This article has been corrected. See "ERRATUM: Spelling Correction. Suppressive effects of long-term treatment with inhaled steroids on hypothalamic-pituitary-adrenal axis in asthma" in Volume 2 on page 398.
This article has been corrected. See "ERRATUM: Table Correction. Suppressive effects of long-term treatment with inhaled steroids on hypothalamic-pituitary-adrenal axis in asthma" in Volume 3 on page 90.
Abstract
Purpose
Long-term treatment with inhaled steroids (ICS), especially fluticasone that developed lately, may suppress the hypothalamic-pituitary-adrenal (HPA) axis. This study investigated the relationship between ICS use and HPA axis suppression in asthmatics under ICS treatment for average 4.5 years.
Methods
The medical records of 129 adult asthmatics who received ICS treatment for 6 months or more and underwent a corticotropin stimulation test from January 2005 to August 2013 were retrospectively reviewed.
Results
The patients received ICS only (n=87) were found to have an abnormal response to the corticotropin test in as high as 32.2%, and those received ICS in combination with oral steroids (n=42) had a significantly higher prevalence of the response (71.4%, P<0.001). Abnormal responses to corticotropin occurred depending on ICS daily doses (low, n=8, 12.5%; medium, n=19, 36.8%; high, n=102, 49.0%; χ2=4.384, P=0.036). Among the subjects received ICS only, nasal steroid doses (P=0.016) but not ICS doses (P=0.159) were significantly higher in those with abnormal responses than the others. Among all the subjects, oral steroid use (odds ratio [OR], 4.27; 95% confidence interval [CI], 2.35-11.80; P<0.001) and nasal steroid dose (OR, 1.02; 95% CI, 1.00-1.04; P=0.015) were significant risk factors for HPA axis suppression.
Conclusion
One-third of asthmatics under long-term treatment with ICS showed a suppression of the HPA axis in a dose-dependent manner. Oral or nasal steroid use may be a risk factor for the suppression. However, since our results may have been overestimated due to subject selection bias, further prospective case-control studies are warranted.
Figures and Tables
Fig. 1
Comparison of adrenal suppression markers (morning cortisol ≤3 µg/dL [A], serum cortisol <18 µg/dL before and 60 minutes after administration of 250-µg ACTH [B], and adrenal insufficiency determined by abnormal ACTH test response or morning cortisol ≤3 µg/dL [C]) between asthma patients used inhaled steroid (ICS) only and those used inhaled +oral steroids (OCS). ACTH, adrenocorticotrophic hormone.

Fig. 2
Comparison of adrenal suppression markers (morning cortisol ≤3µg/dL [A], serum cortisol <18 µg/dL before and 60 minutes after administration of 250-µg ACTH [B], and adrenal insufficiency determined by abnormal ACTH test response or morning cortisol ≤3 µg/dL [C]) among asthma patient groups classified according to the daily doses of inhaled steroids. ACTH, adrenocorticotrophic hormone.

Fig. 3
Correlation between serum cortisol levels at 60 minutes after administration of 250-µg adrenocorticotrophic hormone (ACTH) and oral (A), nasal (B), or inhaled steroid doses (C).

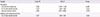
Table 1
The demographics and clinical characteristics of asthma patients treated with inhaled corticosteroid and classified according to the daily doses of inhaled steroids
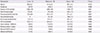
Values are presented as mean±standard deviation or number (%).
ICS, inhaled corticosteroid; FEV1, forced expiratory volume in one second; ACTH, adrenocorticotrophic hormone.
*Abnormal ACTH response: serum cortisol <18 µg/dL before and 60 minutes after administration of 250-µg adrenocorticotrophic hormone. †Adrenal insufficiency: abnormal ACTH response or morning cortisol ≤3 µg/dL.
References
1. The Global Initiative for Asthma. Global strategy for asthma management and prevention 2012 (update) [Internet]. cited 2014 Jan 22. Available from: http://www.ginasthma.org/documents/4.
2. Waalkens HJ, Van Essen-Zandvliet EE, Hughes MD, Gerritsen J, Duiverman EJ, Knol K, et al. The Dutch CNSLD Study Group. Cessation of long-term treatment with inhaled corticosteroid (budesonide) in children with asthma results in deterioration. Am Rev Respir Dis. 1993; 148:1252–1257.

3. National Heart, Lung, and Blood Institute. National asthma education and prevention program. Expert panel report 3: Guidelines for the diagnosis and management of asthma full report 2007. NIH Publication No. 07-4051, 2007. Bethesda, MD: National Institute of Health;2007.
4. Pauwels RA, Yernault JC, Demedts MG, Geusens P. Safety and efficacy of fluticasone and beclomethasone in moderate to severe asthma Belgian Multicenter Study Group. Am J Respir Crit Care Med. 1998; 157(3 Pt 1):827–832.

