Introduction
Carotid artery dissection (CAD) is a common cause of cerebral infarction in younger patients. Bogousslavsky and Pierre
1) reported that CAD accounted for 20.5% of cases of ischemic stroke in patients aged under 45 years. However, of all CADs, extracranial internal CAD (ICAD) comprise the majority, and common CAD (CCAD) is rare. Zach et al.
17) reported that they found only 47 cases of CCAD in 43 patients. In the 47 cases, only 11 cases were traumatic CCAD without aorta involvement. To our knowledge, only 14 case reports have described traumatic CCAD.
3111417) Here, we report a case of CCAD in a patient with severe trauma, who was admitted to our institution.
Go to :

Case Report
A 50-year-old man came to the emergency room after a pedestrian traffic accident. He was lying on the road after drinking alcohol, when the car drove over him. He had multiple laceration wounds on his face, scalp, body, and leg. His blood pressure was 60/40 mmHg and oxygen saturation was 83%. The patient's mental status was stuporous (E4VTM5). He did not show any lateralizing sign at admission. The patient demonstrated hematuria following the insertion of a Foley catheter. There were no significant lesions, such as hematoma, fracture on a brain computed tomographic (CT) image (
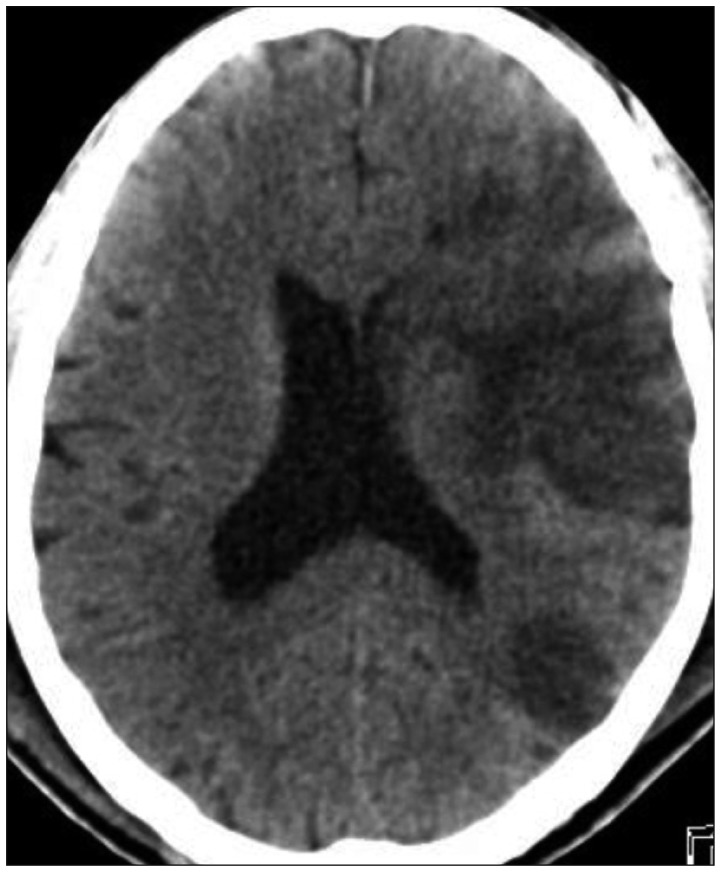
Figure 1). Further, chest CT, revealed multiple rib fractures, hemopneumothorax, and a lung contusion. He presented a flail chest. A large amount of hematoma with bladder rupture was seen on an abdomen CT scan. Moreover, a cervical CT scan revealed C6 spinous process fracture, while a pelvis CT scan showed multiple fractures in the sacral ala, iliac bone, and pubic ramus. A urological surgery team performed a bladder rupture repair operation. The patient was sedated for ventilator therapy. On hospital day 2, explore thoracotomy and open reduction of rib fracture were performed by the thoracic and cardiovascular surgery team. Hematuria ceased on hospital day 4. The patient's mental state, however, was still stuporous. Right side hemiparesis was checked and we performed a brain CT scan. It revealed large diffuse acute left middle cerebral artery (MCA) infarction, with mild mass effect (
