Abstract
Purpose
Although allergic disease has been recognized as a common chronic disease related to the sleep disturbance of children, studies on sleep disturbance in children with allergic disease are scanty in Korea. The aim of this study was to evaluate the sleep disturbance of children with allergic disease.
Methods
Children aged 2 to 12 years were assessed using the sleep questionnaires. From July 2011 to June 2012, surveys were conducted on patients who were diagnosed with allergies in 3 general hospitals and in an elementary school in Seoul and the capital area. The analysis was done in 3 groups according to age.
Results
The sleep questionnaires of 1,174 children were evaluated. Children with allergic disease were 341 (209 males and 132 females) and those in the control group were 833 (428 males and 405 females). Parasomnia symptoms were common in young children (ages 2 to 5 years) than in the control group (P<0.05). Symptoms of sleep-disordered breathing were more common in early adolescent children (ages 11 to 12 years) than in the control group (P<0.05). The presence of allergic rhinitis, gender, and body mass index did not correlate with a sleep disturbance in children with allergic disease.
Conclusion
To our knowledge, this study was the first report of sleep disturbance in children with allergic disease in Korea. This study suggests that children with allergic disease from early children may have poor sleep quality than those without. Therefore, proper treatment of and great interest in sleep disturbance are required for children with allergic disease.
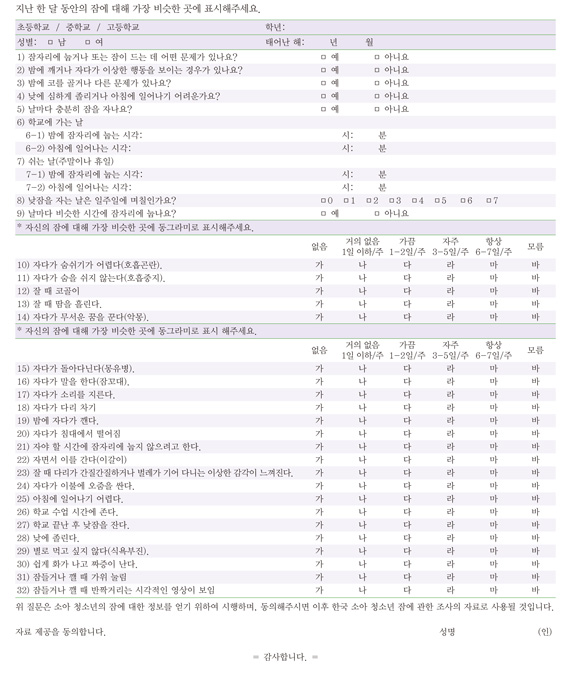
Figures and Tables
Table 1
Demographic informations of the participants

Table 2
Comparison of sleep schedules between allergy group and control group

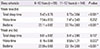
Table 3
Comparison of sleep disturbance and symptoms between allergy group and control group

Values are presented as mean±standard deviation.
*P<0.05. †Sum of score of number 1-5 in sleep questionnaires (score 0-5). ‡Sum of score of number 10-13 in sleep questionnaires (score 0-16). §Sum of score of number 14-20 in sleep questionnaires (score 0-28).∥Sum of score of number 25-28 in sleep questionnaires (score 0-16).
Table 4
Comparison of sleep schedules between children with allergic rhinitis and children without allergic rhinitis in allergy group aged 6-12 years
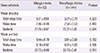
Table 5
Comparison of sleep schedules of children with allergic diseases between ages 6-10 and 11-12 years
References
1. Mindell JA, Owens JA. A clinical guide to pediatric sleep: diagnosis and management of sleep problems. Philadelphia: Lippincott Williams & Wilkins;2009.
2. Stores G, Wiggs L. Sleep disturbance in children and adolescents with disorders of development: its significance and management. London: Cambridge University Press;2001. p. 3–8.
3. Wiggs L, Stores G. Severe sleep disturbance and daytime challenging behaviour in children with severe learning disabilities. J Intellect Disabil Res. 1996; 40(Pt 6):518–528.

4. Kaplan BJ, McNicol J, Conte RA, Moghadam HK. Sleep disturbance in preschool-aged hyperactive and nonhyperactive children. Pediatrics. 1987; 80:839–844.

5. Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001; 107:E60.

6. Seo WS, Koo BH, Kim MJ, Rho YH, Sung HM, Shin JH. Preliminary study of children's sleep problems in an elementary school in Daegu. J Korean Acad Child Adolesc Psychiatry. 2008; 19:156–161.
7. Owens J. Classification and epidemiology of childhood sleep disorders. Prim Care. 2008; 35:533–546.

8. van Litsenburg RR, Waumans RC, van den Berg G, Gemke RJ. Sleep habits and sleep disturbances in Dutch children: a population-based study. Eur J Pediatr. 2010; 169:1009–1015.

9. Meltzer LJ, Moore M. Sleep disruptions in parents of children and adolescents with chronic illnesses: prevalence, causes, and consequences. J Pediatr Psychol. 2008; 33:279–291.

