Abstract
Purpose
This study aimed to evaluate the clinical factors that could influence the length of hospital stay (LHS) of infants with acute bronchiolitis using the bronchiolitis severity score (BSS).
Methods
The medical records of 105 infants aged 0–12 months with acute bronchiolitis who were admitted to a tertiary hospital between December 2014 and May 2015 were reviewed. The BSS was composed 5 factors, namely general condition, wheezing, chest retraction, respiration rate, and peripheral oxygen saturation, which were evaluated at admission. In addition, the age of the infants, LHS, body weight, birth history, familial history, laboratory test result, chest X-ray, and treatment modalities were reviewed. Subjects were classified into 3 groups according to their BSS, and logistic regression analysis was used to identify the association of the BSS with longer LHS.
Results
Among subjects, 62 were studied. Their mean LHS and age were 5.5±2.0 days and 3.9±2.7 months, respectively. Twelve infants were classified as mild (20.3%), 43 as moderate (68.8%), and 7 as severe (10.9%). Venous blood gas pH value and white blood cell count were the best predictors of disease severity. The LHS was associated with the BSS, age, body weight and pCO2 by venous blood gas analysis (P<0.05).
Figures and Tables
Fig. 1
Percentage of oxygen therapy and use of systemic corticosteroid in each groups by bronchial severity score (BSS). BSS: mild, 0–5; moderate, 6–10; severe, >10.
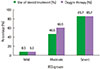
Table 1
Bronchiolitis severity score (BSS)8

Table 2
Demographic characteristics of the subjects (n=62)

Table 3
Demographic characteristics of 3 groups by bronchiolitis severity score (BSS)
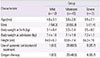
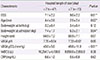
Table 4
Comparison of clinical characteristics between mild, moderate, and severe group
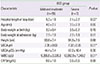
Table 5
Comparison of clinical characteristics between groups sorted by hospital length of stay
References
1. American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics. 2006; 118:1774–1793.
2. Coates BM, Camarda LE, Goodman DM. Wheezing, bronchiolitis, and bronchitis. In : Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier/Saunders;2014. p. 2044–2050.
3. Mansbach JM, Emond JA, Camargo CA Jr. Bronchiolitis in US emergency departments 1992 to 2000: epidemiology and practice variation. Pediatr Emerg Care. 2005; 21:242–247.
4. Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr. Temporal trends in emergency department visits for bronchiolitis in the United States, 2006 to 2010. Pediatr Infect Dis J. 2014; 33:11–18.

5. Roh EJ, Won YK, Lee MH, Chung EH. Clinical characteristics of patients with acute bronchiolitis who visited 146 Emergency Department in Korea in 2012. Allergy Asthma Respir Dis. 2015; 3:334–340.

6. Gouyon JB, Rozé JC, Guillermet-Fromentin C, Glorieux I, Adamon L, DI Maio M, et al. Hospitalizations for respiratory syncytial virus bronchiolitis in preterm infants at <33 weeks gestation without bronchopulmonary dysplasia: the CASTOR study. Epidemiol Infect. 2013; 141:816–826.

7. Feltes TF, Cabalka AK, Meissner HC, Piazza FM, Carlin DA, Top FH Jr, et al. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr. 2003; 143:532–540.

8. Wang EE, Milner RA, Navas L, Maj H. Observer agreement for respiratory signs and oximetry in infants hospitalized with lower respiratory infections. Am Rev Respir Dis. 1992; 145:106–109.

9. Liu LL, Gallaher MM, Davis RL, Rutter CM, Lewis TC, Marcuse EK. Use of a respiratory clinical score among different providers. Pediatr Pulmonol. 2004; 37:243–248.

10. Destino L, Weisgerber MC, Soung P, Bakalarski D, Yan K, Rehborg R, et al. Validity of respiratory scores in bronchiolitis. Hosp Pediatr. 2012; 2:202–209.

11. Lowell D, Lister G, Von Koss H, McCarthy P. Wheezing in infants: the response to epinephrine. Pediatrics. 1987; 79:939–945.

12. Corneli HM, Zorc JJ, Holubkov R, Bregstein JS, Brown KM, Mahajan P, et al. Bronchiolitis: clinical characteristics associated with hospitalization and length of stay. Pediatr Emerg Care. 2012; 28:99–103.
13. Voets S, van Berlaer G, Hachimi-Idrissi S. Clinical predictors of the severity of bronchiolitis. Eur J Emerg Med. 2006; 13:134–138.

14. Alansari K, Sakran M, Davidson BL, Ibrahim K, Alrefai M, Zakaria I. Oral dexamethasone for bronchiolitis: a randomized trial. Pediatrics. 2013; 132:e810–e816.

