Abstract
South Korea and Taiwan have had similar experiences of economic development in the post-war era. The two societies have also successfully overcome the threat of liver cancer by using mass hepatitis B vaccinations. However, to reach their current states, they followed different directions, and experienced differing effects on their national health governance systems. In South Korea, vaccine production occurred prior to effectively introducing immunization programs. In contrast, Taiwan established an effective immunization program first. However, industrialization of vaccines against hepatitis B has failed. Taiwan has to import vaccines for domestic use. This article provides a contextual overview on the different methods South Korea and Taiwan have used to arrive at their modern status of hepatitis B immunization.
South Korea and Taiwan are among the leading countries using vaccines against hepatitis B. They have launched mass immunization programs in the early 1980s, years before the World Health Assembly (WHA) began recommending that member states integrate this vaccine into their national immunization programs in 1992. Moreover, the results of using this vaccine were beneficial in both South Korea and Taiwan in a manner different from that of certain advanced countries, such as France. In France, although the hepatitis B vaccine was included in the general immunization campaign shortly after the recommendation of the WHA, and became a free school-based vaccination program, confidence toward the vaccine decreased due to weaknesses in planning, monitoring and evaluation process of the program [1]. This did not occur in South Korea and Taiwan. Hepatitis B vaccinations can be regarded as successful stories for these two societies.
South Korea and Taiwan have different approaches to providing immunizations against hepatitis B, although they have similar economic and social contexts. This article reviews the route each country took to social awareness of hepatitis B, strategies for mass immunization, and the current status of vaccine usage in South Korea and Taiwan. First, we review the commonalities between South Korea and Taiwan. Their different paths are then described with consideration to their specific initial conditions, the characteristics of the decision makers, different vaccination strategies, the industrialization of vaccines, and the outcomes.
The 'Taiwan Miracle' and 'Miracle on the Han River' are often used to express the rapid economic growth in Taiwan and South Korea, respectively, from the mid-1960s to the 1990s. As shown in Fig. 1, the gross domestic product (GDP) per capita in Taiwan and South Korea increased rapidly from under US$1,000 in the 1970s to over US$15,000 in the 2000s. This phenomenon was explained by the concept of the "developmental state," which emphasizes effective economic planning led by the government. From this perspective, similar trends for South Korea and Taiwan, as shown from left to right in Fig. 1, are interpreted as the results of governmental intervention.
Fig. 1 also shows that, despite their economic performances, Taiwan and South Korea have successfully improved the quality of life of the population. The life expectancy at birth in both Taiwan and South Korea has extended from approximately 60 years in the early 1970s to approximately 80 years in the 2000s. The rapid increase in life expectancy is an outcome of the governance of life, or 'governmentality,' which is defined as the government's effective actions at the population level to preserving the human resources that are required for economic development. For example, prevention of liver cancer was considered effective in increasing life expectancy [2]. The trends of governmentality are similar in South Korea and Taiwan.
South Korea and Taiwan have another hidden common factor that is not shown in Fig. 1: The science and technology that helped latecomers such as South Korea and Taiwan to realize economic growth as well as health improvements. For example, vaccinations are among the technological tools that are recognized as most effective in preventing diseases and improving public health. However, neither South Korea nor Taiwan has a tradition of developing new vaccines. For these two countries, most knowledge and technology regarding vaccines and vaccinations have been introduced by other advanced countries.
Although South Korea and Taiwan exhibit similar trends, as shown in Fig. 1, their paths have not been identical. As the figure shows, between 1980 and 2000 they appeared to be in competition because their graphs often intersect. Since the mid-2000s, South Korea has continued to grow, leaving Taiwan behind. Hepatitis B immunizations occurred in the period of competition from 1980 to 2000. However, their common backgrounds are not determinants for their different paths. The graphs imply that different approaches were used to adopt vaccines in South Korea and Taiwan (Table 1), where certain important events about hepatitis B vaccines and vaccination took place.
The divergent paths of hepatitis B immunizations in South Korea and Taiwan began from different initial conditions in the late 1970s. The initial conditions included their styles of hepatological research, political contexts, and economic development strategies.
