Abstract
Purpose
Asthma is one of the most common allergic diseases in which depression is an important comorbidity. However, little is known about the prevalence of depression in Korean adult asthmatics. This study was performed to evaluate the association between asthma and depression and to investigate the clinical characteristics of Korean adult asthmatics with depression.
Methods
Data were acquired from 18,066 men and women, aged older than 19 years who participated in the Fifth Korea National Health and Nutrition Examination Surveys, which was conducted from 2010 to 2012. The presence of asthma was based on self-reported physician diagnosis of asthma in the Health Interview Surveys.
Results
The prevalence of asthma was 3.2%, and that of depression was 4.2%. In univariate analysis, adults with asthma were old age, marital status, unemployment, low education, low monthly family income, low number of household members, obesity (P<0.05) were significantly associated with asthma, but sex, residence area, and smoking status were not associated with asthma. The prevalence of hypertension and depression were higher in asthmatics (P<0.05), while diabetes mellitus was not associated with asthma. After adjustment for age, marital status, number of household members, monthly family income, body mass index, hypertension, unemployment, low educated status, and depression were associated with the higher prevalence of asthma (P<0.01). Depression was associated with female sex, unemployment, while it was not associated with lung function in asthmatics.
Figures and Tables
Table 1
Demographic characteristics of subjects (n= 18,066)

Table 2
Demographic characteristics according to the presence of asthma(n= 18,066)

Table 3
Adjusted odds ratio (OR) and their 95% confidence intervals (CIs) for the prevalence of asthma

Table 4
Demographic characteristics of asthma with and without depression (n= 587)

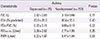
Table 5
Lung function of asthma with and without depression (n=587)
References
1. Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006; 368:733–743.

3. Kim H, Oh SY, Kang MH, Kim KN, Kim Y, Chang N. Association between kimchi intake and asthma in Korean adults: the fourth and fifth Korea National Health and Nutrition Examination Survey (2007-2011). J Med Food. 2014; 17:172–178.

4. Kim SY, Jung JY, Park MS, Kang YA, Kim EY, Kim SK, et al. Increased prevalence of self-reported asthma among Korean adults: an analysis of KNHANES I and IV data. Lung. 2013; 191:281–288.

5. Brown EM, Arrieta MC, Finlay BB. A fresh look at the hygiene hypothesis: how intestinal microbial exposure drives immune effector responses in atopic disease. Semin Immunol. 2013; 25:378–387.

6. Delfino RJ. Epidemiologic evidence for asthma and exposure to air toxics: linkages between occupational, indoor, and community air pollution research. Environ Health Perspect. 2002; 110:Suppl 4. 573–589.

7. Pearce N, Douwes J. Lifestyle changes and childhood asthma. Indian J Pediatr. 2013; 80:Suppl 1. S95–S99.

8. Goodwin RD, Jacobi F, Thefeld W. Mental disorders and asthma in the community. Arch Gen Psychiatry. 2003; 60:1125–1130.

9. Lu Y, Mak KK, van Bever HP, Ng TP, Mak A, Ho RC. Prevalence of anxiety and depressive symptoms in adolescents with asthma: a meta-analysis and meta-regression. Pediatr Allergy Immunol. 2012; 23:707–715.

10. Cluley S, Cochrane GM. Psychological disorder in asthma is associated with poor control and poor adherence to inhaled steroids. Respir Med. 2001; 95:37–39.

11. Choi GS, Shin YS, Kim JH, Choi SY, Lee SK, Nam YH, et al. Prevalence and risk factors for depression in Korean adult patients with asthma: is there a difference between elderly and non-elderly patients? J Korean Med Sci. 2014; 29:1626–1631.

12. Kunik ME, Roundy K, Veazey C, Souchek J, Richardson P, Wray NP, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005; 127:1205–1211.

13. Loerbroks A, Apfelbacher CJ, Bosch JA, Sturmer T. Depressive symptoms, social support, and risk of adult asthma in a population-based cohort study. Psychosom Med. 2010; 72:309–315.

14. Oraka E, King ME, Callahan DB. Asthma and serious psychological distress: prevalence and risk factors among US adults, 2001-2007. Chest. 2010; 137:609–616.
15. Hasler G, Gergen PJ, Kleinbaum DG, Ajdacic V, Gamma A, Eich D, et al. Asthma and panic in young adults: a 20-year prospective community study. Am J Respir Crit Care Med. 2005; 171:1224–1230.
16. Scott KM, Von Korff M, Ormel J, Zhang MY, Bruffaerts R, Alonso J, et al. Mental disorders among adults with asthma: results from the World Mental Health Survey. Gen Hosp Psychiatry. 2007; 29:123–133.

