Abstract
Purpose
Mumps vaccine has not been included in the routine national immunization program in Japan, leading to low vaccine coverage rates and periodic epidemics approximately every 5 years. Our hospital (a secondary community hospital in Japan) experienced an increased number of mumps-related complications with a nationwide epidemic in 2016. Using previously reported data and mumps-related cases in our hospital, we estimated the cost-effectiveness of routine mumps vaccination in Japan with a static model using current epidemiologic data.
Materials and Methods
With a decision tree flowchart of mumps infection and adverse events, we estimated the burden of mumps-related complications in our hospital for 5 years, and calculated the current annual national burden. Finally, we compared the current burden and assumptive burden of the stable state after routine vaccination in Japan using a static model.
Mumps vaccine was included in the national immunization programs (NIPs) of 121 countries as of late 2015 [1]. Countries where routine mumps vaccination has not yet started are some African countries, South Asian countries, and Japan. In Japan, routine vaccination was stopped in 1993 because vaccine-induced aseptic meningitis provoked a social problem. Thereafter, vaccine coverage has been 30%–40% due to voluntary inoculations. Because of the low coverage rate in Japan, there are 400,000 to 1.5 million mumps patients in Japan, and there was another nationwide epidemic in 2016 [2]. Complications occur at the following rates: aseptic meningitis 1%–10%, encephalitis 0.03%–0.2%, hearing loss 0.1%, orchitis 25% in adult men, and oophoritis 5% in adult women [3].
We reviewed mumps-related complication cases over 5 years in our hospital (a 430-bed secondary hospital in Nara Prefecture, Japan) and the cost-effectiveness of routine vaccination in Japan using a static model.
We created a decision tree flowchart of mumps infection and adverse events due to vaccination (Fig. 1). We estimated the burden of mumps-related complications using current available data and cases in our hospital for 5 years, and then we computed the current annual national burden. Finally, we compared the current burden and assumptive burden of the stable state after routine vaccination in Japan using a static model. All of the calculations were performed by the methods described as follows with Microsoft Excel 2016 (Redmond, WA, USA).
We reviewed the electronic medical records of Nara Prefecture General Medical Center, Japan (a 430-bed secondary hospital in Nara Prefecture) and calculated the burden of all mumps related complication cases from January 1, 2012, to December 31, 2016. All mumps-related complication cases in our hospital were diagnosed with serological confirmation. Medical costs included the outpatient and inpatient costs of the hospital for mumps complications. We confirmed that no cases with mumps-related complications had any other medical conditions throughout the periods of cost calculation. Social cost was estimated by (recuperation period)×(average adult female wage) in pediatric cases and (recuperation period)×(average adult wage by sex) in adult cases because a patient's parent must care for his or her children with taking off from work in most pediatric cases, and patients themselves must take off work in adult cases. The recuperation period was the duration from the date of the patient's first day of absence until the day before the doctor's permission to return to work or school. Overall, male and female hourly wages were estimated as 2,172, 2,496, and 1,667 Japanese Yen (JPY)/hr [4]. Since national surveillance data do not contain information about the patient's age in adult cases or parents' ages in pediatric cases, although they do include pediatric patient ages (6-month intervals before 1 year old, 1-year intervals from 1 to 10 years old, and 5-year intervals from 10 to 20 years old), we did not consider age-specific wages in our calculation [5].
We estimated the total mumps-related burden (medical cost, social cost, and quality-adjusted life years [QALYs] lost) in Japan. Using surveillance data from 2000 to 2016, we calculated the number of annual average symptomatic mumps patients [25]. To estimate the burden of mumps and its related complications, we referred to each preceding study for reports of encephalitis, orchitis, oophoritis, hearing loss, other mumps-related hospitalizations, and outpatient cases [67891011]; however, for meningitis, we used the data from real mumps meningitis cases from our hospital because there were few data available about the burden of mumps meningitis in Japan. For example, Hoshi et al. [12] used data on pneumococcal meningitis as an estimation of the burden of mumps meningitis in a previous study, but these data are not appropriate for the estimation of the burden of mumps meningitis because the clinical courses of mumps meningitis and pneumococcal meningitis are very different [6]. The incidence of mumps meningitis was estimated to be 2.23% of all mumps cases in a previous study [13].
