Abstract
Purpose
Breast-feeding is recommended to prevent allergies, particularly in high-risk infants, but the evidence of protective effects that breast-feeding has on food allergy (FA) remains elusive. The aim of this study was to investigate risk factors of FA and the association between breast-feeding and FA symptoms/food sensitization (FS) in children with atopic dermatitis under 2 years of age.
Methods
We reviewed the medical records of 384 children with atopic dermatitis under 2 years of age who visited our pediatric allergy clinic from March 1, 2009 through December 31, 2014. Symptoms of FA, feeding type, and family history of allergic disease were assessed. Laboratory tests were conducted, including serum total IgE, eosinophil (%), serum 25-hydroxyvitamin D, and specific IgE to egg white, milk, soy, peanut, and wheat.
Results
Subjects were divided into 3 groups based on FA symptoms and evidence of sensitization: The FA symptom group (n=240), no symptom group (n=53) and no FS group (n=91). The FA symptom group had a higher log total IgE level (2.0 vs. 1.3, P<0.001) and eosinophil (%) (7.0% vs. 4.7%, P=0.001) than the no FA symptom group. In multivariate analysis, breast-feeding was associated with FS (adjusted odds ratio [aOR], 2.43; 95% confidence intervals [CI], 1.03–5.74) but was not associated with FA symptoms (aOR, 0.65; 95% CI, 0.23–1.83).
Figures and Tables
Table 1
Comparison of study subject characteristics
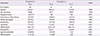
Table 2
Comparison of characteristics between study subgroups

Table 3
Risk factors for food sensitization among infants with atopic dermatitis
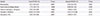
Table 4
Risk factors for food allergy symptoms among infants with atopic dermatitis
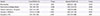
Table 5
Risk of breast feeding for food allergy symptom and food sensitization in subgroup analysis

References
2. Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011; 128:e9–e17.

3. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Korean J Pediatr. 2008; 51:343–350.

4. Oh JW, Pyun BY, Choung JT, Ahn KM, Kim CH, Song SW, et al. Epidemiological change of atopic dermatitis and food allergy in school-aged children in Korea between 1995 and 2000. J Korean Med Sci. 2004; 19:716–723.

5. Kumar R. Epidemiology and risk factors for the development of food allergy. Pediatr Ann. 2008; 37:552–558.

7. Eggesbo M, Botten G, Stigum H, Nafstad P, Magnus P. Is delivery by cesarean section a risk factor for food allergy? J Allergy Clin Immunol. 2003; 112:420–426.

8. Grulee CG, Sanford HN. The influence of breast and artificial feeding oninfantile eczema. J Pediatr. 1936; 9:223–225.

9. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012; 129:e827–e841.
10. Thygarajan A, Burks AW. American Academy of Pediatrics recommendations on the effects of early nutritional interventions on the development of atopic disease. Curr Opin Pediatr. 2008; 20:698–702.

11. Ehlayel MS, Bener A. Duration of breast-feeding and the risk of childhood allergic diseases in a developing country. Allergy Asthma Proc. 2008; 29:386–391.

12. Dell S, To T. Breastfeeding and asthma in young children: findings from a population-based study. Arch Pediatr Adolesc Med. 2001; 155:1261–1265.
13. Saarinen UM, Kajosaari M. Breastfeeding as prophylaxis against atopic disease: prospective follow-up study until 17 years old. Lancet. 1995; 346:1065–1069.

14. Chulada PC, Arbes SJ Jr, Dunson D, Zeldin DC. Breast-feeding and the prevalence of asthma and wheeze in children: analyses from the Third National Health and Nutrition Examination Survey, 1988-1994. J Allergy Clin Immunol. 2003; 111:328–336.

15. Kull I, Melen E, Alm J, Hallberg J, Svartengren M, van Hage M, et al. Breast-feeding in relation to asthma, lung function, and sensitization in young schoolchildren. J Allergy Clin Immunol. 2010; 125:1013–1019.

16. Giwercman C, Halkjaer LB, Jensen SM, Bonnelykke K, Lauritzen L, Bisgaard H. Increased risk of eczema but reduced risk of early wheezy disorder from exclusive breast-feeding in high-risk infants. J Allergy Clin Immunol. 2010; 125:866–871.

