Abstract
Purpose
We aimed to evaluate the use and safety of double dose oseltamivir for patients manifesting severe respiratory symptoms or showing no improvement of clinical symptoms after 72 hours' treatment with the usual oseltamivir dosage.
Methods
We analyzed the clinical features of 2009 influenza A H1N1 inpatients who had been admitted to a university hospital's Department of Pediatrics between August 2009 and January 2010. The Influenza A H1N1 diagnoses were confirmed by real-time reverse transcriptase polymerase chain reaction.
Results
The study participants numbered 157 (mean age, 5.0 years; male-to-female ratio, 1.1:1). Among them, twenty (mean age, 5.2 years) were administered double dose oseltamivir. This double dose group showed higher peak body temperatures and more abnormal radiologic results than the other, usual-dose group. The mean time duration between high fever and afebrile status after initiation of double-dose oseltamivir administration was 2.1 days, whereas that within the usual-dose group was 1.7 days. There were no adverse effects in the patients treated with double-dose oseltamivir.
Figures and Tables
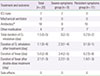
Table 2
Clinical features and radiologic and laboratory test results for Influenza A H1N1 patients receiving double-dose oseltamivir (n=20)

Values are presented as mean (range).
GI, gastrointestinal; WBC, white blood cell; CRP, C-reactive protein.
*Other symptoms included arthralgia, skin lesion, and headache. The first patient complained of arthralgia and urticaria on the day of admittance; the second patient complained of macular rash, abdominal pain and the uttering of meaningless words, immediately upon taking the first double-dose of oseltamivir; the third patient complained of headache.
References
1. Halasa NB. Update on the 2009 pandemic influenza A H1N1 in children. Curr Opin Pediatr. 2010; 22:83–87.

2. Neuzil KM, Zhu Y, Griffin MR, Edwards KM, Thompson JM, Tollefson SJ, et al. Burden of interpandemic influenza in children younger than 5 years: a 25-year prospective study. J Infect Dis. 2002; 185:147–152.

3. World Health Organization. Clinical management of human infection with pandemic (H1N1) 2009: revised guidance. 2009 Nov [Internet]. Geneva: World Health Organization;c2013. cited 2012 Nov 16. Available from: http://www.who.int/csr/resources/publications/swineflu/clinical_management_h1n1.pdf.
4. Hui DS, Lee N, Chan PK. Clinical management of pandemic 2009 influenza A(H1N1) infection. Chest. 2010; 137:916–925.

5. World Health Organization. Clinical management of adult patients with complications of pandemic influenza A(H1N1) 2009 influenza: emergency guidelines for the management of patients with severe respiratory distress and shock in district hospitals in limited-resource settings. 2010 May [Internet]. Geneva: World Health Organization;c2013. cited 2012 Nov 16. Available from: http://www.who.int/csr/resources/publications/swineflu/imai_h1n1.pdf.
6. WHO guidelines for pharmacological management of pandemic influenza A(H1N1) 2009 and other influenza viruses [Internet]. Geneva: World Health Organization;2010. 02. cited 2013 Jul 4. Available from: http://www.ncbi.nlm.nih.gov/books/NBK138515/.
7. To KK, Hung IF, Li IW, Lee KL, Koo CK, Yan WW, et al. Delayed clearance of viral load and marked cytokine activation in severe cases of pandemic H1N1 2009 influenza virus infection. Clin Infect Dis. 2010; 50:850–859.

8. Bai L, Gu L, Cao B, Zhai XL, Lu M, Lu Y, et al. Clinical features of pneumonia caused by 2009 influenza A(H1N1) virus in Beijing, China. Chest. 2011; 139:1156–1164.

9. Okada T, Morozumi M, Matsubara K, Komiyama O, Ubukata K, Takahashi T, et al. Characteristic findings of pediatric inpatients with pandemic (H1N1) 2009 virus infection among severe and nonsevere illnesses. J Infect Chemother. 2011; 17:238–245.

10. Hackett S, Hill L, Patel J, Ratnaraja N, Ifeyinwa A, Farooqi M, et al. Clinical characteristics of paediatric H1N1 admissions in Birmingham, UK. Lancet. 2009; 374:605.

12. Binz P, Bodmer N, Leibundgut K, Teuffel O, Niggli FK, Ammann RA. Different fever definitions and the rate of fever and neutropenia diagnosed in children with cancer: a retrospective two-center cohort study. Pediatr Blood Cancer. 2013; 60:799–805.

13. Global initiative for asthma. Pocket guide for asthma management and prevention in children 5 years and younger. 2009 May [Internet]. [place unknown]: The Global Initiative For Asthma;cited 2013 Sep 15. Available from: http://www.Ginasthma.Org/local/uploads/files/GINA_Under5_Pocket_20091_1.pdf.
14. Global initiative for asthma. Pocket guide for asthma management and prevention. 2012 December [Internet]. [place unknown]: The Global Initiative For Asthma;cited 2013 Sep 15. Available from: http://www.Ginasthma.org/local/uploads/files/GINA_Pocket2013_May15.pdf.
15. Widmer N, Meylan P, Ivanyuk A, Aouri M, Decosterd LA, Buclin T. Oseltamivir in seasonal, avian H5N1 and pandemic 2009 A/H1N1 influenza: pharmacokinetic and pharmacodynamic characteristics. Clin Pharmacokinet. 2010; 49:741–765.
17. Dutkowski R, Smith JR, Davies BE. Safety and pharmacokinetics of oseltamivir at standard and high dosages. Int J Antimicrob Agents. 2010; 35:461–467.

18. Nicholson KG, Aoki FY, Osterhaus AD, Trottier S, Carewicz O, Mercier CH, et al. Neuraminidase Inhibitor Flu Treatment Investigator Group. Efficacy and safety of oseltamivir in treatment of acute influenza: a randomised controlled trial. Lancet. 2000; 355:1845–1850.

19. Treanor JJ, Hayden FG, Vrooman PS, Barbarash R, Bettis R, Riff D, et al. US Oral Neuraminidase Study Group. Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza: a randomized controlled trial. JAMA. 2000; 283:1016–1024.

20. Oo C, Barrett J, Hill G, Mann J, Dorr A, Dutkowski R, et al. Pharmacokinetics and dosage recommendations for an oseltamivir oral suspension for the treatment of influenza in children. Paediatr Drugs. 2001; 3:229–236.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download