Hepatitis was among the most severe diseases occurring in the East Asian region, where Taiwan and South Korea are located. Hepatological research had been a vital subject of Taiwanese and South Korean medical researchers for a lengthy period. Some of the most influential physicians in the medical communities are hepatitis experts, such as Juei-low Sung and Ding-Hsing Chen in Taiwan and Chung-Yong Kim in South Korea. These domestic medical professionals were influenced by their early experiences under Japanese colonization, and were offered opportunities to join certain United States-based research; that is, these physicians were not isolated from the world; rather, compared with other professionals, they had more contact with leading research worldwide because of their scientific cooperation with prestigious research centers in the United States, Western Europe, and Japan.
However, the medical professionals in South Korea and Taiwan have had different interests in hepatological research. Pathological and epidemiological research between the hepatitis viruses and liver diseases was more possible in Taiwan. Taiwanese medical professionals preferred using existing vaccines to developing vaccines of their own. However, South Korean physicians seemed to be more interested in vaccine development. For example, Dr. Chung-Yong Kim, a South Korean expert of hepatological studies, developed a method of hepatitis B antigen purification in the early 1970s [3]. He also assisted the Green Cross to develop plasma-derived vaccines in the early 1980s.
Political situations in the late 1970s and early 1980s were critical factors that affected governmental decision making on hepatitis B prevention. Former South Korean President Chung-hee Park adopted the Yushin Constitution and began the Fourth Republic in 1972, which was an authoritarian regime in which the president held the ultimate power of the state. President Park was assassinated in 1979. Political disorder followed, and in 1980, the Gwangju massacre occurred. The political regime transitioned into the Fifth Republic when Doo-hwan Chun came into power in 1981. The period from the Fourth Republic to the mid-1980s was described as the darkest period of democratization in South Korea.
The political situation in Taiwan was opposite that of South Korea. The Fifth Republic of South Korea was controlled by the military from the end of the 1970s. However, in Taiwan, Chiang Ching-Kuo, the son of Chiang Kai-shek, began gaining political power since the mid-1970s, and became the president of Taiwan in 1978. He was the premier of Taiwan between 1972 and 1978. During his term as premier, his father Chiang Kai-shek died, in 1975. He was reelected president in 1984, and died in 1988. In contrast to his father, Chiang Ching-Kuo had no military background. During his terms as premier and president, he named several technocrats to promote economic development. Certain smart strategies were implemented during that time. However, in the beginning of his first term of presidency, in 1978, the United States severed official relations with Taiwan, and recognized the People's Republic of China (mainland China) as the legitimate government of China. Since then, international relations became difficult for the Taiwanese government.
The South Korean economy is characterized by conglomerates, which were gradually cultivated through a series of National 5-Year Economic Plans in the 1960s and 1970s. During the Yushin Regime of the Fourth Republic, President Park focused on the development of heavy industries by the Third (1972-1976) and Fourth (1977-1981) National 5-Year Plans. The efforts of the so-called big push further strengthened the economic powers of the conglomerates.
For the purpose of economic and social development, each year since 1972, the Taiwanese government invited foreign Chinese professionals to visit the island and provide their opinions concerning the future developments of Taiwan. This occasion is called the National Development Meeting (NDM, or Kuo Chien Hueh in Chinese). As in the inaugural speech of Prime Minister Sun in the 1981 NDM, almost all 1,847 suggestions by members of the 1978-1980 NDMs had been considered for policy implications. In brief, the NDM became an important tool for national policy making in the 1970s and 1980s, in response to Taiwan's isolated situation since the early 1970s. For example, the semiconductor industry was created based on the opinions of a small group of Chinese-American professionals who were fully experienced in this related domain in the United States. Although the subjects of the NDMs covered a wide range of social issues, including social welfare and medical care, major topics that the government considered more seriously were regarding economic development.
Korean companies started to develop vaccines in the late 1970s. With assistance from foreign experts, especially those of the World Health Organization (WHO) task force, these companies successfully developed a plasma-derived vaccine in 1982, only 1 year after Pasteur and Merck, two leading vaccine producers at that time. The domestic vaccines entered clinical trials among the staff members of the companies. The results showed efficacy of the vaccine. The success of the domestic vaccine development encouraged the South Korean government to launch a nationwide immunization program in 1983. The program, called the Hepatitis B Eradication 5-Year Program, was based on the clinical trial results of the companies [4].
