This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
A pertussis patient from an elementary school, in Gyeonggi Province, Korea, was notified to public health authority on July 25, 2017. Epidemiologic investigation was conducted to identify the magnitude, possible source of infection and risk factors for this outbreak on August 17, 2017.
Materials and Methods
A case was defined as the school student experiencing cough for more than two weeks with or without paroxysmal, whoop, or post-tussive vomiting. Control was defined as the student polymerase chain reaction-negative at the school. School based surveillance was implemented to identify additional cases.
Results
From June 29 to August 27, 2017, nine patients of pertussis were identified from an elementary school. Among nine cases, eight were confirmed by polymerase chain reaction positive. All cases had cough, one (11%) had post-tussive vomiting, and one (11%) had fever. Eight cases had macrolide for 7 days in outpatient clinic, and one case admitted in a hospital. There was no significant difference of demographic factors including gender (p=0.49), age group (p=0.97), number of series of vaccination of pertussis (p=0.52), the number of participation of after school activity (p=0.28), and the time elapsed since last vaccination (p=0.42). However, we found the history of contact within the classroom or after-school activity was only the independent risk factor among all the demographic factors collected (odds ratio, 63.61; 95% confidence interval, 4.35 to 930.79).
Conclusion
The contributing factor for transmission is associated with the case-contact. Immediate identification of pertussis with use of appropriate diagnostic test may help to avoid a large number of cases.
Go to :

Keywords: Pertussis, Disease outbreaks, Surveillance, Vaccines
Introduction
Pertussis is a vaccine-preventable disease caused by
Bordatella pertussis [
1]. It is usually transmitted by respiratory droplets and the incubation period is between 6 and 20 days [
2].
The symptoms are characterized typically repeated violent coughing and can be followed by inspiratory whoop [
3]. The transmission of pertussis is high at the early stage of the paroxysmal cough, and is gradually decrease onward and required to have five days of treatment with macrolide to loss of infection [
2]. Pertussis vaccination reduces the morbidity and mortality (92% decline in case development and 99% or more declines in deaths in the United States) of pertussis [
4]. Furthermore, a vaccinated person tends to have a milder symptom [
3].
Korean children have been recommended having a five-dose series of pertussis vaccine (diphtheria-tetanus-acellular pertussis; diphtheria, tetanus, acellular pertussis [DTaP] at 2, 4, and 6 months of age, and Tetanus toxoid, reduced diphtheria and acellular pertussis; tetanus, diphtheria, and pertussis [Tdap] at age between 15 and 18 months and at age between 4 and 6 years) [
5]. Despite the high vaccination coverage rate (96.6%) in Korea [
6], the reported number of pertussis cases have been risen from 26 cases in 2013 to 123 cases in 2016 [
7]. The underlying cause of this increase is not well understood; however, the waning immunity after acellular pertussis vaccination in children and adults has been considered one of contributing factors [
38].
Outbreaks of pertussis in highly vaccinated population have been rarely reported in the Republic of Korea; thus, detailed epidemiologic investigation is recommended to identify the associated factors for the transmission of pertussis [
9].
On July 25, 2017, Osan City Department of Public Health in Gyeonggi Province was notified of a laboratory-confirmed pertussis-patient, a student from an elementary school. On July 31, 2017, the second laboratory confirmed pertussis patient from the same classroom where first patient developed were notified. In the following two weeks, two additional school attendees reported laboratory result positive for pertussis. On August 16, an outbreak investigation in the elementary school was conducted to identify the size of the outbreak, identify the associated factors of this transmission, and prevent additional patients developed.
Go to :

Materials and Methods
Ethical approval for this study was not required under the Korean Infectious Disease Control and Prevention Act No. 4 and Enforcement Rule of Bioethics and Safety Act No. 33. An informed consent was obtained from the study participants.
Study area and design
An investigation was carried out in the affected elementary school, which had 855 students and 43 staffs.
A retrospective unmatched case-control study was conducted to identify the risk factors for this outbreak. All parents of students with respiratory illness in the school during the outbreak period were interviewed by telephone using a newly developed questionnaire. The questionnaire sought to capture sex, age, onset date of symptoms, classroom in the school, and the after-school activity in and out of the school. Their vaccination history was abstracted from the national vaccination administration database.
