This article has been corrected. See "ERRATUM: Author's English name correction. A single hospital survey of anaphylaxis awareness among health care providers and medical students" in Volume 4 on page 231.
Abstract
Purpose
Anaphylaxis is a rapidly progressive allergic reaction that requires precise recognition and immediate management. However, health care providers, awareness of anaphylaxis has not been acknowledged. The aim of this study is to investigate the extent of knowledge and principal management skills on anaphylaxis among medical personnel and students.
Methods
We performed a questionnaire survey on knowledge, education, and managing skills for anaphylaxis to physicians, nurses, health personnel, and medical students in Ajou University Medical Center, from 26 June to 31 October, 2014. The survey contained 2 main sections: questions about demographic data and 2 types of questionnaire (type I for all participants and type II for only medical staffs) for self-assessment on anaphylaxis.
Results
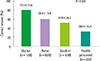
A total of 1,615 participants (128 doctors, 828 nurses, 436 students, and 223 health personnel) completed the survey. For questionnaire I, the percentages of correct answers in doctors, nurses, medical students, and health personnel were 77.5%, 56.4%, 47.8%, and 28.0% respectively, showing significant differences between groups (P<0.001). For questionnaire II, 93% of doctors and 75.6% of nurses indicated epinephrine as the drug of choice, and 79.7% of doctors and 71.3% of nurses selected the correct intramuscular route. More than 3 quarters of the doctors (80.5%) selected epinephrine within the first 5 steps of treatment, but only 48% included epinephrine within the first 3 steps.
Conclusion
Our study showed considerable lack of knowledge on anaphylaxis among health care providers, especially on the specific management steps of anaphylaxis. As significant gaps on overall knowledge of anaphylaxis were observed between different groups of medical personnel, regular education should be implemented for each department in the health care setting.
Figures and Tables
 | Fig. 1The percentages of medical staffs who included epinephrine within essential steps of management of anaphylaxis. |
Table 1
Demographic data

Table 2
The percentages of correct answers to questionnaire I

Table 3
The distribution of selection to questions (I4, I7, I8)

Table 4
The percentages of correct answers to questionnaire II

Table 5
The distribution of selection to questions (II5, II7, II8)

Table 6
The results* according to experience of treatment
References
1. Simons FE, Ardusso LR, Bilo MB, Cardona V, Ebisawa M, El-Gamal YM, et al. International consensus on (ICON) anaphylaxis. World Allergy Organ J. 2014; 7:9.

2. Panesar SS, Javad S, de Silva D, Nwaru BI, Hickstein L, Muraro A, et al. The epidemiology of anaphylaxis in Europe: a systematic review. Allergy. 2013; 68:1353–1361.

3. Tejedor Alonso MA, Moro Moro M, Mugica Garcia MV. Epidemiology of anaphylaxis. Clin Exp Allergy. 2015; 45:1027–1039.

5. Lee SY, Kim KW, Lee HH, Lim DH, Chung HL, Kim SW, et al. Incidence and clinical characteristics of pediatric emergency department visits of children with severe food allergy. Korean J Asthma Allergy Clin Immunol. 2012; 32:169–175.
6. Jang GC, Chang YS, Choi SH, Song WJ, Lee SY, Park HS, et al. Overview of anaphylaxis in Korea: diagnosis and management. Allergy Asthma Respir Dis. 2013; 1:181–196.

7. Ye YM, Kim MK, Kang HR, Kim TB, Sohn SW, Koh YI, et al. Predictors of the severity and serious outcomes of anaphylaxis in korean adults: a multicenter retrospective case study. Allergy Asthma Immunol Res. 2015; 7:22–29.

8. Turner PJ, Gowland MH, Sharma V, Ierodiakonou D, Harper N, Garcez T, et al. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992-2012. J Allergy Clin Immunol. 2015; 135:956–963.e1.

9. Koplin JJ, Martin PE, Allen KJ. An update on epidemiology of anaphylaxis in children and adults. Curr Opin Allergy Clin Immunol. 2011; 11:492–496.

10. Ibrahim I, Chew BL, Zaw WW, Van Bever HP. Knowledge of anaphylaxis among Emergency Department staff. Asia Pac Allergy. 2014; 4:164–171.

11. Jung-Wu S. Anaphylaxis knowledge and practice preference of pediatric emergency medicine physicians: a national survey. Pediatrics. 2014; 134:Suppl 3. S148–S149.

12. Grossman SL, Baumann BM, Garcia Pena BM, Linares MY, Greenberg B, Hernandez-Trujillo VP. Anaphylaxis knowledge and practice preferences of pediatric emergency medicine physicians: a national survey. J Pediatr. 2013; 163:841–846.

13. Jacobsen RC, Toy S, Bonham AJ, Salomone JA 3rd, Ruthstrom J, Gratton M. Anaphylaxis knowledge among paramedics: results of a national survey. Prehosp Emerg Care. 2012; 16:527–534.

14. Baccıoglu A, Yılmazel Ucar E. Level of knowledge about anaphylaxis among health care providers. Tuberk Toraks. 2013; 61:140–146.

15. Droste J, Narayan N. Hospital doctors' knowledge of adrenaline (epinephrine) administration in anaphylaxis in adults is deficient. Resuscitation. 2010; 81:1057–1058.

16. Jeong JW, Park CS, Jung JW, Park HK, Kim SH, Kim TB, et al. Anaphylaxis: hospital doctors' knowledge of management guidelines. J Allergy Clin Immunol. 2013; 131:AB221.

17. Anaphylaxis quiz [Internet]. Milwaukee (WI): American Academy of Allergy, Asthma & Immunology;c2016. cited 2014 Jun 1. Available from: http://www.aaaai.org/conditions-and-treatments/allergies/anaphylaxis/anaphylaxis-quiz.aspx.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download