For encephalitis cases, we used 0.05% as the incidence, and a study of pneumococcal meningitis was substituted for the estimation of mumps encephalitis because of a lack of available data nationwide and in our hospital [613]. The recuperation periods per case for social cost calculation were 22.7 and 21.1 days for younger than 3 years old and 3 or older, respectively [6]. In cases with neurological sequelae, the annual medical costs were calculated as 368,350 and 396,929 JPY for younger than 3 years old and 3 or older, respectively, throughout the rest of their lives [6]. Japanese average life expectancy was 80.5 and 86.8 years old in men and women, respectively, in 2016 [14]. According to national surveillance data, 13.7% of mumps cases are estimated to occur in patients younger than 3 years old [5]. We assumed that each patient loses 0.43 QALYs per year [6]. In this section, we used healthy life expectancy instead of life expectancy. Japanese average healthy life expectancy was 71.19 and 74.21 years old in men and women, respectively, in 2013 [15]. Social deficit was calculated as 0.43×(average adult annual wage)×45 years (period of productive age in Japan).
The burdens of orchitis and oophoritis were estimated as 171,732 and 186,905 JPY in medical costs, respectively, 4.9 and 5.3 days in recuperation periods for the calculation of social costs, and 0.01 QALYs loss per case [7].
With respect to hearing loss, we used the studies of Yamanaka et al. [9] and Okubo et al. [10] for unilateral and bilateral hearing loss, respectively, with 0.1 and 0.2 QALY loss in each patient followed by a subsequent social deficit as 0.1×(average adult annual wage by sex)×45 years and 0.2×(average adult annual wage by sex)×45 years. Medical costs were estimated as 79,422 and 4,000,000 JPY for each unilateral and bilateral case, respectively.
Regarding other mumps-related hospitalizations and outpatient cases, we used the study of Sugawara et al. [11] with the results of 233,200 and 10,477 JPY as medical costs, respectively, and 9.5 days and 5.0 days×(adult women daily wage) as social cost, and 0.01 and 0.005 as QALYs loss per case. Five days was the mandatory absence period for all mumps cases.
Using national surveillance data from 2000 to 2016, we calculated that 53.6% of mumps cases were male, and 1.7% were adults. We assumed that these proportions were equal among all complications other than orchitis and oophoritis [5].
In addition, we performed sensitivity analysis for each complication to address the variability of each case's burden, as described later.
Since our study was a static model and we could not simply apply vaccine efficacy to reduce the rate of incidence, we reviewed data from countries comparing incidences before and after the introduction of routine mumps vaccination [316171819]. The study of Galazka et al. [3] showed that countries where two-dose routine vaccination was introduced achieved from 97% to more than 99% reductions in cases comparing before and after routinization, while those with one-dose vaccination had 88 to 98% reductions. For example, Finland achieved more than a 99.9% reduction in cases [16]; however, mumps are endemic in countries with high coverage rates of two-dose vaccinations. We assumed that the number of patients and the burden of the disease would decrease by 98% after a stable state of routine vaccination [19]. We performed sensitivity analysis with a range of a 70%–99.9% reduction in cases.
We expected a 96.2% first dose coverage rate and 92.9% second dose coverage rate once mumps vaccine was included in the NIP with full financial support from the government [20]. These coverage rates were from measles-rubella vaccine coverage in 2015, which was already included the NIP in Japan. We assumed 6,000 JPY for the vaccination cost for each dose. One million people are eligible for vaccination each year. We estimated a 30% first dose coverage rate and a 0% second dose coverage rate in the current state [122122]. In addition, if children received single mumps vaccinations (independent inoculation), we considered the parent's burden to take them to health care facilities to be 0.5 working days lost for each vaccination. If they received mumps vaccine with other vaccines (simultaneous inoculation), we did not consider any further deficits. In the routine vaccination program, we assumed all children to receive a first dose at 1 year old. For rate estimations of each adverse event due to vaccinations, we first referred to a prospective or randomized study for the adverse event. In adverse events without such studies, we referred to a retrospective study. The rate of each adverse event was estimated as follows: fever 6.0% (336/5,603), parotid gland swelling 1.8% (97/5,541), meningitis 0.016% (1/6,443), encephalitis 0.0004%, and hearing loss 0.000017% [212324].
