Abstract
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome—also known as drug-induced hypersensitivity syndrome—is an uncommon disease entity that manifests as fever, skin rash, blood cell abnormalities, lymphadenopathy, and often coagulopathy. Tigecycline is an antibiotic that is selectively used to treat complicated intra-abdominal and soft-tissue infections. Recently, a few cases of tigecycline-induced coagulopathy have been reported. Herein, we report a case of tigecycline-induced coagulopathy in a patient with DRESS syndrome. Both prothrombin time and activated partial thromboplastin time were abruptly exceeded beyond 180 seconds on day 6 of tigecycline treatment and normalized after discontinuation of tigecycline.
Figures and Tables
 | Fig. 2High-resolution chest computed tomography images showing pulmonary edema (A) and mediastinal lymphadenopathy (B; arrow, mediastinal lymphadenom). DRESS syndrome can manifest interstitial pneumonia and pleural effusion. |
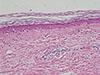 | Fig. 3Skin biopsy showing dermatitis with perivascular lymphocytic and eosinophilic infiltration (H&E, ×400). |
Table 1
Coagulation profiles on select days in the hospital
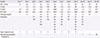
PLT, platelet; PT, prothrombin time; INR, International normalized ratio; aPTT, activated partial thromboplastin time; PC, platelet concentration; FFP, fresh frozen plasma; CP, cryoprecipitate.
*Day 1 test was done in emergency department and day 2 result was considered as initial result in admission.
Table 2
Comparison of reported cases of tigecycline-induced coagulopathy
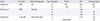
| Source | Comorbidity | Indication for tigecycline | Days of tigecycline | PT (sec) | INR | Fibrinogen (mg/dL) |
|---|---|---|---|---|---|---|
| Sabanis et al.4 | ESRD | SSI | 10 | 120 | 6.33 | 297 |
| 19 | 18.8 | 1.71 | 42 | |||
| Pieringer et al.3 | ESRD | Peritonitis | 15 | - | 1.50 | - |
| 35 | - | 1.76 | 38 | |||
| 39 | - | 3.08 | 30 | |||
| Rossitto et al.5 | LC with AKI | Severe septic shock | 6 | - | 2.70 | 50 |
| 7 | Indeterminate | - | 25 |
References
1. Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, et al. The DRESS syndrome: a literature review. Am J Med. 2011; 124:588–597.

2. Kimmoun A, Dubois E, Perez P, Barbaud A, Levy B. Shock state: an unrecognized and underestimated presentation of drug reaction with eosinophilia and systemic symptoms. Shock. 2013; 40:387–391.
3. Pieringer H, Schmekal B, Biesenbach G, Pohanka E. Severe coagulation disorder with hypofibrinogenemia associated with the use of tigecycline. Ann Hematol. 2010; 89:1063–1064.

4. Sabanis N, Paschou E, Gavriilaki E, Kalaitzoglou A, Vasileiou S. Hypofibrinogenemia induced by tigecycline: a potentially life-threatening coagulation disorder. Infect Dis (Lond). 2015; 47:743–746.

5. Rossitto G, Piano S, Rosi S, Simioni P, Angeli P. Life-threatening coagulopathy and hypofibrinogenaemia induced by tigecycline in a patient with advanced liver cirrhosis. Eur J Gastroenterol Hepatol. 2014; 26:681–684.

6. Zhang Q, Zhou S, Zhou J. Tigecycline treatment causes a decrease in fibrinogen levels. Antimicrob Agents Chemother. 2015; 59:1650–1655.

7. Kardaun SH, Sidoroff A, Valeyrie-Allanore L, Halevy S, Davidovici BB, Mockenhaupt M, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007; 156:609–611.

8. Richard MA, Fiszenson F, Jreissati M, Jean Pastor MJ, Grob JJ. Cutaneous adverse effects during selective serotonin reuptake inhibitors therapy: 2 cases. Ann Dermatol Venereol. 2001; 128:759–761.
9. Heymann WR. Addressing the role of human herpesviruses 6 and 7 in DRESS. Skinmed. 2014; 12:100–101.
10. Morito H, Ogawa K, Fukumoto T, Kobayashi N, Morii T, Kasai T, et al. Increased ratio of FoxP3+ regulatory T cells/CD3+ T cells in skin lesions in drug-induced hypersensitivity syndrome/drug rash with eosinophilia and systemic symptoms. Clin Exp Dermatol. 2014; 39:284–291.

11. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: part I. Clinical perspectives. J Am Acad Dermatol. 2013; 68:693.
12. Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2011; 36:6–11.

13. Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996; 15:250–257.

14. Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis. 2010; 10:597–602.

15. Barberan J, Mensa J, Farinas C, Llinares P, Olaechea P, Palomar M, et al. Recommendations of antimicrobial treatment in patients allergic to beta-lactam antibiotics. Rev Esp Quimioter. 2008; 21:60–82.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download