Abstract
Purpose
This study aimed to investigate the prevalence of atopic dermatitis (AD) and associated factors for AD in a total of 2,077 children from 5 elementary schools in Gyeonggi-do province.
Methods
AD was defined when parents answered "Yes" to a question in the on International Study of Asthma and Allergies in Childhood questionnaire "Has your child ever has itchy rashes with xax and wane pattern for at least 6 months?" in October 2012. SCORing Atopic Dermatitis index, skin prick testing and blood testing, were evaluated.
Results
The prevalence of AD was 25.9% among 2,077 elementary school children in Gyeonggi-do province. Proportions of obesity (8.0% vs. 4.5%, P=0.004) and breast-feeding over 6 months (46.6% vs. 41.3%, P=0.035) were significantly higher in children with AD than those without. No significant differences were found in terms of sex, age, body mass index, history of breast-feeding ever and mode of delivery beween AD and non-AD children. obesity (adjusted odds ration [aOR], 1.80; 95% confidence interval [CI], 1.13–2.75; P=0.006) and breast-feeding over 6 months (aOR, 1.35; 95% CI, 1.03–1.77; P=0.029) were found as significant associated factors for AD. When stratified by sex, obesity in boys (aOR, 2.67; 95% CI, 1.53–4.66; P=0.001) and breast-feeding history in girls (aOR, 1.47; 95% CI, 1.03–2.11; P=0.034) were independently considered significant associated factors for AD. We found more boys (66.7%, P=0.028) than girls among the severe AD cases. Male sex was considered an associated factor of having severe AD (aOR, 2.23; 95% CI, 1.01–4.73; P=0.048).
Figures and Tables
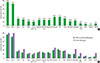 | Fig. 1(A) The most common sensitized allergen group was house dust mites, followed by pollen, animal dander, fungus, and food allergens and (B) the sensitization rates to the common allergens in the severe atopic dermatitis (AD) group were not significantly different from those in the mild-to-moderate AD group. Der. p., Dermatophagoides pteronyssinus; Der. f., Dermatophagoides farinae. |
Table 1
The clinical characteristics of study subjects

Table 2
Comparison of clinical characteristics and blood eosinophil markers between mild-to-moderate and severe atopic dermatitis subjects
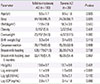
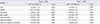
Table 3
Multivariate models for atopic dermatitis and severe atopic dermatitis

Table 4
Multivariate models for atopic dermatitis in boys and girls
References
1. Zhang A, Silverberg JI. Association of atopic dermatitis with being overweight and obese: a systematic review and metaanalysis. J Am Acad Dermatol. 2015; 72:606–616.e4.

2. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Korean J Pediatr. 2008; 51:343–350.

3. Jee HM, Kim KW, Kim CS, Sohn MH, Shin DC, Kim KE. Prevalence of asthma, rhinitis and eczema in Korean children using the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaires. Pediatr Allergy Respir Dis. 2009; 19:165–172.
4. Ahn K, Kim J, Kwon HJ, Chae Y, Hahm MI, Lee KJ, et al. The prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in Korean children: nationwide cross-sectional survey using complex sampling design. J Korean Med Assoc. 2011; 54:769–778.

5. Thomsen SF. Atopic dermatitis: natural history, diagnosis, and treatment. ISRN Allergy. 2014; 2014:354250.

6. Park YM. Epidemiologic study and risk factors of atopic dermatitis. Pediatr Allergy Respir Dis. 2011; 21:74–77.

7. Baek JO, Hong S, Son DK, Lee JR, Roh JY, Kwon HJ. Analysis of the prevalence of and risk factors for atopic dermatitis using an ISAAC questionnaire in 8,750 Korean children. Int Arch Allergy Immunol. 2013; 162:79–85.

8. Lee YM, Hwang SW. Prevalence and risk factors for atopic dermatitis in pre-school and school aged children. J Korean Acad Child Health Nurs. 2008; 14:285–294.
9. Flohr C, Yeo L. Atopic dermatitis and the hygiene hypothesis revisited. Curr Probl Dermatol. 2011; 41:1–34.

10. Kim YM, Kim YC, Lee S, Back JH, Chun K. Association between parental history of allergic diseases and atopic dermatitis in school aged children. Allergy Asthma Respir Dis. 2014; 2:377–382.

11. Son KY, Park KS, Hwang HH, Yun BS, Lee SJ, Kim MA, et al. Prevalence of allergic diseases among primary school children in Ilsan, Gyeonggi and changes of symptoms after environmental control in 2005. Pediatr Allergy Respir Dis. 2007; 17:384–393.
12. Park JS, Kim BJ, Park Y, Lee SY, Kim WK, Kim JE, et al. KAAACI Work Group Report on the treatment of severe/recalcitrant atopic dermatitis. Korean J Asthma Allergy Clin Immunol. 2010; 30:255–270.
13. Na SY, Roh JY, Kim JM, Tamang MD, Lee JR. Analysis of colonization and genotyping of the exotoxins of Staphylococcus aureus in patients with atopic dermatitis. Ann Dermatol. 2012; 24:413–419.

