Abstract
Purpose
Vascular endothelial growth factor (VEGF), transforming growth factor beta1 (TGF-β1), and platelet derived growth factor (PDGF) are known to be involved in the pathogenesis of inflammation and remodeling in asthmatic airways. YKL-40, a chitinase-like protein, and clusterin have been reported to be biomarkers for severe asthma. We examined the serum levels of growth factors, YKL-40, and clusterin in children with acute asthma or stable asthma, and investigated their correlation with clinical findings and lung function parameters.
Methods
Forty-one children (≥6 years of age) with asthma were enrolled, and 2 groups were defined: 23 patients admitted with acute asthma (acute asthma group) and 18 patients with stable asthma (stable asthma group). The serum levels of VEGF, TGF-β1, PDGF-BB, YKL-40, and clusterin were measured using enzyme-linked immunosorbent assay and assessed in relation to clinical manifestations and spirometric parameters. Fifteen age-matched controls were also studied.
Results
The serum levels of VEGF, TGF-β1, and YKL-40 were significantly elevated in children with acute asthma compared to controls. The serum levels of VEGF and YKL-40 were higher in the stable asthma group than in controls. The serum levels of VEGF, TGF-β1, and YKL-40 were not different between the acute asthma and stable asthma groups. The serum VEGF levels in the acute asthma group correlated significantly with asthma severity. The serum TGF-β1 levels in stable asthma group showed a significant inverse correlation with (FEV1) forced expiratory volume in one second and FEF25%-75% (forced expiratory flow between 25 and 75 percent of expired vital capacity). Serum YKL-40 had no significant relationship with clinical manifestations and spirometric parameters.
Figures and Tables
 | Fig. 1Serum VEGF (A), TGF-β1 (B), PDGF-BB (C), YKL-40 (D), and clusterin (E) levels in acute and stable asthma groups, and controls. VEGF, vascular endothelial growth factor; TGF-β1, transforming growth factor beta1; PDGF, platelet derived growth factor. |
Table 1
Characteristics of the patients from two asthma groups

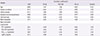
Table 2
Correlation between clinical parameters and serum levels of growth factors, YKL-40, and clusterin in acute asthma group
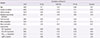
Table 3
Correlation between clinical parameters and serum levels of growth factors, YKL-40, and clusterin in stable asthma group
References
1. Detoraki A, Granata F, Staibano S, Rossi FW, Marone G, Genovese A. Angiogenesis and lymphangiogenesis in bronchial asthma. Allergy. 2010; 65:946–958.

2. Meyer N, Akdis CA. Vascular endothelial growth factor as a key inducer of angiogenesis in the asthmatic airways. Curr Allergy Asthma Rep. 2013; 13:1–9.

3. Willis BC, Borok Z. TGF-beta-induced EMT: mechanisms and implications for fibrotic lung disease. Am J Physiol Lung Cell Mol Physiol. 2007; 293:L525–L534.
4. Nishioka Y, Azuma M, Kishi M, Aono Y. Targeting platelet-derived growth factor as a therapeutic approach in pulmonary fibrosis. J Med Invest. 2013; 60:175–183.

5. Mukherjee S, Duan F, Kolb MR, Janssen LJ. Platelet derived growth factor-evoked Ca2+ wave and matrix gene expression through phospholipase C in human pulmonary fibroblast. Int J Biochem Cell Biol. 2013; 45:1516–1524.

6. Burgess JK. The role of the extracellular matrix and specific growth factors in the regulation of inflammation and remodelling in asthma. Pharmacol Ther. 2009; 122:19–29.

7. Honkova L, Uhlik J, Berankova K, Svobodova T, Pohunek P. Epithelial basement membrane thickening is related to TGF-Beta 1 expression in children with chronic respiratory diseases. Pediatr Allergy Immunol. 2014; 25:593–599.

8. Gagliardo R, Chanez P, Gjomarkaj M, La Grutta S, Bonanno A, Montalbano AM, et al. The role of transforming growth factor-β1 in airway inflammation of childhood asthma. Int J Immunopathol Pharmacol. 2013; 26:725–738.

9. Papadaki G, Bakakos P, Kostikas K, Hillas G, Tsilogianni Z, Koulouris NG, et al. Vascular endothelial growth factor and cysteinyl leukotrienes in sputum supernatant of patients with asthma. Respir Med. 2013; 107:1339–1345.

10. Lee CG, Da Silva CA, Dela Cruz CS, Ahangari F, Ma B, Kang MJ, et al. Role of chitin and chitinase/chitinase-like proteins in inflammation, tissue remodeling, and injury. Annu Rev Physiol. 2011; 73:479–501.