According to nationwide retrospective surveillance reports of suspected adverse events with the mumps vaccine, 3,784,329 vaccines were administered from Apr 1, 2013, to Mar 31, 2016 [25]. Four suspected cases of anaphylaxis were reported (one case of anaphylactic shock and three cases of anaphylactic reactions); however, after reviews by experts, none of these cases were diagnosed as level 3 by the Brighton Collaboration minor and major criteria, and no severe anaphylaxis cases were confirmed. Other suspected adverse events, such as pancreatitis (one case), immune thrombocytopenic purpura (six cases), and Guillain-Barre syndrome (one case), were reported [23]. We did not include these very rare adverse events in our analysis because all of these adverse events also occurred in cases of natural infections without available data regarding the burdens of these rare adverse events and these complications due to natural infections, and considering these conditions in adverse events analysis alone might have prevented accurate estimation.
We assumed that the severity and cost of adverse events were the same as those of natural infections because of a lack of reliable data about the burdens of adverse events. We also supposed that 10% of febrile patients and patients with parotid gland swelling after vaccination would visit outpatient clinics, and the medical and social costs in the cases were the same as in those with natural mumps infection.
Finally, we calculated the cost-benefit ratio and QALY gain using sensitivity analysis. As parameters of sensitivity analysis, we selected vaccine cost (4,000 to 8,000 JPY per dose), vaccine coverage rate (80% and 70% to 99% and 99% for the first and second doses, respectively), reduction rate in patients after routinization (70% to 99.9%), burden of each complication of natural infection (-50% to +50%), and incidence of adverse events after vaccination (-50% to +50%).
Fig. 2 shows the number of mumps-related complications in Nara Prefecture General Medical Center from January 1, 2012, to December 31, 2016, in addition to the estimated overall number of patients in Japan. We could see an increase in complications cases in 2016 (meningitis, eight cases; orchitis, six cases; hearing loss, two cases) because there was a nationwide epidemic in 2016 [5]. The incidence in 2016 was approximately 4 times that in 2013 and 2014.
Table 1 shows the burden of each complication. The costs of orchitis were less than those of hearing loss and meningitis because all of the cases of orchitis in our hospital were treated as outpatients.
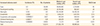
We calculated that the average number of mumps patients from 2000 to 2016 was 907,345, and the average age of patients with mumps infection was calculated as 6.43 years old [5]. The number of patients and age distributions by year are listed in Table 2. The burdens of each complication are estimated in Table 3. The estimated medical cost was 21.6 billion JPY, and the estimated social cost was 63.3 billion JPY per year in addition to 9,487 JPY in annual QALY loss.
After the 98% reduction in patients and burdens of mumps due to routine vaccination, medical costs, social costs, and QALYs lost were estimated as 431 million JPY, 1.27 billion JPY, and 196, respectively.
The incremental budget for routine vaccination is 9.55 billion JPY from a social perspective and 11.35 billion JPY from the payer's perspective. The estimated incidence and burden of each adverse event are calculated in Table 4. Incremental medical costs, social costs, and QALYs lost due to routine vaccination were 271 million JPY, 890 million JPY, and 132, respectively, per year.
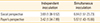
Table 5 showed that the cost-benefit ratios were 3.69/6.84 with independent/simultaneous inoculation from a social perspective and 3.42/5.97 from the payer's perspective. Considering the worst and best scenarios with all of the parameters in sensitivity analysis (vaccine cost, vaccine coverage rate, reduction rate of patients after routinization, burden of each complication of natural infection, and incidence rates of adverse events after vaccination), each cost benefit was 3.69 (1.08–9.52)/6.84 (1.51–23.73) with independent/simultaneous inoculation from a social perspective, and 3.42 (1.04–7.89)/5.97 (1.43–15.66) from the payer's perspective. Moreover, an annual QALY gain of 9,487 (3,227–14,659) was expected if a stable status of routine vaccination was achieved. The ranges were the results when all of the parameters of sensitivity analysis were vaccine-unfavorable values and when all of them were vaccine favorable values. Sensitivity analysis revealed that the burden of each complication and the reduction in mumps patient were factors vulnerable to the cost-benefit ratio (Fig. 3). Even in the worst scenario with all of the parameters in sensitivity analysis, the cost-benefit ratio was greater than 1.