14. US Preventive Services Task Force. Barton M. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010; 125:361–367.

15. Gdalevich M, Mimouni D, David M, Mimouni M. Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. J Am Acad Dermatol. 2001; 45:520–527.

16. Kramer MS, Chalmers B, Hodnett ED, Sevkovskaya Z, Dzikovich I, Shapiro S, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001; 285:413–420.

17. Matheson MC, Allen KJ, Tang ML. Understanding the evidence for and against the role of breastfeeding in allergy prevention. Clin Exp Allergy. 2012; 42:827–851.

18. Yang YW, Tsai CL, Lu CY. Exclusive breastfeeding and incident atopic dermatitis in childhood: a systematic review and meta-analysis of prospective cohort studies. Br J Dermatol. 2009; 161:373–383.

19. Flohr C, Nagel G, Weinmayr G, Kleiner A, Strachan DP, Williams HC, et al. Lack of evidence for a protective effect of prolonged breastfeeding on childhood eczema: lessons from the International Study of Asthma and Allergies in Childhood (ISAAC) phase two. Br J Dermatol. 2011; 165:1280–1289.

20. Munblit D, Boyle RJ, Warner JO. Factors affecting breast milk composition and potential consequences for development of the allergic phenotype. Clin Exp Allergy. 2015; 45:583–601.

21. Baumann S, Lorentz A. Obesity: a promoter of allergy? Int Arch Allergy Immunol. 2013; 162:205–213.
22. Murray CS, Canoy D, Buchan I, Woodcock A, Simpson A, Custovic A. Body mass index in young children and allergic disease: gender differences in a longitudinal study. Clin Exp Allergy. 2011; 41:78–85.

23. Kusunoki T, Morimoto T, Nishikomori R, Heike T, Ito M, Hosoi S, et al. Obesity and the prevalence of allergic diseases in schoolchildren. Pediatr Allergy Immunol. 2008; 19:527–534.

24. Silverberg JI, Kleiman E, Lev-Tov H, Silverberg NB, Durkin HG, Joks R, et al. Association between obesity and atopic dermatitis in childhood: a case-control study. J Allergy Clin Immunol. 2011; 127:1180–1186.e1.
25. Nino M, Franzese A, Ruggiero Perrino N, Balato N. The effect of obesity on skin disease and epidermal permeability barrier status in children. Pediatr Dermatol. 2012; 29:567–570.

26. Gorgievska-Sukarovska B, Lipozencić J, Susac A. Obesity and allergic diseases. Acta Dermatovenerol Croat. 2008; 16:231–235.
27. Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003; 112:1796–1808.

28. Silverberg JI, Greenland P. Eczema and cardiovascular risk factors in 2 US adult population studies. J Allergy Clin Immunol. 2015; 135:721–728.e6.

29. Mitchell EA, Beasley R, Björkstén B, Crane J, García-Marcos L, Keil U, et al. The association between BMI, vigorous physical activity and television viewing and the risk of symptoms of asthma, rhinoconjunctivitis and eczema in children and adolescents: ISAAC Phase Three. Clin Exp Allergy. 2013; 43:73–84.

30. Lam QL, Lu L. Role of leptin in immunity. Cell Mol Immunol. 2007; 4:1–13.
31. Nagel G, Koenig W, Rapp K, Wabitsch M, Zoellner I, Weiland SK. Associations of adipokines with asthma, rhinoconjunctivitis, and eczema in German schoolchildren. Pediatr Allergy Immunol. 2009; 20:81–88.

32. Bostanci I, Atli O, Celebi N, Taşar A, Alpkarakoç E, Dallar Y. Serum leptin level in children with atopic dermatitis-treated topical steroids. Pediatr Allergy Immunol. 2004; 15:267–269.

34. Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. 1999. Biochem Biophys Res Commun. 2012; 425:560–564.

35. Koo H, Lee SM, Lee SP, Han E. Association of body mass index with asthma, allergy rhinitis, and atopic dermatitis among adolescents in Incheon, South Korea. Allergy Asthma Respir Dis. 2014; 2:243–250.

36. Ricci G, Patrizi A, Baldi E, Menna G, Tabanelli M, Masi M. Long-term follow-up of atopic dermatitis: retrospective analysis of related risk factors and association with concomitant allergic diseases. J Am Acad Dermatol. 2006; 55:765–771.

37. Ben-Gashir MA, Seed PT, Hay RJ. Predictors of atopic dermatitis severity over time. J Am Acad Dermatol. 2004; 50:349–356.

38. Kim HY, Seo JH, Jung YH, Lee E, Yang SI, Ha M, et al. Sensitization rates to inhalant allergens in children and adolescents of Incheon and Asan area and the relationship between polysensitization and prevalence of allergic diseases. Allergy Asthma Respir Dis. 2013; 1:41–49.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download