10. Li AM, So HK, Au CT, Ho C, Lau J, Ng SK, et al. Epidemiology of obstructive sleep apnoea syndrome in Chinese children: a two-phase community study. Thorax. 2010; 65:991–997.

11. Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol. 2000; 36:291–301.

12. Zamir G, Press J, Tal A, Tarasiuk A. Sleep fragmentation in children with juvenile rheumatoid arthritis. J Rheumatol. 1998; 25:1191–1197.
14. Desager KN, Nelen V, Weyler JJ, De Backer WA. Sleep disturbance and daytime symptoms in wheezing school-aged children. J Sleep Res. 2005; 14:77–82.

15. Fitzpatrick MF, Martin K, Fossey E, Shapiro CM, Elton RA, Douglas NJ. Snoring, asthma and sleep disturbance in Britain: a community-based survey. Eur Respir J. 1993; 6:531–535.
16. Madge PJ, Nisbet L, McColl JH, Vallance A, Paton JY, Beattie JO. Home nebuliser use in children with asthma in two Scottish Health Board Areas. Scott Med J. 1995; 40:141–143.

17. Craig TJ, Teets S, Lehman EB, Chinchilli VM, Zwillich C. Nasal congestion secondary to allergic rhinitis as a cause of sleep disturbance and daytime fatigue and the response to topical nasal corticosteroids. J Allergy Clin Immunol. 1998; 101:633–637.

18. Bender BG, Leung SB, Leung DY. Actigraphy assessment of sleep disturbance in patients with atopic dermatitis: an objective life quality measure. J Allergy Clin Immunol. 2003; 111:598–602.

19. Baiardini I, Braido F, Cauglia S, Canonica GW. Sleep disturbances in allergic diseases. Allergy. 2006; 61:1259–1267.

20. Park YS, Lee DH, Choi JM, Kang YJ, Kim CH. Trend of obesity in school age children in Seoul over the past 23 years. Korean J Pediatr. 2004; 47:247–257.
21. Petit D, Touchette E, Tremblay RE, Boivin M, Montplaisir J. Dyssomnias and parasomnias in early childhood. Pediatrics. 2007; 119:e1016–e1025.

22. Kim YH, Lee JS, Kim HD, Cho YJ, Kang JH, Lee JC, et al. Clinical evaluation of sleep disorders in childhood and adolescence. J Korean Child Neurol Soc. 2010; 18:187–196.
23. Laberge L, Tremblay RE, Vitaro F, Montplaisir J. Development of parasomnias from childhood to early adolescence. Pediatrics. 2000; 106(1 Pt 1):67–74.

25. Gozal D. Obstructive sleep apnea in children. Minerva Pediatr. 2000; 52:629–639.
27. Capdevila OS, Kheirandish-Gozal L, Dayyat E, Gozal D. Pediatric obstructive sleep apnea: complications, management, and long-term outcomes. Proc Am Thorac Soc. 2008; 5:274–282.

28. Bhattacharjee R, Kheirandish-Gozal L, Pillar G, Gozal D. Cardiovascular complications of obstructive sleep apnea syndrome: evidence from children. Prog Cardiovasc Dis. 2009; 51:416–433.

29. Quintana-Gallego E, Carmona-Bernal C, Capote F, Sanchez-Armengol A, Botebol-Benhamou G, Polo-Padillo J, et al. Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med. 2004; 98:984–989.

30. Lazaratou H, Dikeos DG, Anagnostopoulos DC, Sbokou O, Soldatos CR. Sleep problems in adolescence. A study of senior high school students in Greece. Eur Child Adolesc Psychiatry. 2005; 14:237–243.

31. Kohler MJ, van den Heuvel CJ. Is there a clear link between overweight/obesity and sleep disordered breathing in children? Sleep Med Rev. 2008; 12:347–361.

32. Hadley JA, Derebery MJ, Marple BF. Comorbidities and allergic rhinitis: not just a runny nose. J Fam Pract. 2012; 61:2 Suppl. S11–S15.
33. Cibella F, Cuttitta G. Nocturnal asthma and gastroesophageal reflux. Am J Med. 2001; 111:Suppl 8A. 31S–36S.

34. Sheldon SH, Ferber R, Kryger MH. Principles and practice of pediatric sleep medicine. Philadelphia: Elsevier Health Sciences;2005. p. 179–194.
35. Alkhalil M, Schulman E, Getsy J. Obstructive sleep apnea syndrome and asthma: what are the links? J Clin Sleep Med. 2009; 5:71–78.

36. Yoon HK, Kang SG, Lee HJ, Yoo Y, Choung JT, Seo WH, et al. Apnea-related sleep fragmentation and poor vigilance in children with well-controlled asthma. J Sleep Res. 2013; 11. [Epub]. http://dx.doi.org/10.1111/jsr.12103.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download