Abstract
Purpose
It is difficult to differentiate between viral and bacterial pneumonia in children and to decide antibiotic therapy. Study was conducted to investigate the clinical usefulness of antibiotic therapy based on procalcitonin (PCT) in children diagnosed with viral pneumonia.
Methods
This study included 108 patients diagnosed with viral pneumonia. Patient's age, fever duration, hospital stay, and treatment progress were noted, and laboratory study including PCT levels were tested. In addition, Polymerase chain reaction was done to test for viruses. Patients were divided into PCT and non-PCT groups according to PCT level. And their clinical patterns, treatment outcome, antibiotic use, severity of complications were compared.
Results
The number of patients with respiratory syncytial virus (RSV) was 35 and 50, rhinovirus was 5 and 10 in PCT and non-PCT groups, respectively. Fever duration was longer by 2.5 days in PCT group than in the non-PCT group (P<0.001), but there was no difference in the duration of hospital stay (P=0.191). White blood cell and absolute neutrophil count levels were higher in the PCT group (P=0.013 and P<0.001, respectively). Use of antibiotic therapy was performed in group was on 22% and 90% of patients in the PCT and non-PCT groups, respectively showing a significant reduction in the frequency of antibiotic therapy in PCT group, without a significant difference in treatment outcome, despite more severe clinical signs (P<0.001).
Figures and Tables
Fig. 1
Trial profile. AOM, acute otitis media; RDS, respiratory distress syndrome; PCT, procalcitonin.

Fig. 3
Antibiotic use according to PCT-guidance strategy in children with viral pneumonia. The PCT group significantly showed lower rate of antibiotic use than non-PCT. PCT, procalcitonin.

Table 1
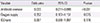
Information of children with pneumonia

Table 2
Clinical and laboratory differences in children with viral pneumonia according to procalcitonin-guideline antibiotic therapy

References
1. Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet. 2004; 363:600–607.

2. Deis JN, Creech CB, Estrada CM, Abramo TJ. Procalcitonin as a marker of severe bacterial infection in children in the emergency department. Pediatr Emerg Care. 2010; 26:51–60.

3. Schuetz P, Christ-Crain M, Albrich W, Zimmerli W, Mueller B. ProHOSP Study Group. Guidance of antibiotic therapy with procalcitonin in lower respiratory tract infections: insights into the ProHOSP study. Virulence. 2010; 1:88–92.

4. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993; 341:515–518.

5. Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide to antibiotic decisions: past, present and future. BMC Med. 2011; 9:107.

6. Virkki R, Juven T, Rikalainen H, Svedstrom E, Mertsola J, Ruuskanen O. Differentiation of bacterial and viral pneumonia in children. Thorax. 2002; 57:438–441.

7. Ashworth M, Charlton J, Latinovic R, Gulliford M. Age-related changes in consultations and antibiotic prescribing for acute respiratory infections, 1995-2000. Data from the UK General Practice Research Database. J Clin Pharm Ther. 2006; 31:461–467.

8. Don M, Valent F, Korppi M, Canciani M. Differentiation of bacterial and viral community-acquired pneumonia in children. Pediatr Int. 2009; 51:91–96.

9. Christ-Crain M, Stolz D, Bingisser R, Muller C, Miedinger D, Huber PR, et al. Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med. 2006; 174:84–93.

10. Muller B, Christ-Crain M, Nylen ES, Snider R, Becker KL. Limits to the use of the procalcitonin level as a diagnostic marker. Clin Infect Dis. 2004; 39:1867–1868.

11. Schuetz P, Briel M, Christ-Crain M, Stolz D, Bouadma L, Wolff M, et al. Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: an individual patient data meta-analysis. Clin Infect Dis. 2012; 55:651–662.

12. Lim HH, Kang HJ, Yang EA, Lee JH. Clinical usefulness of procalcitonin as guideline of antibiotic treatment in children with respiratory tract infection. Pediatr Allergy Respir Dis. 2012; 22:110–115.