11. Chupp GL, Lee CG, Jarjour N, Shim YM, Holm CT, He S, et al. A chitinase-like protein in the lung and circulation of patients with severe asthma. N Engl J Med. 2007; 357:2016–2027.

12. Konradsen JR, James A, Nordlund B, Reinius LE, Soderhall C, Melen E, et al. The chitinase-like protein YKL-40: a possible biomarker of inflammation and airway remodeling in severe pediatric asthma. J Allergy Clin Immunol. 2013; 132:328–335.e5.
13. Kwon HS, Kim TB, Lee YS, Jeong SH, Bae YJ, Moon KA, et al. Clusterin expression level correlates with increased oxidative stress in asthmatics. Ann Allergy Asthma Immunol. 2014; 112:217–221.

14. Malmström K, Pelkonen AS, Makela MJ. Remodeling, inflammation and airway responsiveness in early childhood asthma. Curr Opin Allergy Clin Immunol. 2013; 13:203–210.

15. Chung HL, Lee EJ, Park HJ, Lee KH. Increased epidermal growth factor in nasopharyngeal aspirates from infants with recurrent wheeze. Pediatr Pulmonol. 2015; 50:841–847.

16. National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007; 120:5 Suppl. S94–S138.
17. Barbato A, Turato G, Baraldo S, Bazzan E, Calabrese F, Panizzolo C, et al. Epithelial damage and angiogenesis in the airways of children with asthma. Am J Respir Crit Care Med. 2006; 174:975–981.

18. Hoshino M, Takahashi M, Aoike N. Expression of vascular endothelial growth factor, basic fibroblast growth factor, and angiogenin immunoreactivity in asthmatic airways and its relationship to angiogenesis. J Allergy Clin Immunol. 2001; 107:295–301.

19. Asai K, Kanazawa H, Kamoi H, Shiraishi S, Hirata K, Yoshikawa J. Increased levels of vascular endothelial growth factor in induced sputum in asthmatic patients. Clin Exp Allergy. 2003; 33:595–599.

20. Zou H, Fang QH, Ma YM, Wang XY. Analysis of growth factors in serum and induced sputum from patients with asthma. Exp Ther Med. 2014; 8:573–578.

21. Lee KY, Lee KS, Park SJ, Kim SR, Min KH, Choe YH, et al. Clinical significance of plasma and serum vascular endothelial growth factor in asthma. J Asthma. 2008; 45:735–739.

22. Abdel-Rahman AM, el-Sahrigy SA, Bakr SI. A comparative study of two angiogenic factors: vascular endothelial growth factor and angiogenin in induced sputum from asthmatic children in acute attack. Chest. 2006; 129:266–271.
23. Moore B, Murphy RF, Agrawal DK. Interaction of tgf-beta with immune cells in airway disease. Curr Mol Med. 2008; 8:427–436.
24. Karagiannidis C, Hense G, Martin C, Epstein M, Ruckert B, Mantel PY, et al. Activin A is an acute allergen-responsive cytokine and provides a link to TGF-beta-mediated airway remodeling in asthma. J Allergy Clin Immunol. 2006; 117:111–118.

25. Brown SD, Baxter KM, Stephenson ST, Esper AM, Brown LA, Fitzpatrick AM. Airway TGF-β1 and oxidant stress in children with severe asthma: association with airflow limitation. J Allergy Clin Immunol. 2012; 129:388–396. 396.e1–396.e8.

26. Jiang K, Chen HB, Wang Y, Lin JH, Hu Y, Fang YR. Changes in IL-17 and TGF-β1 levels in serum and bronchoalveolar lavage fluid and their clinical significance among children with asthma. Zhongguo Dang Dai Er Ke Za Zhi. 2013; 15:604–608.
27. Bara I, Ozier A, Girodet PO, Carvalho G, Cattiaux J, Begueret H, et al. Role of YKL-40 in bronchial smooth muscle remodeling in asthma. Am J Respir Crit Care Med. 2012; 185:715–722.

28. Santos CB, Davidson J, Covar RA, Spahn JD. The chitinase-like protein YKL-40 is not a useful biomarker for severe persistent asthma in children. Ann Allergy Asthma Immunol. 2014; 113:263–266.

29. Tang H, Fang Z, Sun Y, Li B, Shi Z, Chen J, et al. YKL-40 in asthmatic patients, and its correlations with exacerbation, eosinophils and immunoglobulin E. Eur Respir J. 2010; 35:757–760.

30. Adcock KG, Martin J, Loggins J, Kruger TE, Baier RJ. Elevated platelet-derived growth factor-BB concentrations in premature neonates who develop chronic lung disease. BMC Pediatr. 2004; 4:10.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download