17. Sears MR, Greene JM, Willan AR, Taylor DR, Flannery EM, Cowan JO, et al. Long-term relation between breastfeeding and development of atopy and asthma in children and young adults: a longitudinal study. Lancet. 2002; 360:901–907.

18. Pesonen M, Kallio MJ, Ranki A, Siimes MA. Prolonged exclusive breastfeeding is associated with increased atopic dermatitis: a prospective follow-up study of unselected healthy newborns from birth to age 20 years. Clin Exp Allergy. 2006; 36:1011–1018.

19. Duncan JM, Sears MR. Breastfeeding and allergies: time for a change in paradigm? Curr Opin Allergy Clin Immunol. 2008; 8:398–405.

20. Hill DJ, Hosking CS, de Benedictis FM, Oranje AP, Diepgen TL, Bauchau V, et al. Confirmation of the association between high levels of immunoglobulin E food sensitization and eczema in infancy: an international study. Clin Exp Allergy. 2008; 38:161–168.

21. Eigenmann PA, Sicherer SH, Borkowski TA, Cohen BA, Sampson HA. Prevalence of IgE-mediated food allergy among children with atopic dermatitis. Pediatrics. 1998; 101:E8.

22. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta derm venereol (Stockh). 1980; 92:44–47.
23. Baker S, Cochran W, Greer F, Heyman M, Jacobson M, Jaksic T, et al. Hypoallergenic infant formulas. Pediatrics. 2000; 106:346–349.

24. Greer FR, Sicherer SH, Burks AW. American Academy of Pediatrics Committee on Nutrition. American Academy of Pediatrics Section on Allergy and Immunology. Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2008; 121:183–191.

25. Strid J, Thomson M, Hourihane J, Kimber I, Strobel S. A novel model of sensitization and oral tolerance to peanut protein. Immunology. 2004; 113:293–303.

26. Poole JA, Barriga K, Leung DY, Hoffman M, Eisenbarth GS, Rewers M, et al. Timing of initial exposure to cereal grains and the risk of wheat allergy. Pediatrics. 2006; 117:2175–2182.

27. Kilshaw PJ, Cant AJ. The passage of maternal dietary proteins into human breast milk. Int Arch Allergy Appl Immunol. 1984; 75:8–15.

28. Vadas P, Wai Y, Burks W, Perelman B. Detection of peanut allergens in breast milk of lactating women. JAMA. 2001; 285:1746–1748.

29. Han YS, Chung SJ, Ahn KM, Lee KS, Choi HM, Lee SI. Sensitization of food allergen in breastfed infant with atopic dermatitis. Korean J Community Nutr. 2005; 10:264–270.
30. Chehade M, Mayer L. Oral tolerance and its relation to food hypersensitivities. J Allergy Clin Immunol. 2005; 115:3–12.

31. Mowat AM. Anatomical basis of tolerance and immunity to intestinal antigens. Nat Rev Immunol. 2003; 3:331–341.

32. Verhasselt V. Neonatal tolerance under breastfeeding influence. Curr Opin Immunol. 2010; 22:623–630.

33. Verhasselt V, Milcent V, Cazareth J, Kanda A, Fleury S, Dombrowicz D, et al. Breast milk-mediated transfer of an antigen induces tolerance and protection from allergic asthma. Nat Med. 2008; 14:170–175.

34. Kalliomaki M, Ouwehand A, Arvilommi H, Kero P, Isolauri E. Transforming growth factor-beta in breast milk: a potential regulator of atopic disease at an early age. J Allergy Clin Immunol. 1999; 104:1251–1257.
35. Oddy WH, Halonen M, Martinez FD, Lohman IC, Stern DA, Kurzius-Spencer M, et al. TGF-beta in human milk is associated with wheeze in infancy. J Allergy Clin Immunol. 2003; 112:723–728.
36. Rubaltelli FF, Biadaioli R, Pecile P, Nicoletti P. Intestinal flora in breast- and bottle-fed infants. J Perinat Med. 1998; 26:186–191.

37. Lowe AJ, Carlin JB, Bennett CM, Abramson MJ, Hosking CS, Hill DJ, et al. Atopic disease and breast-feeding: cause or consequence? J Allergy Clin Immunol. 2006; 117:682–687.
38. Noh G, Lee JH. Revision of immunopathogenesis and laboratory interpretation for food allergy in atopic dermatitis. Inflamm Allergy Drug Targets. 2012; 11:20–35.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download