale. Total cholesterol was classified into four groups (quartile). Odds Ratios of low level of cholesterol were evaluated using multi-variable logistic models.
Results
The prevalence of major depression was 7.7% in men and 10.4% in women. After adjustment for various confounding variables, an inverse association was detected between cholesterol levels and depression intensity among men and women. The odds ratio (95% confidence interval) of the lowest quartile of cholesterol was 1.16 (1.13-1.20) on major depression compared with the highest quartile of cholesterol in men. The corresponding odds ratio among women was 1.09 (1.04-1.15). The strongest association among 9 items of depression was found at "decreased appetite and lost weight" in both men (OR=1.68) and women (OR=1.43).
Figures and Tables
Table 1
Translated version of the depression questionnaire‡ utilized in the Korean Cancer Prevention Study

Table 3
Odds Ratios for association between total cholesterol and subgroup according to total cholesterol in men
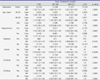
Table 4
Odds Ratios for association between total cholesterol and subgroup according to total cholesterol in women
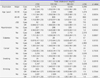
Table 5
Odds Ratios for association between total cholesterol and questions of depression
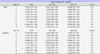
1. I feel depressed with no particular reason.
2. I have lost interest, pleasure, and sexual desire in daily life.
3. I have decreased appetite and lost weight.
4. I have difficulty getting to sleep or staying asleep.
5. I feel agitated and restless.
6. Recently, there are times when I feel very tired without any particular reason.
7. I feel worthless or excessively guilty.
8. My memory is declining and I have difficulty concentrating.
9. I occasionally have thoughts about suicide.SD: standard deviation.
References
1. World Health Organization (CH). Depression [Internet]. Geneva: World Health Organization;2012. cited 2013 Jun. 1. Available from: http://www.who.int/mental_health/management/depression/who_paper_depression_wfmh_2012.pdf.

2. Chang HY, Shin YJ, Batty GD, Son DK, Yun YD, Jee SH, et al. Measuring depression in South Korea: validity and reliability of a brief questionnaire in the Korean Cancer Prevention Study. J Affect Disord. 2013; 150:760–765.

3. Steegmans PH, Fekkes D, Hoes AW, Bak AA, van der Does E, Grobbee DE. Low serum cholesterol concentration and serotonin metabolism in men. BMJ. 1996; 312:221.

4. Steegmans PH, Hoes AW, Bak AA, van der Does E, Grobbee DE. Higher prevalence of depressive symptoms in middle-aged men with low serum cholesterol levels. Psychosom Med. 2000; 62:205–211.

5. Tedders SH, Fokong KD, McKenzie LE, Wesley C, Yu L, Zhang J. Low cholesterol is associated with depression among US household population. J Affect Disord. 2011; 135:115–121.

6. Olié E, Picot MC, Guillaume S, Abbar M, Courtet P. Measurement of total serum cholesterol in the evaluation of suicidal risk. J Affect Disord. 2011; 133:234–238.

7. Hyyppä MT, Kronholm E, Virtanen A, Leino A, Jula A. Does simvastatin affect mood and steroid hormone levels in hypercholesterolemic men? A randomized double-blind trial. Psychoneuroendocrinology. 2003; 28:181–194.

8. Muldoon MF, Manuck SB, Matthews KA. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ. 1990; 301:309–314.

9. Jee SH, Kivimaki M, Kang HC, Park IS, Samet JM, Batty GD. Cardiovascular disease risk factors in relation to suicide mortality in Asia: prospective cohort study of over one million Korean men and women. Eur Heart J. 2011; 32:2773–2780.

10. Cho MJ, Hahm BJ, Kim JK, Park KK, Chung EK, Suh TW, et al. Korean Epidemiologic Catchment Area(KECA) study for psychiatric disorders: prevalence of specific psychiatric disorders. J Korean Neuropsychiatr Assoc. 2004; 43:470–480.

11. Cho MJ, Chang SM, Hahm BJ, Chung IW, Bae A, Lee YM, et al. Prevalence and correlates of major mental disorders among Korean adults : a 2006 National Epidemiologic Survey. J Korean Neuropsychiatr Assoc. 2009; 48:143–152.

12. Park JH, Kim KW. A review of the epidemiology of depression in Korea. J Korean Med Assoc. 2011; 54:362–369.

13. Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013; 34:119–138.

14. Heron DS, Shinitzky M, Hershkowitz M, Samuel D. Lipid fluidity markedly modulates the binding of serotonin to mouse brain membranes. Proc Natl Acad Sci U S A. 1980; 77:7463–7467.

15. Kaplan JR, Shively CA, Fontenot MB, Morgan TM, Howell SM, Manuck SB, et al. Demonstration of an association among dietary cholesterol, central serotonergic activity, and social behavior in monkeys. Psychosom Med. 1994; 56:479–484.

17. Blazer DG, Burchett BB, Fillenbaum GG. APOE epsilon4 and low cholesterol as risks for depression in a biracial elderly community sample. Am J Geriatr Psychiatry. 2002; 10:515–520.

18. Bove M, Carnevali L, Cicero AF, Grandi E, Gaddoni M, Noera G, et al. Psychosocial factors and metabolic parameters: is there any association in elderly people? The Massa Lombarda Project. Aging Ment Health. 2010; 14:801–806.

19. Boscarino JA, Erlich PM, Hoffman SN. Low serum cholesterol and external-cause mortality: potential implications for research and surveillance. J Psychiatr Res. 2009; 43:848–854.

20. Bligh-Glover W, Kolli TN, Shapiro-Kulnane L, Dilley GE, Friedman L, Balraj E, et al. The serotonin transporter in the midbrain of suicide victims with major depression. Biol Psychiatry. 2000; 47:1015–1024.

21. Shin JY, Suls J, Martin R. Are cholesterol and depression inversely related? A meta-analysis of the association between two cardiac risk factors. Ann Behav Med. 2008; 36:33–43.

22. Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: a prospective study of depressed inpatients. Psychiatry Res. 2007; 152:11–20.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download