Abstract
Septic pulmonary embolism occurs when septic material becomes detached from its origin and infiltrates into the pulmonary parenchyma causing significant clinical symptoms. It is uncommon in children and mostly related to intravascular catheterization, endocarditis, pelvic thrombophlebitis, and soft tissue infection. We report a case of a 5-year-old boy who experienced septic pulmonary embolism originating from a left shoulder abscess after traumatic injury. Magnetic resonance imaging of the shoulder revealed a multifocal subcutaneous and intramuscular abscess with septic arthritis. The initial chest radiograph showed suspicious pneumonic infiltration with nodular opacities. A percutaneous catheter was inserted to drain the shoulder abscess, and cefazedone, a first-generation cephalosporin, was administered intravenously. Two days later, a chest radiograph taken for the follow-up of the initial pneumonic infiltration with nodular opacities demonstrated aggravation of multifocal nodular lesions in bilateral lung fields, with one of the nodular cavities containing an air-fluid level. Despite the absence of significant respiratory symptoms, chest computed tomography showed multifocal necrotic nodules and cavity lesions with feeding vessel signs dominantly in the left lower lung field, which is characteristic of septic pulmonary embolism. Methicillin-susceptible Staphylococcus aureus was isolated from the shoulder abscess, whereas repeated blood and sputum cultures did not reveal any bacterial growth. With resolution of clinical symptoms as well as the finding of chest computed tomography, the patient was discharged 18 days after admission in a stable condition. Regression of the multifocal pulmonary nodular lesions was noticed on the subsequent chest imaging studies performed 45 days after the treatment.
Figures and Tables
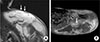 | Fig. 1Magnetic resonance imaging of the left shoulder. Coronal (A) and axial (B) images are showing the large and multifocal intramuscular wall enhancing fluid collection suggestive of abscesses (white arrows). Septic arthritis was also noted in the left shoulder joint (not shown). |
 | Fig. 2Initial chest radiograph (A) showing suspicious pneumonic infiltration with nodular opacities on both lung fields (distinct semicircular shadow are unrelated detail) and 3 days later follow-up chest radiograph (B) demonstrating aggravation of multifocal nodular lesions in both lung fields, with one of the nodular cavities containing an air-fluid level (white arrow) |
References
1. Sakuma M, Sugimura K, Nakamura M, Takahashi T, Kitamukai O, Yazu T, et al. Unusual pulmonary embolism: septic pulmonary embolism and amniotic fluid embolism. Circ J. 2007; 71:772–775.

2. Lee SJ, Cha SI, Kim CH, Park JY, Jung TH, Jeon KN, et al. Septic pulmonary embolism in Korea: microbiology, clinicoradiologic features, and treatment outcome. J Infect. 2007; 54:230–234.

3. Wong KS, Lin TY, Huang YC, Hsia SH, Yang PH, Chu SM. Clinical and radiographic spectrum of septic pulmonary embolism. Arch Dis Child. 2002; 87:312–315.

4. Cook RJ, Ashton RW, Aughenbaugh GL, Ryu JH. Septic pulmonary embolism: presenting features and clinical course of 14 patients. Chest. 2005; 128:162–166.
5. Stawicki SP, Firstenberg MS, Lyaker MR, Russell SB, Evans DC, Bergese SD, et al. Septic embolism in the intensive care unit. Int J Crit Illn Inj Sci. 2013; 3:58–63.

6. Miyashita T, Shimamoto Y, Nishiya H, Koshibu Y, Sugiyama H, Ono Y, et al. Destructive pulmonary embolism in a patient with community-acquired staphylococcal bacteremia. J Infect Chemother. 2002; 8:99–102.

7. Gonzalez BE, Hulten KG, Dishop MK, Lamberth LB, Hammerman WA, Mason EO Jr, et al. Pulmonary manifestations in children with invasive community-acquired Staphylococcus aureus infection. Clin Infect Dis. 2005; 41:583–590.

8. Kuhlman JE, Fishman EK, Teigen C. Pulmonary septic emboli: diagnosis with CT. Radiology. 1990; 174:211–213.

9. Dodd JD, Souza CA, Müller NL. High-resolution MDCT of pulmonary septic embolism: evaluation of the feeding vessel sign. AJR Am J Roentgenol. 2006; 187:623–629.

10. Iwasaki Y, Nagata K, Nakanishi M, Natuhara A, Harada H, Kubota Y, et al. Spiral CT findings in septic pulmonary emboli. Eur J Radiol. 2001; 37:190–194.

11. Shiota Y, Arikita H, Horita N, Hiyama J, Ono T, Ohkawa S, et al. Septic pulmonary embolism associated with periodontal disease: reports of two cases and review of the literature. Chest. 2002; 121:652–654.

12. Osei C, Berger HW, Nicholas P. Septic pulmonary infarction: clinical and radiographic manifestations in 11 patients. Mt Sinai J Med. 1979; 46:145–148.
13. Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJ, et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005; 41:1373–1406.

14. Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN, et al. Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997-1999. Clin Infect Dis. 2001; 32:Suppl 2. S114–S132.
15. Paul M, Zemer-Wassercug N, Talker O, Lishtzinsky Y, Lev B, Samra Z, et al. Are all beta-lactams similarly effective in the treatment of methicillin-sensitive Staphylococcus aureus bacteraemia? Clin Microbiol Infect. 2011; 17:1581–1586.

16. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003; 348:1546–1554.

17. Kuhajda I, Zarogoulidis K, Tsirgogianni K, Tsavlis D, Kioumis I, Kosmidis C, et al. Lung abscess-etiology, diagnostic and treatment options. Ann Transl Med. 2015; 3:183.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download