This study proposed additional evidence using a static model that Japan must start routine mumps vaccination urgently, considering the current enormous burden of the disease that we calculated in this study. There have been studies that showed the cost-effectiveness of mumps routine vaccination [11122526]. The cost-benefit ratio of independent inoculation from a social perspective in our study was 3.69. This number indicated that routine mumps vaccine would be highly cost-effective compared to other vaccines, such as Rota vaccine. The cost-benefit ratio of Rota vaccine in Japan is 0.95 [27].
The characteristics of this study were a medical cost estimation based on real mumps meningitis cases, proof of an enormous QALY gain in addition to a high cost-benefit ratio, reasonable vaccination coverage rates, and considering the incidence rates of adverse events based on domestic studies [2123]. The former Japanese study estimated that the routine vaccine coverage rates were 76.0% (first dose) and 72.7% (second dose), respectively [13]; however, we believe that the coverage rates for mumps vaccine should be equal to those of other vaccines in the NIP once the Japanese government includes mumps vaccine in the NIP.
Regarding the cases in our hospital, we experienced a sharp increase in mumps-related complications in 2016. Although we believe that the increase in mumps meningitis in our hospital in 2016 was mainly due to the nationwide epidemic, it might indicate the possibility of missed diagnoses in the non-epidemic season rather than an anchoring error of doctors in the epidemic season because all of the mumps-related cases in our hospital were serologically confirmed. The burden of cases in our hospital was different from that in previous studies. For example, the medical cost of unilateral hearing loss was much higher in our cases than in preceding studies. Conversely, the medical cost of orchitis in our hospital was less than that of national reports because all of the orchitis patients were followed up as outpatients in our hospital. We used previous reports in our cost-effective analysis because of the larger sample size; however, we chose to use our cases to estimate the burden of mumps meningitis since the preceding study was derived from a group with poor prognosis in the estimation of mumps meningitis, which usually has an excellent prognosis [6].
There were several limitations of our study. First, this study used a static model without herd immunity considerations. Due to a lack of herd immunity consideration, the estimation of the reduction in the number of patients after routinization was unclear. Ideally, vaccine efficacy should be considered in a simulation study. The efficacy of vaccination for mumps is different between vaccine strains. In Japan, the Hoshino and Torii strains are widely used. These strains are considered to have better vaccine efficacy with more frequent adverse events than those for the Jeryl-Lynn strain [2128]. According to the study by Ihara and Ochiai [18], the efficacy of one-dose vaccination for Japanese domestic strains was approximately 78.1%–90.0%. Unfortunately, there are no data on the efficacy of 2 doses vaccination for Japanese domestic strains since few people in Japan receive two-dose vaccinations. A lack of consideration for vaccine efficacy and herd immunity was the greater limitation of our study. Second, a more accurate estimation of mumps meningitis is needed since our estimation was based on data from only one facility and a small sample size. Third, we considered only major mumps-related complications and adverse events. Considering very rare events would be better for thorough estimation, but it was difficult to perform precisely due to a lack of detailed data about these minor events.
Other factors which might have affected our results are as follows. First, although we assumed that the severity and burden of adverse events due to vaccination were the same as those with natural mumps infections, we could infer that vaccine-induced mumps complications are less severe. Considering that assumption would have rendered our results more vaccine-favorable, it was difficult to precisely estimate due to a lack of reliable data. Second, we calculated only adult orchitis and oophoritis in the study with a lack of sufficient data on adolescent complications, considering that adolescent orchitis and oophoritis can result in more vaccine-favorable outcomes. Third, we did not include transportation costs in our estimations, which might have slightly affected our results.
Finally, the wide gap in the cost benefit ratio between simultaneous inoculation and independent inoculation was confirmed in our study due to the burden of mothers taking their children to health care facilities for vaccination. Since simultaneous inoculation is widely accepted worldwide, we recommend that mumps vaccination be administered with other vaccinations to decrease the burdens of caregivers.