Case definition
A case was defined as an elementary school student experiencing cough for more than two weeks with or without paroxysms, whoop, or post-tussive vomiting between June 9, 2017 (3 weeks before the onset date of symptom from the index patient) and November 1, 2017 (9 weeks after the symptom of the last patient notified). Cases were further classified as confirmed by laboratory testing (detection of
Bordetella pertussis by polymerase chain reaction [PCR] and/or isolation of
B. pertussis by culture) according to the guideline from the Korea Centers for Disease Control and Prevention [
10]. Controls were defined as the PCR-negative students at the same school during the outbreak period.
School- and community-based surveillance
On August 17, active surveillance was implemented in the school to identify additional cases through the class teacher encouraging any student having cough illness contact the physicians in the community. Furthermore, the physicians in the community were informed to sample and transport specimens to the provincial public health laboratory to identify B. pertussis if any student had respiratory symptoms. Nasopharyngeal swabs were performed by the physicians using Dacron swab.
Laboratory analysis
Fifty collected samples were evaluated at a provincial public health laboratory. PCR was used for laboratory confirmation of pathogens. PCR testing targeted genes coding for an insertion element (IS481) and for pertussis toxin promoter [
11].
Furthermore, human specimens were inoculated on Regan-Lowe (Charcoal horse blood) agar plates containing cephalexin. The plates were incubated at 37℃ and checked daily for up to 7 days for the presence of typical colonies [
11].
Statistical analysis
Data are expressed as proportions for categorical variables. We used Fisher's exact test to examine the differences of demographic factors between cases and PCR-negative controls. Logistic regression was conducted to estimate the association of pertussis with demographic factors collected.
All analyses were carried out using Epi Info ver. 7.2.1.0 (Centers for Disease Control and Prevention, Atlanta, GA, USA), and SPSS software ver. 18.0 (SPSS Inc., Chicago, IL, USA). A p-value less than 0.05, was considered as statistically significant for all statistical analyses.
Go to :

Results
Descriptive epidemiology
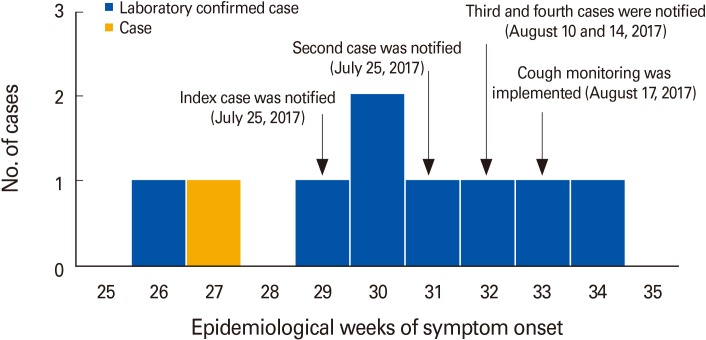
The index patient was presented paroxysmal cough from June 29, 2017, and diagnosed on July 25, 2017 during hospitalization. The infection source of index case was not identified. By August 16, 2017, six additional cases were identified with the attack rates of pertussis at this elementary school (0.8%; seven cases of total 852 students at the school). After implementation of school- and community-based surveillance (August 17, 2017), 50 collected samples were evaluated at a provincial public health laboratory and two cases were identified. After August 27, 2017 no additional cases were detected (
Fig. 1). Among the nine cases, eight were confirmed by PCR positive. The number of case from first year grade was one (11.1%), second year grade was four (44.4%) and fourth year grade was four (44.4%). The most affected classroom was third of second grade where the index case was identified; three additional cases were developed at the very beginning phase of pertussis outbreak and the cases were geographically close each other in the classroom. Cases had shared their desk each other which was located second and third rows in the classroom. The mean age of case was 8.6 (range, 7.0 to 10.0). Three (33.3%) of the cases were male and 26 (66.7%) of cases were female. All cases were had five-dose series of pertussis vaccination. Five (55.6%) of cases had after-school activities at a school. The mean time elapsed since last vaccination was 4.4 years (range, 2.9 to 6.0 years). Of the nine cases, all (100%) had cough, one (11%) had post-tussive vomiting, and one (11%) had fever. Eight cases had macrolide for seven days in outpatient clinic, and one case had an inpatient department.