17. Song WJ, Kang MG, Chang YS, Cho SH. Epidemiology of adult asthma in Asia: toward a better understanding. Asia Pac Allergy. 2014; 4:75–85.

18. Kim KW, Kim SH, Shin JH, Choi BY, Nam JH, Park SC. Psychosocial, physical, and autonomic correlates of depression in Korean adults: results from a county-based depression screening study. Psychiatry Investig. 2014; 11:402–411.

19. Kim TS, Jeong SH, Kim JB, Lee MS, Kim JM, Yim HW, et al. The clinical research center for depression study: baseline characteristics of a Korean long-term hospital-based observational collaborative prospective cohort study. Psychiatry Investig. 2011; 8:1–8.

20. Park RJ, Moon JD. Coffee and depression in Korea: the fifth Korean National Health and Nutrition Examination Survey. Eur J Clin Nutr. 2015; 69:501–504.

21. Brumpton BM, Leivseth L, Romundstad PR, Langhammer A, Chen Y, Camargo CA Jr, et al. The joint association of anxiety, depression and obesity with incident asthma in adults: the HUNT study. Int J Epidemiol. 2013; 42:1455–1463.

22. Sengupta P, Benjamin AI. Prevalence of depression and associated risk factors among the elderly in urban and rural field practice areas of a tertiary care institution in Ludhiana. Indian J Public Health. 2015; 59:3–8.

23. Weyerer S, Eifflaender-Gorfer S, Kohler L, Jessen F, Maier W, Fuchs A, et al. Prevalence and risk factors for depression in non-demented primary care attenders aged 75 years and older. J Affect Disord. 2008; 111:153–163.

24. Ministry of Health & Welfare; Korea Centers for Disease Control and Prevention. Korea Health Statistics 2012: Korea National Health and Nutrition Examination Survey (KNHANES V-3). Cheongwon: Ministry of Health & Welfare, Korea Centers for Disease Control and Prevention;2013.
25. Di Marco F, Santus P, Centanni S. Anxiety and depression in asthma. Curr Opin Pulm Med. 2011; 17:39–44.

26. Ng TP, Chiam PC, Kua EH. Mental disorders and asthma in the elderly: a population-based study. Int J Geriatr Psychiatry. 2007; 22:668–674.

27. Wong SY, Woo J, Lynn HS, Leung J, Tang YN, Leung PC. Risk of depression in patients with chronic respiratory diseases: results from two large cohort studies in Chinese elderly from Hong Kong. Int J Geriatr Psychiatry. 2006; 21:233–238.

28. Kapadia SG, Wei C, Bartlett SJ, Lang J, Wise RA, Dixon AE, et al. Obesity and symptoms of depression contribute independently to the poor asthma control of obesity. Respir Med. 2014; 108:1100–1107.

29. Krommydas GC, Gourgoulianis KI, Angelopoulos NV, Kotrotsiou E, Raftopoulos V, Molyvdas PA. Depression and pulmonary function in outpatients with asthma. Respir Med. 2004; 98:220–224.

30. Ritz T, Steptoe A. Emotion and pulmonary function in asthma: reactivity in the field and relationship with laboratory induction of emotion. Psychosom Med. 2000; 62:808–815.

31. Rimington LD, Davies DH, Lowe D, Pearson MG. Relationship between anxiety, depression, and morbidity in adult asthma patients. Thorax. 2001; 56:266–271.

32. Centanni S, Di Marco F, Castagna F, Boveri B, Casanova F, Piazzini A. Psychological issues in the treatment of asthmatic patients. Respir Med. 2000; 94:742–749.

33. Zaubler TS, Katon W. Panic disorder and medical comorbidity: a review of the medical and psychiatric literature. Bull Menninger Clin. 1996; 60:2 Suppl A. A12–A38.
35. Cookson H, Granell R, Joinson C, Ben-Shlomo Y, Henderson AJ. Mothers' anxiety during pregnancy is associated with asthma in their children. J Allergy Clin Immunol. 2009; 123:847–853. e11.

36. Dreger LC, Kozyrskyj AL, HayGlass KT, Becker AB, MacNeil BJ. Lower cortisol levels in children with asthma exposed to recurrent maternal distress from birth. J Allergy Clin Immunol. 2010; 125:116–122.

37. Wright RJ, Rodriguez M, Cohen S. Review of psychosocial stress and asthma: an integrated biopsychosocial approach. Thorax. 1998; 53:1066–1074.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download