Abstract
Purpose
Necrotizing pneumonia (NP) is a complication of invasive pneumonia. Few studies have reported on the clinical features of NP in children.
Methods
Nineteen patients with NP who were admitted to Pusan National University Hospital and Pusan National University Children's Hospital between December 2008 and March 2013, were studied in terms of sex, age at diagnosis, clinical characteristics, detected organisms, radiologic findings, treatments and clinical outcomes.
Results
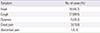
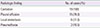
Twelve patients (63.2%) were males and seven patients (36.8%) were female. Eight patients (44.4%) were younger than 5 years of age, seven patients (38.9%) were at 6-10 years of age and four patients (21.1%) were older than 11 years of age. Most patients had fever and cough at the time of diagnosis. Minorganism were identified in 9 cases (47.4%): Mycoplasma pneumonia in 4 (21.1%), Streptococcus pneumonia in 1 (5.3%), Staphylococcus aureus in 1 (5.3%), G+cocci in 1 (5.3%), and M. pneumonia + S. pneumoniae coinfection in 2 (10.5%). The diagnosis of NP was established by computerized tomography. Cavitary necrosis was shown in all patients, and pleural effusion was shown in 15 patients (78.9%). Six patients (31.6%) presented local atelectasis and 2 patients (10.5%) presented pneumothorax. Five patients (26.3%) treated with only antibiotics were cured completely. Invasive treatment was needed by 14 patients (73.7%): 10 patients (52.6%) needed chest tubing, and 5 patients (26.3%) needed surgery. Only one patient (5.3%) expired.
Conclusion
NP is a rare complication of pneumonia in children and has a good prognosis, typically resolving completely with medical treatment alone. However, patients who present with the worsening of clinical status or pleural complications despite the use of appropriate antibiotics should be evaluated for surgical indications.
Figures and Tables
 | Fig. 1A 16-year-old male with diagnosed with combined infection of Mycoplasma pneumoniae and Streptococcus pneumoniae (patient #17 in Table 1). He was underwent right lobectomy previously. Plain radiograph and chest computed tomography (CT) (A, B) which obtained at the time of admission show consolidation in the remained right middle lobe and right lower lobe. Large areas of low attenuation may represent necrotizing pneumonia. After 10 days, plain radiograph (C) reveal total haziness in the right hemithorax and air-fluid level in the right upper lung field (black arrow). On CT scan (D), a cavitary lesion was appeared in the right hemithorax. Note the air-fluid level within the cavitary lesion which may suggest lung abscess. Plain radiograph and CT scan which acquired after 13 days of admission (E, F) show interval decrease of abscess cavity (white arrowheads) in its extent after percutaneous placement of thoracostomy catheter (white arrow) for drainage of lung abscess. In spite of conservative treatment, however, the patient was underwent right pneumonectomy (G). |
Table 1
Patient characteristics (n=19)

Bo, bronchiolitis obliterans; LLL, left lower lobe; LUL, left upper lobe; RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; VATS, video assisted thoracoscopic surgery; CGD, chronic granluomatous disease; PCD, percutaneous catheter drainage; HLH, hemophagocytic lymphohistiocytosis; S. pneumoniae, Streptococcus pneumoniae; M. pneumoniae, Mycoplasma pneumoniae; S. aureus, Staphylococcus aureus.
*Gram-positive cocci didn't identified.
References
1. Hacimustafaoglu M, Celebi S, Sarimehmet H, Gurpinar A, Ercan I. Necrotizing pneumonia in children. Acta Paediatr. 2004; 93:1172–1177.

2. Im JG, Han MC, Yeon KM, Ryoo JW, Park HS. Necrotizing pneumonia: CT findings & its clinical significance. J Korean Radiol Soc. 1995; 33:875–881.

3. Lee KY, Yim SJ, Yoon JS, Han JW, Lee JS. Two cases of community acquired necrotizing pneumonia in healthy children. Pediatr Allergy Respir Dis. 2006; 16:71–78.
4. McCarthy VP, Patamasucon P, Gaines T, Lucas MA. Necrotizing pneumococcal pneumonia in childhood. Pediatr Pulmonol. 1999; 28:217–221.

5. Wang RS, Wang SY, Hsieh KS, Chiou YH, Huang IF, Cheng MF, et al. Necrotizing pneumonitis caused by Mycoplasma pneumoniae in pediatric patients: report of five cases and review of literature. Pediatr Infect Dis J. 2004; 23:564–567.

6. Sawicki GS, Lu FL, Valim C, Cleveland RH, Colin AA. Necrotising pneumonia is an increasingly detected complication of pneumonia in children. Eur Respir J. 2008; 31:1285–1291.

7. Liu JR, Xu BP, Li HM, Sun JH, Tian BL, Zhao SY, et al. Clinical analysis of 20 cases with Streptococcus pneumoniae necrotizing pneumonia in China. Zhonghua Er Ke Za Zhi. 2012; 50:431–434.
8. Lee NY, Hur TH, Song SW, Lee HK, Lee KY, Lee HS, et al. Clinical aspects of necrotizing pneumonitis resulting from Mycoplasma pneumoniae infection in children. Pediatr Allergy Respir Dis. 2007; 17:183–195.
9. Kerem E, Bar Ziv Y, Rudenski B, Katz S, Kleid D, Branski D. Bacteremic necrotizing pneumococcal pneumonia in children. Am J Respir Crit Care Med. 1994; 149:242–244.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download