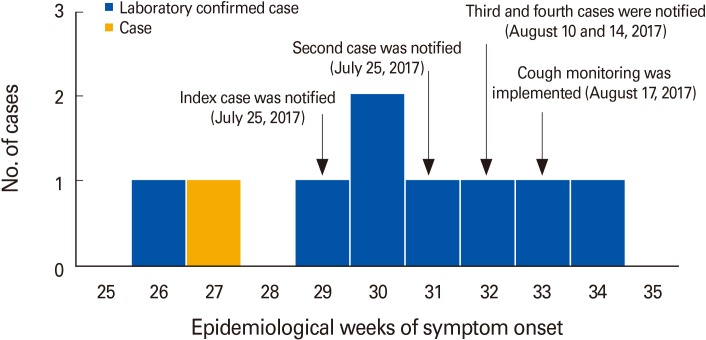 | Fig. 1The number of pertussis case patients during an outbreak in an elementary school: Osan City, Gyeonggi Province, Republic of Korea by epidemiologic weeks of the onset date of symptom from 26 of 2017 to 34 of 2017 and the date of case-notification from physicians.
|
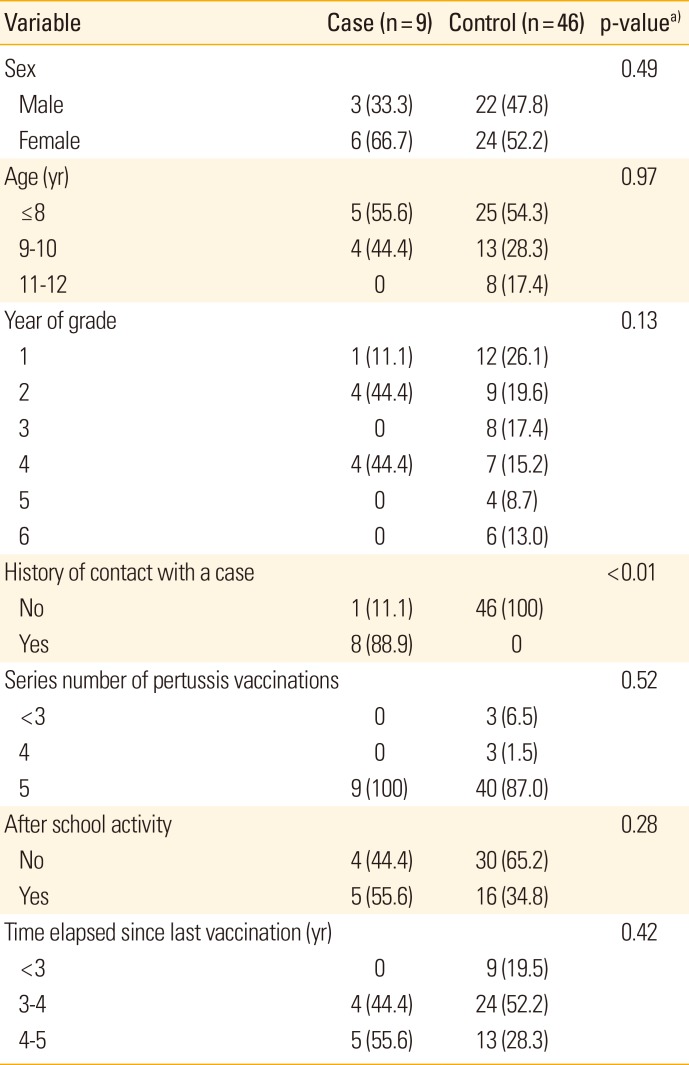
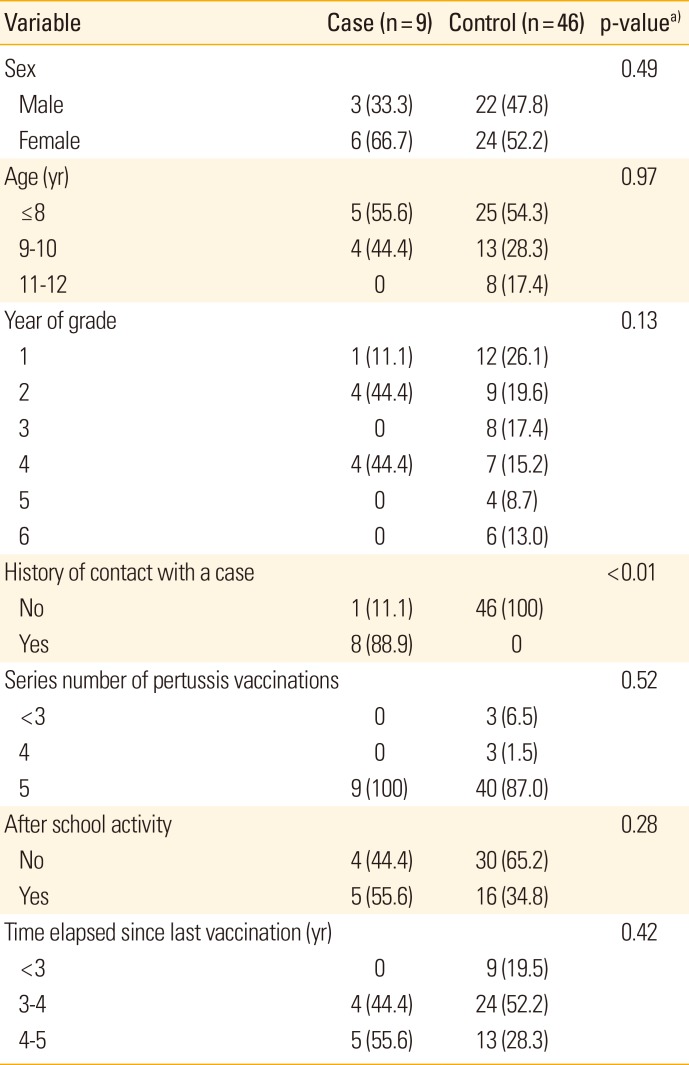
Analytical epidemiology
There were no significant differences between cases and controls by gender (p=0.49), age group (p=0.97), number of series of vaccination of pertussis (p=0.52), the number of participation of the school activity (p=0.28), and the time elapsed since last vaccination (p=0.42) (
Table 1). However, the history of contact with same classroom or same after-school activity was significantly different between cases and controls (p<0.01).
Table 1
Characteristics of cases (n=9) and controls (n=46) associated with an outbreak of pertussis in an elementary school, June 29, 2017 to August 27, 2017
|
Variable |
Case (n=9) |
Control (n=46) |
p-valuea)
|
|
Sex |
|
|
0.49 |
|
Male |
3 (33.3) |
22 (47.8) |
|
Female |
6 (66.7) |
24 (52.2) |
|