In conclusion, this study showed that routine mumps vaccination is cost-effective and QALY saving, but simulation with a dynamic transmission model and herd immunity analysis are needed for more accurate simulations.
Figures and Tables
 | Fig. 2Mumps-related complication cases in Nara Prefecture General Medical Center (2012-2016) and estimated overall number of patients in Japan. The overall number of patients in Japan was estimated using Japanese epidemiologic data. |
 | Fig. 3Sensitivity analysis. The figure plots worst and best scenarios for each parameter of vaccine cost (4,000 to 8,000 per dose), vaccine coverage rate (80%, 70% to 99%, and 99% for first and second doses, respectively), reduction rate of patients after routinization (70% to 99.9%), burden of each complication of natural infection (-50% to +50%), and incidence of adverse events after vaccination (-50% to +50%). JPY, Japanese Yen. |
Table 1
Burdens of each complication in Nara Prefecture General Medical Center (2012–2016)
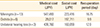
| Medical cost (JPY) | Social cost (JPY) | Recuperation period (day) | |
|---|---|---|---|
| Meningitis (n = 13) | 547,493 | 223,416 | 16.75 |
| Orchitis (n = 6) | 29,017 | 197,711 | 9.9 |
| Unilateral hearing loss (n = 3) | 439,760 | 160,059 | 12.0 |
Table 2
The number of mumps patients in Japan and age distribution by year from 2000 to 2016
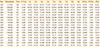
Table 3
Incidence and burdens of each complication estimated

Table 4
Increased adverse event due to routine vaccination
References
1. World Health Organization. Media Center: immunization coverage [Internet]. Geneva: World Health Organization;2017. cited 2017 Feb 27. Available from: http://www.who.int/mediacentre/factsheets/fs378/en/.
2. Hashimoto S, Kawado M, Murakami Y, et al. Incidence of infectious diseases estimated by the surveillance data in 2002-2004 in Japan. Nihon Koshu Eisei Zasshi. 2006; 53:794–799.
3. Galazka AM, Robertson SE, Kraigher A. Mumps and mumps vaccine: a global review. Bull World Health Organ. 1999; 77:3–14.
4. Japanese Ministry of Health, Labour and Welfare. Monthly labour survey, e-stat annual survey, 2015. Tokyo: Japanese Ministry of Health, Labour and Welfare;2015.
5. National Institute of Infectious Diseases. Infectious disease surveillance annual report [Internet]. Tokyo: National Institute of Infectious Disease, Japan;2017. cited 2017 Feb 27. Available from: http://www.nih.go.jp/niid/ja/allarticles/surveillance/2085-idwr/ydata/6555-ydata2015.html.
6. Iwata S, Ishiwada N, Sakata H, Sakano T, Sato Y, Nakano T. Burden of illness of bacterial meningitis and bacteremia caused by Streptococcus pneumonia in children. Jpn J Pediatr. 2008; 61:2206–2220.
7. Japanese Ministry of Health, Labour and Welfare. Survey on the trend of medical care expenditures. Tokyo: Health Insurance Bureau of Medical Economics Division, Japanese Ministry of Health, Labour and Welfare;2010.
8. Hashimoto H, Fujioka M, Kinumaki H. Kinki Ambulatory Pediatrics Study Group. An office-based prospective study of deafness in mumps. Pediatr Infect Dis J. 2009; 28:173–175.

9. Yamanaka N, Hotomi M, Sugata R. Cost-effectiveness of pneumococcal conjugate vaccine in Japan: estimation on acute otitis media in children. Jpn J Pediatr. 2008; 61:2221–2232.
10. Okubo S, Takahashi M, Kai I. How Japanese parents of deaf children arrive at decisions regarding pediatric cochlear implantation surgery: a qualitative study. Soc Sci Med. 2008; 66:2436–2447.

11. Sugawara T, Ohkusa Y, Taya K, et al. Cost-effectiveness analysis of routine mumps immunization in Japan. Kansenshogaku Zasshi. 2007; 81:555–561.

