Abstract
Purpose
This study was performed to investigate the indications, yield, and complications of flexible bronchoscopy for respiratory disease in children compared to earlier domestic studies and to examine if any differences existed in comparison to international studies.
Methods
The medical records of 100 cases of flexible bronchoscopy that were performed in 76 patients at the Department of Pediatrics of The Catholic University of Korea, Seoul St. Mary's Hospital from June 16, 2010 to August 6, 2013 were reviewed.
Results
A total of 76 patients (50 males and 26 females) were included in the study. The most common indication of flexible bronchoscopy was persistent pneumonia or pneumonia in immunocompromised patients (53 cases). The object of flexible bronchoscopy was accomplished in 65 of 100 cases, and, the treatment was changed in 24 of 65 cases. The most common abnormal finding was tracheomalacia that was found in 18 cases. In 67 cases where bronchoalveolar lavage was performed, bacteria were identified in 47 cases, fungi in 9 cases, and viruses in 22 cases. Complications occurred in 8 cases.
Conclusion
Compared to earlier domestic studies, there was no significant change in diagnostic approaches and therapeutic improvement. However, this study showed that flexible bronchoscopy appears to be safe in patients with hemato-oncologic disease. Compared to international studies, the occurrence of complications due to flexible bronchoscopy was relatively low.
Figures and Tables
Table 1
Characteristics of patients (n=76, case=100)

Table 2
Indication for pediatric flexible bronchoscopy (case=100)

Table 3
Yield of pediatric bronchoscopy (case=100)

Table 4
Bronchoscopic finding of patients (case=100)

Table 5
Cultured pathogens of bronchoalveolar lavage and bronchoscopic washing (case=68)

Table 6
Complications during the Procedure (case=100)
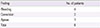
| Finding | No. of patients |
|---|---|
| Bleeding | 4 |
| Convulsion | 3 |
| Apnea | 1 |
| Total | 8 |
Table 7
Characteristics of main studies reporting pediatric bronchoscopy

| Characteristic | Current study | Moon et al.7 | Ahn et al.8 | Peng et al.14 | Manna and Durward11 |
|---|---|---|---|---|---|
| Country | South Korea | South Korea | South Korea | Taiwan | United Kingdom |
| Study period | 3 yr (2010-2013) | 3 yr (2007-2010) | 7 yr (2001-2008) | 4 yr (2005-2009) | 2 yr (2002-2004) |
| Design | Retrospective | Retrospective | Retrospective | Retrospective | Retrospective |
| Age | 7 day-18 yr | 5 day-18 yr | 0-18 yr | 1 day-17.5 yr | 4 mo-6 yr |
| Single/multicenter | Single center | Single center | Single center | Single center | single center |
| Bronchoscopic case | 100 | 100 | 105 | 725 | 148 |
| Indications | Persistent pneumonia; stridor; persistent atelectasis; BAL; foreign body aspiration; Hemoptysis; wheezing | Anatomic evaluation; respiratory distress; BAL; persistent atelectasis; extubation failure; foreign body aspiration; hemoptysis | BAL; anatomic evaluation; respiratory distress; persistent atelectasis; foreign body aspiration; hemoptysis | Anatomic evaluation; BAL; intubation; respiratory distress | Anatomic evaluation; atelectasis; BAL; extubation failure; hemorrhage |
| Diagnostic yield | Overall: 65.0% (65/100): change in medical management: 36.9% (24/65) | Overall: 67.0% (67/100): change in management: 50.7% (34/67) | Overall: 62.9% (66/105) | Overall:87.2% (312/358): airway malacia: 47.8% (171/358): inflammatory changes: 39.4% (141/358) | Overall:76.4% (113/148): upper airway: 84.4% (27/32); lower airway: 80.0% (56/70): CHD identified extraluminal compression: 18.6% (13/70): extubation failure: 90.5% (19/21): pulmonary disease: 44.0% (11/25) |
| Diagnostic BAL findings | Identified organism: 67.6% (46/68) | Identified organism: 63.3% (38/60) | Identified organism: 44.7% (17/38) | Identified organism: 35.3% (6/17) | |
| Therapeutic outcomes | Re-expanded collapsed lobe: 66.7% (6/9) | Re-expanded collapsed lobe: 72.7% (8/11) | Re-expanded collapsed lobe: 64.2% (9/14) | 71.4% (518/725) of all FFB were interventional. | Re-expanded collapsed lobe: 92.3% (24/26) |
| Complication | Bleeding: 4.0% (4/100); convulsion: 3.0% (3/100); apnea: 1.0% (1/100) | Fever: 4.0% (4/100); convulsion: 3.0% (3/100); dyspnea: 2.0% (2/100); bleeding: 1.0% (1/100); hypotension: 1.0% (1/100); vomiting: 1.0% (1/100) | Bleeding: 3.8% (4/105); bronchospasm: 1.9% (2/105); fever: 1.0% (1/105); desaturation: 1.0% (1/105) | Laryngospasm: 0.8% (6/725); pneumothorax: 0.3% (2/725); fever; 29.5% (214/725) | Transient hypoxia: 10.8% (16/148); hypoxia of ARDS patients: 16.7% (3/18); hypotension: 17.6% (26/148); rigid chest after fentanyl: 0.6% (1/148) |
References
1. Wood RE, Fink RJ. Applications of flexible fiberoptic bronchoscopes in infants and children. Chest. 1978; 73:5 Suppl. 737–740.