Age (yr) |
|
|
0.97 |
|
≤8 |
5 (55.6) |
25 (54.3) |
|
9–10 |
4 (44.4) |
13 (28.3) |
|
11–12 |
0 |
8 (17.4) |
|
Year of grade |
|
|
0.13 |
|
1 |
1 (11.1) |
12 (26.1) |
|
2 |
4 (44.4) |
9 (19.6) |
|
3 |
0 |
8 (17.4) |
|
4 |
4 (44.4) |
7 (15.2) |
|
5 |
0 |
4 (8.7) |
|
6 |
0 |
6 (13.0) |
|
History of contact with a case |
|
|
<0.01 |
|
No |
1 (11.1) |
46 (100) |
|
Yes |
8 (88.9) |
0 |
|
Series number of pertussis vaccinations |
|
|
0.52 |
|
<3 |
0 |
3 (6.5) |
|
4 |
0 |
3 (1.5) |
|
5 |
9 (100) |
40 (87.0) |
|
After school activity |
|
|
0.28 |
|
No |
4 (44.4) |
30 (65.2) |
|
Yes |
5 (55.6) |
16 (34.8) |
|
Time elapsed since last vaccination (yr) |
|
|
0.42 |
|
<3 |
0 |
9 (19.5) |
|
3–4 |
4 (44.4) |
24 (52.2) |
|
4–5 |
5 (55.6) |
13 (28.3) |

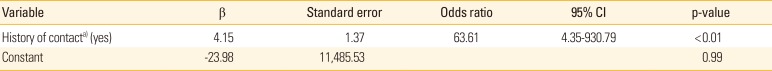
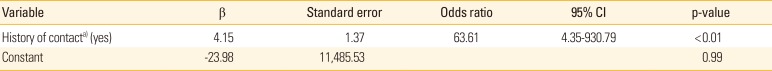
From bivariate logistic regression analysis, which model has 75% of predicted value, the history of contact within the classroom or after-school activity was only the independent risk factor for pertussis infection (odds ratio, 63.3; 95% confidence interval, 4.4 to 930.8; p<0.01) among other demographic factors (
Table 2).
