Abstract
Purpose
Endotoxin exposure is associated with the development and pathogenesis of allergic diseases. The present study aimed to determine whether plasma endotoxins are elevated in children with atopic dermatitis (AD) and whether the plasma endotoxins are associated with the AD severity.
Methods
This study included 42 children with AD and 16 controls. The AD severity was assessed and skin prick tests were performed along with serum total IgE, total eosinophil count, and ImmunoCAP analyses for common allergens. For plasma endotoxin levels, kinetic turbidimetric assay and limulus amebocyte lysate reagent were used.
Results
The endotoxin levels were significantly higher in children with AD than in controls (0.039 [interquartile range {IQR}, 0.031 to 0.046] EU/mL vs. 0.031 [IQR, 0.019 to 0.035] EU/mL, P<0.05). The endotoxin levels showed a significantly inverse correlation with the disease severity in the extrinsic AD (r=-0.414, P=0.017) but not in the intrinsic AD (r=0.222, P=0.426). No significant correlation was observed between plasma endotoxin levels, serum total eosinophil count, and serum total IgE.
Conclusion
Our results suggest that plasma endotoxin level is increased in the AD subjects than in the normal controls and affects the disease severity only in the extrinsic AD subjects. Further studies with larger sample sizes are warranted to investigate whether plasma endotoxin levels have a different effect on the AD severity depending on the presence of atopy.
Figures and Tables
 | Fig. 1This figure shows the comparison of the plasma level of endotoxins in children with atopic dermatitis and controls. P-value was calculated by the Mann-Whitney U test. *P<0.05, atopic dermatitis versus controls. |
 | Fig. 2This figure presents the correlation between the severity of atopic dermatitis and plasma endotoxin levels in children with atopic dermatitis. Spearman correlation analysis was used to calculate the correlation between plasma endotoxin levels and the SCORing Atopic Dermatitis (SCORAD) index. |
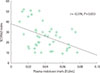
 | Fig. 3These figures demonstrate the correlations between the severity of atopic dermatitis and plasma endotoxin levels in children with extrinsic atopic dermatitis (A) and with intrinsic atopic dermatitis (B). Spearman correlation analyses were used to calculate the correlations between plasma endotoxin levels and the SCORing Atopic Dermatitis (SCORAD) index. |
Table 1
Clinical characteristics of the subjects and SCORAD index, total eosinophil count, total IgE, and plasma endotoxin levels in the three groups

Values are presented as mean±standard deviation or median (interquartile range). SCORAD, SCORing Atopic Dermatitis.
*P-value was calculated by the chi-square, Fisher exact test, Mann-Whitney U test, or Kruskal-Wallis test when appropriate. †P-value was calculated by Mann-Whitney test to compare the values between extrinsic and intrinsic atopic dermatitis subjects. ‡There was a significant difference in plasma endotoxin levels between extrinsic and intrinsic atopic dermatitis and controls by the Kruskal-Wallis test.
References
1. Hansen TE, Evjenth B, Holt J. Increasing prevalence of asthma, allergic rhinoconjunctivitis and eczema among schoolchildren: three surveys during the period 1985-2008. Acta Paediatr. 2013; 102:47–52.

2. Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006; 368:733–743.

3. Umetsu DT, Akbari O, Dekruyff RH. Regulatory T cells control the development of allergic disease and asthma. J Allergy Clin Immunol. 2003; 112:480–487.

4. Gehring U, Bolte G, Borte M, Bischof W, Fahlbusch B, Wichmann HE, et al. Exposure to endotoxin decreases the risk of atopic eczema in infancy: a cohort study. J Allergy Clin Immunol. 2001; 108:847–854.

5. Braun-Fahrländer C, Riedler J, Herz U, Eder W, Waser M, Grize L, et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N Engl J Med. 2002; 347:869–877.

6. Phipatanakul W, Celedon JC, Raby BA, Litonjua AA, Milton DK, Sredl D, et al. Endotoxin exposure and eczema in the first year of life. Pediatrics. 2004; 114:13–18.

7. Douwes J, van Strien R, Doekes G, Smit J, Kerkhof M, Gerritsen J, et al. Does early indoor microbial exposure reduce the risk of asthma? The Prevention and Incidence of Asthma and Mite Allergy birth cohort study. J Allergy Clin Immunol. 2006; 117:1067–1073.

8. Chen CM, Sausenthaler S, Bischof W, Herbarth O, Borte M, Behrendt H, et al. Perinatal exposure to endotoxin and the development of eczema during the first 6 years of life. Clin Exp Dermatol. 2010; 35:238–244.

9. Brown WG, Halonen MJ, Kaltenborn WT, Barbee RA. The relationship of respiratory allergy, skin test reactivity, and serum IgE in a community population sample. J Allergy Clin Immunol. 1979; 63:328–335.

10. Kunz B, Oranje AP, Labreze L, Stalder JF, Ring J, Taieb A. Clinical validation and guidelines for the SCORAD index: consensus report of the European Task Force on Atopic Dermatitis. Dermatology. 1997; 195:10–19.

11. Lawson JA, Dosman JA, Rennie DC, Beach JR, Newman SC, Crowe T, et al. Endotoxin as a determinant of asthma and wheeze among rural dwelling children and adolescents: a case-control study. BMC Pulm Med. 2012; 12:56.

12. Flohr C, Yeo L. Atopic dermatitis and the hygiene hypothesis revisited. Curr Probl Dermatol. 2011; 41:1–34.

13. Bolte G, Bischof W, Borte M, Lehmann I, Wichmann HE, Heinrich J, et al. Early endotoxin exposure and atopy development in infants: results of a birth cohort study. Clin Exp Allergy. 2003; 33:770–776.

14. Rizzo MC, Naspitz CK, Fernandez-Caldas E, Lockey RF, Mimica I, Sole D. Endotoxin exposure and symptoms in asthmatic children. Pediatr Allergy Immunol. 1997; 8:121–126.

16. Reefer AJ, Satinover SM, Wilson BB, Woodfolk JA. The relevance of microbial allergens to the IgE antibody repertoire in atopic and nonatopic eczema. J Allergy Clin Immunol. 2007; 120:156–163.

17. Shin JE, Jeon YH, Yang HJ, Pyun BY. Comparison of clinical severity and laboratory results between atopic and non-atopic eczema in children. Pediatr Allergy Respir Dis. 2008; 18:219–227.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download