5. Han ER, Choi IS, Kim HK, Kang YW, Park JG, Lim JR, et al. Inhaled corticosteroid-related tooth problems in asthmatics. J Asthma. 2009; 46:160–164.

6. Wolthers OD, Honour JW. Measures of hypothalamic-pituitary-adrenal function in patients with asthma treated with inhaled glucocorticoids: clinical and research implications. J Asthma. 1999; 36:477–486.

7. Ahmet A, Kim H, Spier S. Adrenal suppression: a practical guide to the screening and management of this under-recognized complication of inhaled corticosteroid therapy. Allergy Asthma Clin Immunol. 2011; 7:13.

8. Lipworth BJ. Systemic adverse effects of inhaled corticosteroid therapy: a systematic review and meta-analysis. Arch Intern Med. 1999; 159:941–955.

9. Schwartz RH, Neacsu O, Ascher DP, Alpan O. Moderate dose inhaled corticosteroid-induced symptomatic adrenal suppression: case report and review of the literature. Clin Pediatr (Phila). 2012; 51:1184–1190.

10. Todd GR, Acerini CL, Ross-Russell R, Zahra S, Warner JT, McCance D. Survey of adrenal crisis associated with inhaled corticosteroids in the United Kingdom. Arch Dis Child. 2002; 87:457–461.

11. Lipworth BJ, Kaliner MA, LaForce CF, Baker JW, Kaiser HB, Amin D, et al. Effect of ciclesonide and fluticasone on hypothalamic-pituitary-adrenal axis function in adults with mild-to-moderate persistent asthma. Ann Allergy Asthma Immunol. 2005; 94:465–472.

12. Heller MK, Laks J, Kovesi TA, Ahmet A. Reversal of adrenal suppression with ciclesonide. J Asthma. 2010; 47:337–339.

13. Lee YC, Rhee YK. Effect of inhaled steroids on the cortisol concentration by different dosage or delivery method. Tuberc Respir Dis. 1995; 42:888–899.

15. Neary N, Nieman L. Adrenal insufficiency: etiology, diagnosis and treatment. Curr Opin Endocrinol Diabetes Obes. 2010; 17:217–223.

16. Dickstein G, Saiegh L. Low-dose and high-dose adrenocorticotropin testing: indications and shortcomings. Curr Opin Endocrinol Diabetes Obes. 2008; 15:244–249.

17. Zollner EW, Lombard CJ, Galal U, Hough FS, Irusen EM, Weinberg E. Hypothalamic-pituitary-adrenal axis suppression in asthmatic school children. Pediatrics. 2012; 130:e1512–e1519.
18. Crapo RO, Morris AH, Gardner RM. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981; 123:659–664.
19. Masoli M, Weatherall M, Holt S, Shirtcliffe P, Beasley R. Inhaled fluticasone propionate and adrenal effects in adult asthma: systematic review and meta-analysis. Eur Respir J. 2006; 28:960–967.

20. Wlodarczyk JH, Gibson PG, Caeser M. Impact of inhaled corticosteroids on cortisol suppression in adults with asthma: a quantitative review. Ann Allergy Asthma Immunol. 2008; 100:23–30.

21. Guilbert TW, Denlinger LC. Role of infection in the development and exacerbation of asthma. Expert Rev Respir Med. 2010; 4:71–83.

22. Webster JI, Sternberg EM. Role of the hypothalamic-pituitary-adrenal axis, glucocorticoids and glucocorticoid receptors in toxic sequelae of exposure to bacterial and viral products. J Endocrinol. 2004; 181:207–221.

23. Sim D, Griffiths A, Armstrong D, Clarke C, Rodda C, Freezer N. Adrenal suppression from high-dose inhaled fluticasone propionate in children with asthma. Eur Respir J. 2003; 21:633–636.

24. Bousquet J, Van Cauwenberge P, Khaltaev N. Aria Workshop Group. World Health Organization. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001; 108:5 Suppl. S147–S334.

25. Adams RJ, Fuhlbrigge AL, Finkelstein JA, Weiss ST. Intranasal steroids and the risk of emergency department visits for asthma. J Allergy Clin Immunol. 2002; 109:636–642.

26. The Korean Society of Allergology. National guideline for the diagnosis and management of allergic rhinitis. J Asthma Allergy Clin Immunol. 1999; 19:809–885.
27. Zollner EW. Hypothalamic-pituitary-adrenal axis suppression in asthmatic children on inhaled corticosteroids: part 1. Which test should be used? Pediatr Allergy Immunol. 2007; 18:401–409.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download