Table 2
Bivariate logistic regression analysis of risk factor for pertussis infection in an elementary school
|
Variable |
β |
Standard error |
Odds ratio |
95% CI |
p-value |
|
History of contacta) (yes) |
4.15 |
1.37 |
63.61 |
4.35–930.79 |
< 0.01 |
|
Constant |
−23.98 |
11,485.53 |
|
|
0.99 |

Control measures
To control the spread of the disease, several measures were taken. All the cases excluded from the school and extracurricular activities until the completion of antibiotic treatment. All the household of cases asked to have prophylactic antibiotic treatment (Macrolide for 5 days).
To identify additional cases promptly, city department of public health set the daily cough monitoring in the school and community. At the first week of the implementation of active search, 10 students (1.2% of total students in the school) were evaluated. In the following weeks, the number of students for cough illness declined from 30 students on second week to two students on third week. The students with respiratory symptoms were asked to wear a mask until they were confirmed as PCR negative by the laboratory test. The elementary school was asked not to organize after-school activities, field trip and athletic events during the outbreak period.
Furthermore, all students in the school were recommended strict personal hygiene including frequent hand-washing and avoiding any contact with the sick person.
Go to :

Discussion
This study demonstrated that pertussis outbreaks could develop among highly vaccinated population in elementary school. Despite the vaccination coverage is quite high, we found immediate identification with appropriate control measure is critical to limit spread of pertussis.
The attack rates of pertussis at this elementary school (1%) were lower than other previous outbreaks in elementary schools (range, 5% to 75%) [
1213]. The vaccination coverage in this school was more than 95% with complete scheduled pertussis vaccinations (five-dose series, 95.8%; 4-dose series, 100%). The lower attack rate in this outbreak is highly likely due to the high coverage rate of five-dose series of pertussis vaccination which has similar finding with previous report of the low risk of pertussis-transmission among the highly-vaccinated students in an elementary school [
9]. Thus, most of the cases in this outbreak have a mild symptom such as cough without inspiratory whoop, which has consistent finding of a previous study that the pertussis vaccination has a positive effect to reduce the risk of severe progress [
14]. However, pertussis vaccination does not prevent all pertussis cases [
15]; although the vaccination is also likely to affect the substantial reduction in the rate at which pertussis is transmitted to other students.
All cases have scheduled pertussis vaccinations, and there's no statistically significant difference in the time elapsed since last vaccination (p=0.28). This finding is consistent with previous literature which showed that the waning of vaccine-induced immunity was not likely a contributing factor of infection [
9]. In addition, we found the presence of pertussis infected person in a classroom or in an after-school activity is a significant contributing factor which is consistent with previous study which showed transmission of pertussis was associated with cases [
916].
There was a case who had persistent two more weeks with misdiagnosis as a common cold. This is similar situation in United States due to the wide spectrum of symptoms due to the vaccination [
17]. Thus, the primary care physicians should consider the laboratory test and diagnosis of pertussis to rule out pertussis for those having persistent cough.
School based surveillance is considerable control measure for on-going outbreak in school based setting. In this outbreak, public health and school officials implemented a proactive control strategy such as putting a facial mask of any cough student from school with recommendation of laboratory investigation for active search of additional cases.
There are some limitations of this study. First, the source of infection was not identified, because of the primary case could not remember the place and the person met extraordinarily. However, the source of infection could have been a casual contact from the community which is consistent finding with a previous study [
18]. Second, due to the low incidence of pertussis in this outbreak, the small number of cases was included. This may the confidence intervals for the odds ratios be wide. Third, owing to use a PCR-negative control, our result may be underestimated. Furthermore, there may also have false-negative samples by inappropriate swab method. Fourth, we did not evaluate the DNA comparison to identify the same pathogen. Due to the low culture rate of
B. pertussis, particularly the vaccinated person, we only identify the growth from a single specimen among 50 samples collected. However, regarding the sensitivity of bacterial culture is lower (58%) than PCR (97%) [
19], and the epidemiologic link with consecutive time line among cases and no additional case reported in the region during this outbreak, it is highly likely infected with same pathogen.
This study describes a pertussis outbreak in an elementary school in Gyeonggi Province, the Republic of Korea. The only association factor for transmission is associated with the case-contact. Continued education for the immediate identification of pertussis with use of appropriate diagnostic test from primary physician may help to prevent further outbreaks in a community setting.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download