Abstract
Purpose
We analyzed the pulmonary function and risk factors of allergic rhinitis (AR) in dust mite-sensitized children with current AR and no history of asthma.
Methods
In this cross-sectional study, demographic and disease-related information was obtained from 1,792 Korean children aged 9–12 years using a questionnaire, skin-prick testing, spirometric analysis, and methacholine challenge testing.
Results
A total of 672 children were analyzed. The control group consisted of 583 children without any allergic diseases who were not sensitized to 16 common allergens. The group with current AR and dust mite sensitization consisted of 89 children. Binary logistic regression analysis showed that helminth infection (adjusted odds ratio [aOR], 2.88; 95% confidence interval [CI], 1.23–6.77) and antibiotic use during infancy (aOR, 1.89; 95% CI, 1.10–3.25) were the risk factors. Pet ownership (aOR, 0.32; 95% CI, 0.15–0.69) and older siblings (aOR, 0.58; 95% CI, 0.35–0.96) were protective factors. Spirometry results did not differ between the control and dust mite-induced AR groups. None of the children showed a bronchodilator response. However, 8.5%, 7.1%, and 2.1% of the control-group children and 28.7%, 23.0%, and 8.0% of the dust mite-induced AR-group children showed methacholine PC20 (provocative concentration of methacholine causing a 20% fall in forced expiratory volume in 1 second) values of ≤25 mg/mL, ≤16 mg/mL, and ≤8 mg/mL, respectively (P<0.01).
Figures and Tables
Table 1
Demographics with control group vs. current allergic rhinitis with dust mite sensitization group

Table 2
Binary logistic regression analysis of risk factors (adjusted OR, 95% CI) for current allergic rhinitis with dust mite sensitization group
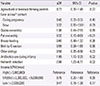
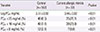
Table 3
Pulmonary function of control and current allergic rhinitis with dust mite sensitization group

Table 4
Methacholine PC20 of control and current allergic rhinitis with dust mite sensitization group
References
1. Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010; 126:466–476.

2. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet. 1998; 351:1225–1232.
3. Hong SJ. Korean ISAAC Study Group of Korean Association of Allergy and Respiratory Disease. Report of Korean ISAAC epidemiologic study for asthma and allergic diseases in children. Pediatr Allergy Respir Dis. 2007; 17:Suppl 1. S55–S66.
4. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Korean J Pediatr. 2008; 51:343–350.

5. Marogna M, Massolo A, Berra D, Zanon P, Chiodini E, Canonica GW, et al. The type of sensitizing allergen can affect the evolution of respiratory allergy. Allergy. 2006; 61:1209–1215.

6. Sener O, Kim YK, Ceylan S, Ozanguc N, Yoo TJ. Comparison of skin tests to aeroallergens in Ankara and Seoul. J Investig Allergol Clin Immunol. 2003; 13(3):202–208.
7. Jeong KY, Park JW, Hong CS. House dust mite allergy in Korea: the most important inhalant allergen in current and future. Allergy Asthma Immunol Res. 2012; 4:313–325.

8. Kim JE, An HS, Kim MJ, Jung JA. A comparison of the sensitization rate to house dust mite in children with allergic disease in Busan's Single University Hospital in 2002 and 2007. Korean J Asthma Allergy Clin Immunol. 2009; 29:117–122.
9. Kwon JW, Seo JH, Yu J, Kim BJ, Kim HB, Lee SY, et al. Relationship between the prevalence of allergic rhinitis and allergen sensitization in children of Songpa area, Seoul. Pediatr Allergy Respir Dis. 2011; 21:47–55.

10. Cockcroft DW, Davis BE. Mechanisms of airway hyperresponsiveness. J Allergy Clin Immunol. 2006; 118:551–559.

11. Park JJ, Kim JJ, Kang IJ. The risk factors for persistence of asthma symptoms from late childhood to early adult life: the effects of pulmonary function and bronchial hyperresponsiveness. Pediatr Allergy Respir Dis. 2008; 18:138–147.
12. Roorda RJ, Gerritsen J, van Aalderen WM, Schouten JP, Veltman JC, Weiss ST, et al. Follow-up of asthma from childhood to adulthood: influence of potential childhood risk factors on the outcome of pulmonary function and bronchial responsiveness in adulthood. J Allergy Clin Immunol. 1994; 93:575–584.

13. Katelaris CH. Allergic rhinitis and asthma: epidemiological evidence for the link. Clin Exp Allergy Rev. 2003; 3:5–8.