The vaccination policy was created by the Ministry of Health and Society (MoHS), and especially by the Institute of Health of the MoHS. The head of the MoHS from 1982 to 1985 was Jung-rye Kim, a former Senator, feminist, and politician. The Institute of Health was directed by a pharmacist, Dr. Dal-hyun Jee. The first was a professional politician, the second a civil servant. Without medical expertise, these administrative officers followed the South Korean administrative tradition to ensure that the immunization policy was feasible.
In Taiwan, the minister of the Department of Health (DoH) is often assigned to senior physicians, and especially to former deans of prestigious medical schools. The DoH can, therefore, have a stronger relationship with the medical community. For example, Dr. Hsu, the minister of the DoH from 1981 to 1986, was an expert on vaccinations. He launched mass vaccination campaigns against polio and Japanese encephalitis (JE) in the mid-1960s, when he was the director of the Provincial Department of Health [5]. With these campaigns, he also conducted clinical trials on polio and JE vaccines.
The Hepatitis B Prevention Plan was recommended by the NDM. This was the first time an immunization program was directed by the Executive Yuan. To master technological details, the Hepatitis Direction Committee was created, consisting not only of governmental staff and domestic experts, but also of foreign advisors, including I. R. Bennett and S. Krugman. These foreign advisors were helpful in settling disputes over trials performed on newborns because they were considered real experts at that time. Regardless, the DoH is relatively separate from other governmental departments and ministries because of its uniqueness. Therefore, domestic vaccines were not specially preferred by the public health sector, which was influenced by attitudes of the DoH.
Before the Hepatitis B Prevention Plan was initiated, two clinical trials of the hepatitis B vaccines were conducted in Taiwan, in 1981. A research team partly composed of members of National Taiwan University Hospital (NTUH), led by Beasley, used the Merck vaccines to inoculate newborns. Another team used Pasteur's vaccines. The two trials obtained similar results, with the vaccines shown to have an efficacy of approximately 94%. These trials were polemic, but their results are strong evidence for instituting immunization programs.
Mass vaccinations of newborns started on July 1, 1984. The vaccines used were provided by Pasteur's vaccines. A technological transfer contract had been signed between the Taiwanese government and Pasteur's vaccines before the hepatitis B vaccination campaign to build the domestic capability of manufacturing Pasteur's plasma-derived vaccines. The manufacturing capacity was realized by creating a vaccine company called Lifeguard. During the building of Lifeguard and training staff, Pasteur's vaccines promised to provide vaccines at $4 per dose to Taiwan. At that time, the actual price of each dose was approximately $20-$50 [6].
From 1984 to 1985, infants of hepatitis B surface antigen-positive women were vaccinated at 1.5 weeks, 9 weeks, and 12 months with plasma-derived vaccines. The immunization program was expanded to all newborns in 1986. Since then, each infant received four doses of plasma-derived vaccines at ages 0, 1, 2, and 12 months [7]. Since the licensing of recombinant DNA vaccines in 1990, infants can now also be vaccinated with these at ages 0, 1, and 6 months [6]. The coverage rate of hepatitis B vaccinations among newborns was sufficiently high (Fig. 2). Fig. 2 shows that the average doses inoculated for each infant approach 4 in the era of plasma-derived vaccine and decline to approximately 3 when recombinant DNA vaccines were introduced in Taiwan.
The high coverage rate of hepatitis B immunization may partly be the result of modifying the childhood vaccination registry system after a polio outbreak in 1981. The outbreak was caused by labor migration from Southern to Northern Taiwan. Accordingly, a system of personal vaccination records was established, which is helpful for surveillance and the promotion of childhood vaccinations. Moreover, because certain medical professionals were deeply involved in the mass immunization program, they could monitor the progress of the program by using their expertise. Thus, parallel to the mass vaccinations of infants since 1984, a long-term survey was conducted by MH Chang, a pediatrician at NTUH. The results of the survey, published in 1997, proved that the vaccination effectively reduced the liver cancer rate in Taiwan [8].
In contrast to Taiwan's approach of technological transfers through the government's efforts, a domestic supply of hepatitis B vaccines became available in South Korea in 1983. We describe the strategy of obtaining self-sufficiency for vaccines in South Korea below. Based on the clinical trial results of the domestic vaccine providers, the South Korean government launched a 5-Year Immunization Program in 1984. The Hepatitis B Eradication 5-Year Program aimed to vaccinate 17.2 million people, or approximately 40% of the national population. The targeted groups included adults in high-risk groups, elementary school students, and children under 6 years old. The goal of 4.1 million people being vaccinated by the end of 1986 was also set. However, criticism from foreign and domestic South Korean experts resulted in abandonment of the 5-year program in 1985 [3]. One of the major arguments among the experts is that newborns, rather than adults, must be vaccinated first. Accordingly, although the government stopped the mass vaccination program, parents have been encouraged to have their newborns freely vaccinated with hepatitis B vaccines in public health offices since 1987.