13. Albrich WC, Dusemund F, Bucher B, Meyer S, Thomann R, Kuhn F, et al. Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in "real life": an international, multicenter poststudy survey (ProREAL). Arch Intern Med. 2012; 172:715–722.

14. Drozdov D, Dusemund F, Muller B, Albrich WC. Efficacy and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections. Antibiotics. 2013; 2:1–10.

15. Gendrel D, Bohuon C. Procalcitonin, a marker of bacterial infection. Infection. 1997; 25:133–134.

16. Chan YL, Tseng CP, Tsay PK, Chang SS, Chiu TF, Chen JC. Procalcitonin as a marker of bacterial infection in the emergency department: an observational study. Crit Care. 2004; 8:R12–R20.
17. van Rossum AM, Wulkan RW, Oudesluys-Murphy AM. Procalcitonin as an early marker of infection in neonates and children. Lancet Infect Dis. 2004; 4:620–630.

18. Becker KL, Snider R, Nylen ES. Procalcitonin assay in systemic inflammation, infection, and sepsis: clinical utility and limitations. Crit Care Med. 2008; 36:941–952.

19. Christ-Crain M, Muller B. Biomarkers in respiratory tract infections: diagnostic guides to antibiotic prescription, prognostic markers and mediators. Eur Respir J. 2007; 30:556–573.

20. Harbarth S, Holeckova K, Froidevaux C, Pittet D, Ricou B, Grau GE, et al. Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med. 2001; 164:396–402.

21. Li H, Luo YF, Blackwell TS, Xie CM. Meta-analysis and systematic review of procalcitonin-guided therapy in respiratory tract infections. Antimicrob Agents Chemother. 2011; 55:5900–5906.

22. Schuetz P, Christ-Crain M, Thomann R, Falconnier C, Wolbers M, Widmer I, et al. Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA. 2009; 302:1059–1066.

23. Schuetz P, Albrich W, Christ-Crain M, Chastre J, Mueller B. Procalcitonin for guidance of antibiotic therapy. Expert Rev Anti Infect Ther. 2010; 8:575–587.

24. Prat C, Dominguez J, Rodrigo C, Gimenez M, Azuara M, Jimenez O, et al. Procalcitonin, C-reactive protein and leukocyte count in children with lower respiratory tract infection. Pediatr Infect Dis J. 2003; 22:963–968.

25. Hatzistilianou M, Hitoglou S, Gougoustamou D, Rekliti A, Tzouvelekis G, Nanas C, et al. Serum procalcitonin, adenosine deaminase and its isoenzymes in the aetiological diagnosis of pneumonia in children. Int J Immunopathol Pharmacol. 2002; 15:119–127.

26. Moulin F, Raymond J, Lorrot M, Marc E, Coste J, Iniguez JL, et al. Procalcitonin in children admitted to hospital with community acquired pneumonia. Arch Dis Child. 2001; 84:332–336.

27. Toikka P, Irjala K, Juven T, Virkki R, Mertsola J, Leinonen M, et al. Serum procalcitonin, C-reactive protein and interleukin-6 for distinguishing bacterial and viral pneumonia in children. Pediatr Infect Dis J. 2000; 19:598–602.

28. Korppi M, Remes S, Heiskanen-Kosma T. Serum procalcitonin concentrations in bacterial pneumonia in children: a negative result in primary healthcare settings. Pediatr Pulmonol. 2003; 35:56–61.

29. Korppi M, Remes S. Serum procalcitonin in pneumococcal pneumonia in children. Eur Respir J. 2001; 17:623–627.

30. Don M, Valent F, Korppi M, Falleti E, De Candia A, Fasoli L, et al. Efficacy of serum procalcitonin in evaluating severity of community-acquired pneumonia in childhood. Scand J Infect Dis. 2007; 39:129–137.

31. Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004; 39:206–217.

32. Muller B, Becker KL. Procalcitonin: how a hormone became a marker and mediator of sepsis. Swiss Med Wkly. 2001; 131:595–602.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download