15. Bugiani M, Carosso A, Migliore E, Piccioni P, Corsico A, Olivieri M, et al. Allergic rhinitis and asthma comorbidity in a survey of young adults in Italy. Allergy. 2005; 60:165–170.

16. Asher I. ISAAC International Study of Asthma and Allergies in childhood. Pediatr Pulmonol. 2007; 42:100.

17. Plaschke PP, Janson C, Norrman E, Bjornsson E, Ellbjar S, Jarvholm B. Onset and remission of allergic rhinitis and asthma and the relationship with atopic sensitization and smoking. Am J Respir Crit Care Med. 2000; 162(3 Pt 1):920–924.

18. Settipane RJ, Hagy GW, Settipane GA. Long-term risk factors for developing asthma and allergic rhinitis: a 23-year follow-up study of college students. Allergy Proc. 1994; 15:21–25.

19. Suh DI, Lee JK, Kim JT, Min YG, Koh YY. Bronchial hyperresponsiveness in preschool children with allergic rhinitis. Am J Rhinol Allergy. 2011; 25:e186–e190.

20. Choi SH, Yoo Y, Yu J, Rhee CS, Min YG, Koh YY. Bronchial hyperresponsiveness in young children with allergic rhinitis and its risk factors. Allergy. 2007; 62:1051–1056.

21. Braman SS, Barrows AA, DeCotiis BA, Settipane GA, Corrao WM. Airway hyperresponsiveness in allergic rhinitis: a risk factor for asthma. Chest. 1987; 91:671–674.
22. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–338.

23. Yoon KA, Lim HS, Koh YY, Kim H. Normal predicted values of pulmonary function test in Korean school-aged children. J Korean Pediatr Soc. 1993; 36:25–37.
24. Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005; 26:948–968.

25. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, et al. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000; 161:309–329.
26. Selcuk ZT, Caglar T, Enunlu T, Topal T. The prevalence of allergic diseases in primary school children in Edirne, Turkey. Clin Exp Allergy. 1997; 27:262–269.

27. Lee SI, Shin MH, Lee HB, Lee JS, Son BK, Koh YY, et al. Prevalences of symptoms of asthma and other allergic diseases in Korean children: a nationwide questionnaire survey. J Korean Med Sci. 2001; 16:155–164.

28. Nam SY, Yoon HS, Kim WK. Prevalence of allergic disease in kindergarten age children in Korea. Pediatr Allergy Respir Dis. 2005; 15:439–445.
29. Kim YH, Urm SH, Kim WK. Prevalence of allergic diseases and risk factors in preschool children, 2009. Pediatr Allergy Respir Dis. 2011; 21:165–175.

30. Kay AB. Concepts of allergy and hypersensitivity. In : Kay AB, Kaplan AP, Bousquet J, Holt PG, editors. Allergy and allergic disease. Oxford: Blackwell Science Ltd.;1997. p. 23–35.
31. Jarjour NN, Gern JE, Kelly EA, Swenson CA, Dick CR, Busse WW. The effect of an experimental rhinovirus 16 infection on bronchial lavage neutrophils. J Allergy Clin Immunol. 2000; 105(6 Pt 1):1169–1177.

32. Denburg JA, Sehmi R, Saito H, Pil-Seob J, Inman MD, O'Byrne PM. Systemic aspects of allergic disease: bone marrow responses. J Allergy Clin Immunol. 2000; 106:5 Suppl. S242–S246.

33. Simons FE. Allergic rhinobronchitis: the asthma-allergic rhinitis link. J Allergy Clin Immunol. 1999; 104(3 Pt 1):534–540.

34. Devalia JL, Bayram H, Rusznak C, Calderon M, Sapsford RJ, Abdelaziz MA, et al. Mechanisms of pollution-induced airway disease: in vitro studies in the upper and lower airways. Allergy. 1997; 52:38 Suppl. 45–51.

35. Ciprandi G, Cirillo I, Pistorio A. Impact of allergic rhinitis on asthma: effects on spirometric parameters. Allergy. 2008; 63:255–260.

36. Tavakol M, Gharagozlou M, Afaride M, Movahedi M, Tavakol Z. Asthma diagnosis and treatment - 1002. FEF25-75%: a more sensitive indicator in the early detection of asthma. World Allergy Organ J. 2013; 6:Suppl 1. P2.

37. Simon MR, Chinchilli VM, Phillips BR, Sorkness CA, Lemanske RF Jr, Szefler SJ, et al. Forced expiratory flow between 25% and 75% of vital capacity and FEV1/forced vital capacity ratio in relation to clinical and physiological parameters in asthmatic children with normal FEV1 values. J Allergy Clin Immunol. 2010; 126:527–534.e1-8.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download