Further action regarding the hepatitis B vaccine did not occur until 1991, when the South Korean Society of Pediatrics recommended the vaccine in the annual book of vaccination guidelines by including it in the vaccination tables. A couple of years later, in response to the WHO, the South Korean government finally added the hepatitis B vaccine to the list of National Mandatory Vaccines in 1995, which was encouraged by a newly established expert group for immunization policy recommendations, the South Korea Advisory Committee on Immunization Practices (KACIP) [9]. The institutionalization of the KACIP and other policy-making mechanisms showed that South Korean society was entering a modern era of immunization governance.
South Korean companies, Green Cross and Cheil, obtained plasma-derived vaccine technologies from foreign partners, and successfully developed their own products: Hepavax-B by Green Cross and Hepaccine-B by Cheil. The scales of these companies were sufficiently large because they were the results of the 5-year economic plans, in place since the 1960s. For instance, Cheil belongs to the Samsung conglomerate, the largest business group in South Korea. They can suffer from temporary losses for a considerably larger market in the future. Consequently, Green Cross and Cheil were able to provide low-priced vaccines in South Korea, as well as to the third world, with the recommendations of foreign experts [10].
With their experience with plasma-derived vaccines, Green Cross and Cheil became devoted to the development of recombinant DNA vaccines in the late1980s. LG Chemicals also entered this industry. With its own research team trained abroad, LG produced the first South Korean recombinant DNA vaccine against hepatitis B (Euvaz B) in 1992. Green Cross obtained patented technology from the German company Rhein Biotech, and successfully developed the vaccine Hepavax-Gene in 1996, which was licensed in 1997. However, Cheil failed in developing out new vaccine product. South Korean companies can survive in the competitive high-valued vaccine market because their strategies are aimed at the third world, in which the leading vaccine companies were uninterested [11]. In addition, providing vaccines to the third world was financially supported by non-governmental organizations, such as the Gate Foundation and United Nations Children's Fund (UNICEF).
Under the Hepatitis B Prevention Plan, the Taiwanese company, Lifeguard, was created by the government for three purposes: to provide vaccines for public health, to improve scientific research, and to promote the domestic biomedical industry. However, the project of building the company was assigned to the National Science Council (NSC). The NSC is responsible for policy making and resource allocation for basic research, but it is not competent in industrial affairs. Thus, in 1984, the NSC created a liaison unit called the Development Center for Biotechnology (DCB) to be responsible for industrial affairs, such as providing administrative support to Lifeguard without requiring the direct intervention of the NSC. The new vaccine company had an ambiguous status among science, public health, and the industry.
Because Lifeguard was created through a special project and coordinated under the NSC, rather than the Ministry of Economic Affairs, it had no other support except for government investment through the National Hepatitis B Prevention Program (i.e., the company was required to be self-sustaining from its inception). In addition, limited by technological development of Pasteur Vaccins, Lifeguard could obtain only the plasma-derived vaccine technology. Although Pasteur's recombinant DNA vaccine technology was nearly available at that time, it failed to develop out a new vaccine product because of patents of Smith-Klein.
When the recombinant DNA vaccines of Merck and Smith-Klein were approved for vaccinating infants in Taiwan, most people switched from the domestically produced plasma-derived vaccines to the so-called second-generation vaccines. Without a domestic market, Lifeguard stopped functioning in 1992, and announced its dissolution in May 1995. South Korean companies also stopped plasma-derived vaccine production in 2004 because of market constraints. However, recombinant DNA vaccines continue to be supplied by South Korean producers.
Mass vaccination programs in South Korea and Taiwan were proven to be effective in the prevention of liver cancer [8,12]. However, the different strategies to universal immunization resulted in contrasting configurations of vaccination adoption and production in the two countries. Production capability was established prior to adoption of hepatitis B vaccines in South Korea, whereas the opposite occurred in Taiwan.