15. Kim KH, Hwang J, Song JH, Lee YS, Kwon JW, Suh DI, et al. Association between the clinical index and disease severity in infants with acute bronchiolitis. Allergy Asthma Respir Dis. 2013; 1:377–382.

16. Marlais M, Evans J, Abrahamson E. Clinical predictors of admission in infants with acute bronchiolitis. Arch Dis Child. 2011; 96:648–652.

17. Mansbach JM, Clark S, Christopher NC, LoVecchio F, Kunz S, Acholonu U, et al. Prospective multicenter study of bronchiolitis: predicting safe discharges from the emergency department. Pediatrics. 2008; 121:680–688.

18. Lind I, Gill JH, Calabretta N, Polizzoto M. Clinical inquiries. What are hospital admission criteria for infants with bronchiolitis? J Fam Pract. 2006; 55:67–69.
19. Cha MA, Woo YR, Kim HJ, Kim MS, Ahn YH. Factors associated with obesity of acute bronchiolitis in infants: association of obesity with disease severity. Allergy Asthma Respir Dis. 2015; 3:281–287.

20. Katona PG, Egbert JR. Heart rate and respiratory rate differences between preterm and full-term infants during quiet sleep: possible implications for sudden infant death syndrome. Pediatrics. 1978; 62:91–95.

21. Walsh P, Rothenberg SJ, O'Doherty S, Hoey H, Healy R. A validated clinical model to predict the need for admission and length of stay in children with acute bronchiolitis. Eur J Emerg Med. 2004; 11:265–272.

22. Corrard F, de La Rocque F, Martin E, Wollner C, Elbez A, Koskas M, et al. Food intake during the previous 24 h as a percentage of usual intake: a marker of hypoxia in infants with bronchiolitis: an observational, prospective, multicenter study. BMC Pediatr. 2013; 13:6.

23. Lemke M, Hartert TV, Gebretsadik T, Carroll KN. Relationship of secondhand smoke and infant lower respiratory tract infection severity by familial atopy status. Ann Allergy Asthma Immunol. 2013; 110:433–437.

24. Mahabee-Gittens M. Smoking in parents of children with asthma and bronchiolitis in a pediatric emergency department. Pediatr Emerg Care. 2002; 18:4–7.

25. Bryan DL, Hart PH, Forsyth KD, Gibson RA. Immunomodulatory constituents of human milk change in response to infant bronchiolitis. Pediatr Allergy Immunol. 2007; 18:495–502.

26. Carroll KN, Gebretsadik T, Griffin MR, Dupont WD, Mitchel EF, Wu P, et al. Maternal asthma and maternal smoking are associated with increased risk of bronchiolitis during infancy. Pediatrics. 2007; 119:1104–1112.

27. Lanari M, Prinelli F, Adorni F, Di Santo S, Vandini S, Silvestri M, et al. Risk factors for bronchiolitis hospitalization during the first year of life in a multicenter Italian birth cohort. Ital J Pediatr. 2015; 41:40.

28. Pelletier AJ, Mansbach JM, Camargo CA Jr. Direct medical costs of bronchiolitis hospitalizations in the United States. Pediatrics. 2006; 118:2418–2423.

29. Kini NM, Robbins JM, Kirschbaum MS, Frisbee SJ, Kotagal UR. Child Health Accountability Initiative. Inpatient care for uncomplicated bronchiolitis: comparison with Milliman and Robertson guidelines. Arch Pediatr Adolesc Med. 2001; 155:1323–1327.
30. Leader S, Kohlhase K. Recent trends in severe respiratory syncytial virus (RSV) among US infants, 1997 to 2000. J Pediatr. 2003; 143:5 Suppl. S127–S132.

31. Castro-Rodriguez JA, Rodriguez-Martinez CE, Sossa-Briceño MP. Principal findings of systematic reviews for the management of acute bronchiolitis in children. Paediatr Respir Rev. 2015; 16:267–275.

32. Turner T, Wilkinson F, Harris C, Mazza D. Health for Kids Guideline Development Group. Evidence based guideline for the management of bronchiolitis. Aust Fam Physician. 2008; 37(6 Spec No):6–13.
33. Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014; 134:e1474–e1502.

34. Baumer JH. SIGN guideline on bronchiolitis in infants. Arch Dis Child Educ Pract Ed. 2007; 92:ep149–ep151.

35. Kim JS, In DK, Sun YH, Hong HJ, Cho KH, Son DW, et al. Current Management of Acute Bronchiolitis in Incheon. Pediatr Allergy Respir Dis. 2006; 16:150–161.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download