2. Barbato A, Magarotto M, Crivellaro M, Novello A Jr, Cracco A, de Blic J, et al. Use of the paediatric bronchoscope, flexible and rigid, in 51 European centres. Eur Respir J. 1997; 10:1761–1766.

3. Nussbaum E. Flexible fiberoptic bronchoscopy and laryngoscopy in infants and children. Laryngoscope. 1983; 93:1073–1075.

4. Tang LF, Chen ZM. Fiberoptic bronchoscopy in neonatal and pediatric intensive care units: a 5-year experience. Med Princ Pract. 2009; 18:305–309.

5. Wood RE. Pitfalls in the use of the flexible bronchoscope in pediatric patients. Chest. 1990; 97:199–203.

6. Rodrigues AJ, Scussiatto EA, Jacomelli M, Scordamaglio PR, Gregorio MG, Palomino AL, et al. Bronchoscopic techniques for removal of foreign bodies in children's airways. Pediatr Pulmonol. 2012; 47:59–62.

7. Moon CJ, Lee EJ, Chun YH, Yoon JS, Kim HH, Lee JS. Pediatric flexible bronchoscopy: clinical experience of 100 cases of bronchoscopy from a single institute. Pediatr Allergy Respir Dis. 2011; 21:313–318.

8. Ahn HS, Choi EJ, Yun HJ, Wang SW, Kwon EY, Hwang KG, et al. The clinical experience of pediatric flexible bronchoscopy at a single institution. Pediatr Allergy Respir Dis. 2011; 21:226–233.

9. Field-Ridley A, Sethi V, Murthi S, Nandalike K, Li ST. Utility of flexible fiberoptic bronchoscopy for critically ill pediatric patients: a systematic review. World J Crit Care Med. 2015; 4:77–88.

10. de Blic J, Marchac V, Scheinmann P. Complications of flexible bronchoscopy in children: prospective study of 1,328 procedures. Eur Respir J. 2002; 20:1271–1276.

11. Manna SS, Durward A, Moganasundram S, Tibby SM, Murdoch IA. Retrospective evaluation of a paediatric intensivist-led flexible bronchoscopy service. Intensive Care Med. 2006; 32:2026–2033.

12. Bar-Zohar D, Sivan Y. The yield of flexible fiberoptic bronchoscopy in pediatric intensive care patients. Chest. 2004; 126:1353–1359.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download