Mass vaccination of newborns was a big challenge to the Taiwanese vaccination program. To cope with the hepatitis B immunization program, considerable governance restructuring occurred in the late 1980s. For example, a professional advisory group was established at that time. Although no new vaccine was introduced in the vaccination schedule during the 1990s, a modernized immunization policy-making system was established in Taiwan with the help of the hepatitis B immunization program. However, the hepatitis B immunization program also impeded the development of the domestic supply of new vaccines, as evidenced by Lifeguard's failure.
The case in South Korea was contrary. The production capability of vaccines was critical to institutional reformation of the immunization system in South Korea. Driven by the exportation requirements of South Korean vaccine companies and the WHO's recommendations on new vaccine adoption, regulatory and immunization policies in South Korea have been modernized since the mid-1990s. For example, the Korea Food and Drug Safety headquarters was created in 1996, and was transformed into the Korea Food and Drug Administration in 1998. All departments followed the standards recommended by the WHO, driven by the production and supplies of vaccines against hepatitis B of the Korean firms.
For both South Korea and Taiwan, mass vaccination against hepatitis B marked a turning point toward their modern immunization states. History shows that South Korea and Taiwan had similar developmental backgrounds in the twentieth century. The disease burdens from hepatitis B in these two societies were also similar in the 1970s. However, political and social conditions in the 1980s shaped different paths toward vaccination in South Korea and Taiwan. The adoption of vaccines relies on the government's actions. However, the government is not a single entity; rather, it consists of different actors whose actions depend on their specific interests and contingent situations. Certain political and professional actors have played critical roles in the decision-making process, which reflects actual political and social situations. Thus, these strategies may further interact with the immunization characteristics of the vaccines to shape unique paths to universal immunization. From the cases of hepatitis B vaccine adoption and production, we can find more inconsistencies between South Korea and Taiwan.
Figures and Tables
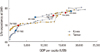 | Fig. 1Comparison of social development between South Korea and Taiwan during the period of 1970-2010. Taiwan and Korea have similar paths of growth in terms of life expectancy and gross domestic product (GDP) per capita. The paths are not identical because of different social and economic contexts. Source: adapted from World Bank; DG Budget, Accounting and Statistics, Taiwan. |
 | Fig. 2Average doses of vaccine inoculated per newborns in Taiwan from 1986 to 2000. The average doses inoculated for each infant approach 4 in the era of plasma-derived vaccine and decline to approximately 3 when recombinant DNA vaccines were introduced in Taiwan. Source: Department of Health (DoH), Taiwan. |
References
1. Denis F, Levy-Bruhl D. Mass vaccination against hepatitis B: the French example. Curr Top Microbiol Immunol. 2006; 304:115–129.

2. Yang S, Khang YH, Harper S, Davey Smith G, Leon DA, Lynch J. Understanding the rapid increase in life expectancy in South Korea. Am J Public Health. 2010; 100:896–903.

3. Kim CY, Tilles JG. Purification and biophysical characterization of hepatitis B antigen. J Clin Invest. 1973; 52:1176–1186.

4. Han JY, Jung TW, Koh DK, Kim JH. A survey for changed control policies of hepatitis B in Republic of Korea. Korean J Pediatr Infect Dis. 2011; 18:124–134.

5. Hsu TC, Chow LP, Wei HY, Chen CL, Hsu ST. A controlled field trial for an evaluation of effectiveness of mouse-brain Japanese encephalitis vaccine. Taiwan Yi Xue Hui Za Zhi. 1971; 70:55–62.
6. Hsu HM. History of hepatitis B in Taiwan. Epidemiol Bull (Taipei Taiwan). 1998; 14:82–91.
7. Chen DS, Hsu NH, Sung JL, et al. A mass vaccination program in Taiwan against hepatitis B virus infection in infants of hepatitis B surface antigen-carrier mothers. JAMA. 1987; 257:2597–2603.

8. Chang MH, Chen CJ, Lai MS, et al. Taiwan Childhood Hepatoma Study Group. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. N Engl J Med. 1997; 336:1855–1859.

9. Cha SH. The history of vaccination and current vaccination policies in Korea. Clin Exp Vaccine Res. 2012; 1:3–8.

10. Muraskin W. The war against hepatitis B: a history of the International Task Force on Hepatitis B Immunization. Philadelphia: University of Pennsylvania Press;1995. p. 23–65.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download