12. Hoshi SL, Kondo M, Okubo I. Economic evaluation of vaccination programme of mumps vaccine to the birth cohort in Japan. Vaccine. 2014; 32:4189–4197.

13. Hosaka S, Komori K, Hoshina K, et al. Investigation about serious cases caused by mumps virus and varicella-zoster virus. J Jpn Pediatr Assoc. 2012; 33:182–186.
14. World Health Organization. Global Health Observatory data, world health statistics. Geneva: World Health Organization;2016.
15. Hashimoto S. Study for healthy life expectancy, healthy Japan 21st century, review of healthy life expectancy. Research Report of Scientific Research Grant from Japanese Ministry of Health, Labour and Welfare [Internet]. Tokyo: Japanese Ministry of Health, Labour and Welfare;2015. cited 2017 Feb 27. Available from: http://www.pbhealth.med.tohoku.ac.jp/japan21/pdf/o-27-3.pdf.
16. Peltola H, Jokinen S, Paunio M, Hovi T, Davidkin I. Measles, mumps, and rubella in Finland: 25 years of a nationwide elimination programme. Lancet Infect Dis. 2008; 8:796–803.

17. Japanese Ministry of Health, Labour and Welfare. Eligible population, the way of inoculation, and choice of vaccine strain for mumps vaccination [Internet]. Tokyo: Health Service Bureau, Division of Tuberculosis and Infectious Disease Control, Japanese Ministry of Health, Labour, and Welfare;2013. cited 2017 Feb 27. Available from: http://www.mhlw.go.jp/stf/shingi/2r985200000371fc-att/2r985200000371w4.pdf.
18. Ihara T, Ochiai H. Mumps vaccine: progress toward the routine vaccination. Rinsyou Uirusu. 2014; 42:174–182.
19. Pickering LK, Baker CJ, Kimberlin DW, Long SS. Red Book. 2012 Report of the Committee on Infectious Diseases. 29th ed. Elk Grove Village, IL: American Academy of Pediatrics;2012. p. 1–109.
20. Japanese Ministry of Health, Labour and Welfare. Measles and rubella immunization situation from 01/04/2015 to 31/03/2016 [Internet]. Tokyo: Japanese Ministry of Health, Labour and Welfare;2016. cited 2017 Feb 27. Available from: http://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou21/dl/160923-01.pdf.
21. Ihara T. Mumps vaccine effectiveness and adverse events: the need for 2-dose vaccination. Nihon Syounikai Kaihou. 2015; 49:55–60.
22. Baba K, Okuno Y, Tanaka-Taya K, Okabe N. Immunization coverage and natural infection rates of vaccine-preventable diseases among children by questionnaire survey in 2005 in Japan. Vaccine. 2011; 29:3089–3092.

23. Muta H, Nagai T, Ito Y, Ihara T, Nakayama T. Effect of age on the incidence of aseptic meningitis following immunization with monovalent mumps vaccine. Vaccine. 2015; 33:6049–6053.

24. Nishimura N. Mumps vaccine. Gendaiigaku. 2010; 58:175–180.
25. Japanese Ministry of Health, Labour and Welfare. Suspected adverse events report of dried weakly activated mumps vaccine [Internet]. Tokyo: Immunization and Vaccine Subcommittee Adverse Events Working Group, Health Sciences Council, Japanese Ministry of Health, Labour and Welfare;2016. cited 2017 Feb 27. Available from: http://www.mhlw.go.jp/file/05-Shingikai-10601000-Daijinkanboukouseikagakuka-Kouseikagakuka/0000144126.pdf.
26. Wiedermann G, Ambrosch F. Costs and benefits of measles and mumps immunization in Austria. Bull World Health Organ. 1979; 57:625–629.
27. Nakagomi T, Nakagomi O. Cost-effectiveness of rotavirus vaccination using direct non-medical costs and opportunity costs estimated from the Internet survey data. Rinsyou Uirusu. 2013; 41:239–250.
28. Rubin SA, Plotkin SA. Mumps vaccine. In : Plotkin SA, Orenstein WA, Offit PA, editors. Vaccines. 6th ed. Philadelphia, PA: Saunders;2013. p. 419–446.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download