Abstract
Purpose
The study for bronchiectasis in children is rare in Korea. The aim of this study was investigate the clinical characteristic and associated etiology in pediatric patients with bronchiectasis.
Methods
We studied 29 pediatirc patients with bronchiectasis from January 2008 to December 2012 at Pusan National University Hospital. The age, sex, clinical symptoms, signs, radiologic findings, associated etiologic factors, and clinical course were investigated retrospectively.
Results
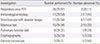
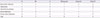
The median age at the time of diagnosis of bronchiectasis was 8.7 years. Chronic coughing was the most common symptom. The associated etiologies were immunodeficiency (31.0%), respiratory infection (27.6%), bronchiolitis obliterans (13.8%), interstitial lung disease (10.3%). The median age at the time of diagnosis of bronchiectasis in immunodeficient patients was 8.3 years. Post infectious bronchiectasis and severe respiratory symptom tend to occur in younger children.
Figures and Tables
References
1. Keistinen T, Saynajakangas O, Tuuponen T, Kivela SL. Bronchiectasis: an orphan disease with a poorly-understood prognosis. Eur Respir J. 1997; 10:2784–2787.

3. Seitz AE, Olivier KN, Steiner CA, Montes de Oca R, Holland SM, Prevots DR. Trends and burden of bronchiectasis-associated hospitalizations in the United States, 1993-2006. Chest. 2010; 138:944–949.

4. Roberts HJ, Hubbard R. Trends in bronchiectasis mortality in England and Wales. Respir Med. 2010; 104:981–985.

5. Martínez-García MÁ, Soler-Cataluña JJ, Catalán-Serra P, Román-Sánchez P, Tordera MP. Clinical efficacy and safety of budesonide-formoterol in non-cystic fibrosis bronchiectasis. Chest. 2012; 141:461–468.

6. Rencken I, Patton WL, Brasch RC. Airway obstruction in pediatric patients. From croup to BOOP. Radiol Clin North Am. 1998; 36:175–187.
7. Eastham KM, Fall AJ, Mitchell L, Spencer DA. The need to redefine non-cystic fibrosis bronchiectasis in childhood. Thorax. 2004; 59:324–327.

8. Kim HY, Kwon JW, Seo J, Song YH, Kim BJ, Yu J, et al. Bronchiectasis in children: 10-year experience at a single institution. Allergy Asthma Immunol Res. 2011; 3:39–45.

9. Morrissey BM, Harper RW. Bronchiectasis: sex and gender considerations. Clin Chest Med. 2004; 25:361–372.

11. Karakoc GB, Yilmaz M, Altintas DU, Kendirli SG. Bronchiectasis: still a problem. Pediatr Pulmonol. 2001; 32:175–178.

12. Tsao PC, Lin CY. Clinical spectrum of bronchiectasis in children. Acta Paediatr Taiwan. 2002; 43:271–275.
14. Westcott JL, Cole SR. Traction bronchiectasis in end-stage pulmonary fibrosis. Radiology. 1986; 161:665–669.

15. Cartier Y, Kavanagh PV, Johkoh T, Mason AC, Muller NL. Bronchiectasis: accuracy of high-resolution CT in the differentiation of specific diseases. AJR Am J Roentgenol. 1999; 173:47–52.

16. Bouyahia O, Essadem L, Matoussi N, Gharsallah L, Fitouri Z, Mrad Mazigh S, et al. Etiology and outcome of bronchiectasis in children: a study of 41 patients. Tunis Med. 2008; 86:996–999.
17. Haidopoulou K, Calder A, Jones A, Jaffe A, Sonnappa S. Bronchiectasis secondary to primary immunodeficiency in children: longitudinal changes in structure and function. Pediatr Pulmonol. 2009; 44:669–675.

18. Driessen G, van der Burg M. Educational paper: primary antibody deficiencies. Eur J Pediatr. 2011; 170:693–702.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download