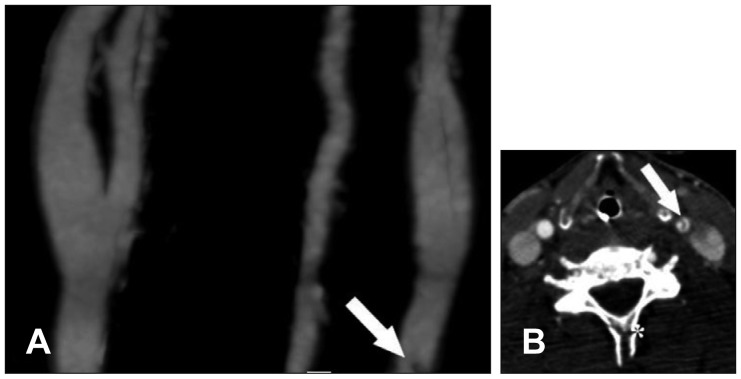
Figure 2). CT angiography showed focal carotid dissection at the left common carotid artery with intimal flap (
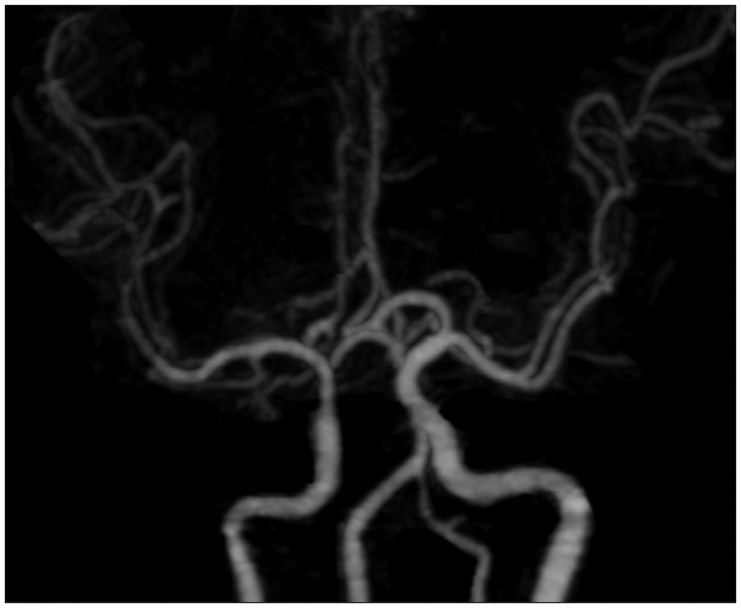
Figure 3). CCAD was located 2 cm proximally from the carotid bifurcation at the C6 level. We identified C6 spinous process fracture on the first cervical CT scan. However, the left MCA showed almost normal vascularity on CT angiography (
Figure 4). Thus, we decided to initiate intravenous clexane (enoxaparin sodium) treatment, at a dose of 40 mg. A brain CT scan showed no significant changes on hospital day 5. On hospital day 9, brain CT revealed resolution of diffuse large subacute left MCA infarction with mild mass effect. The patient was awakened to a deep drowsy mental state. Hematuria recurred on hospital day 12; clexane was discontinued. Abdominal distension was checked on hospital day 14. An abdomen CT scan revealed a huge retroperitoneal hematoma, which was suggestive of persistent bleeding. The CT scan also showed an increased amount of hematoma in the prevesical and perivesical space. This finding suggested the rupture of the urinary bladder. An angiography was performed; however, it did not reveal a significant extravasation site. The patient died on hospital day 16.
 | FIGURE 1Brain computed tomography showing no significant lesions, such as hematoma, fracture. 
|
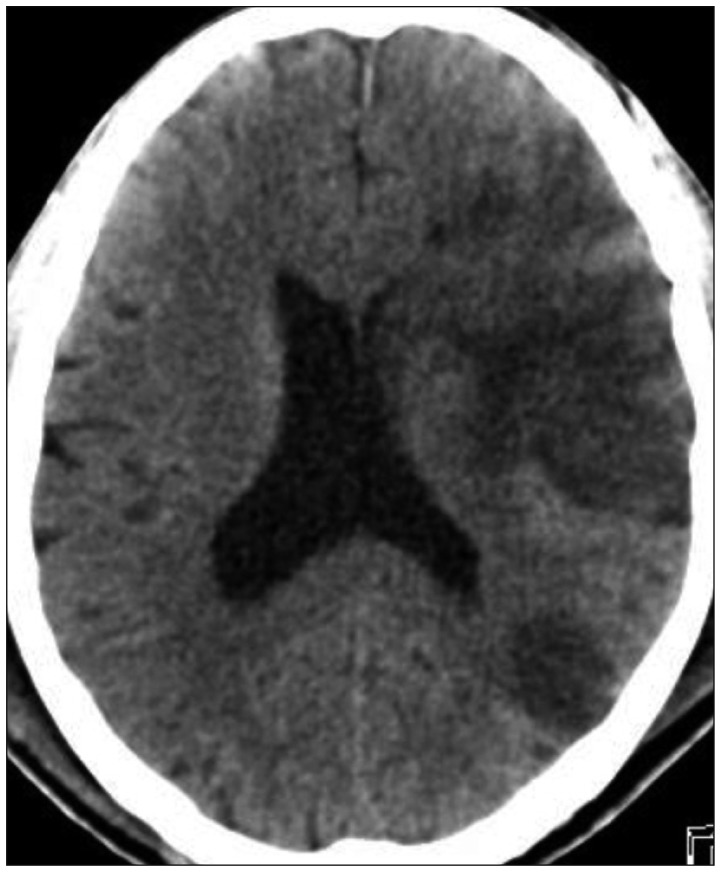 | FIGURE 2Brain computed tomography showing large diffuse acute left middle cerebral artery infarction with mild mass effect. 
|
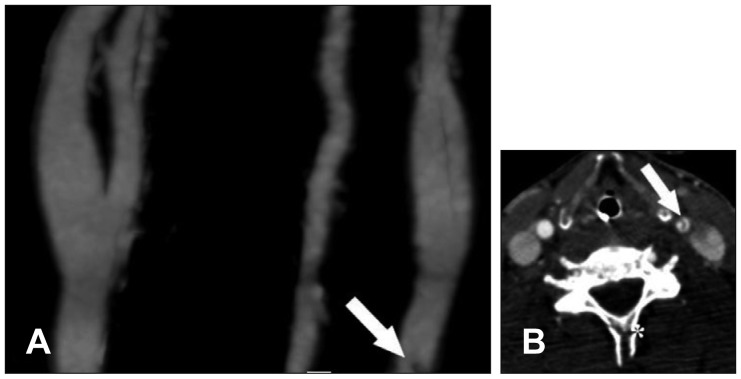 | FIGURE 3(A) Computed tomography (CT) angiography showing focal carotid dissection (white arrow) at the left common carotid artery with intimal flap. Common carotid artery dissection (CCAD) is located 2 cm proximal from the carotid bifurcation. The lesion is located at the lower part of the carotid CT angiographic image. (B) Axial image showing intimal flap of CCAD (white arrow). C6 spinous process fracture (asterisk) is also seen on the same image. 
|
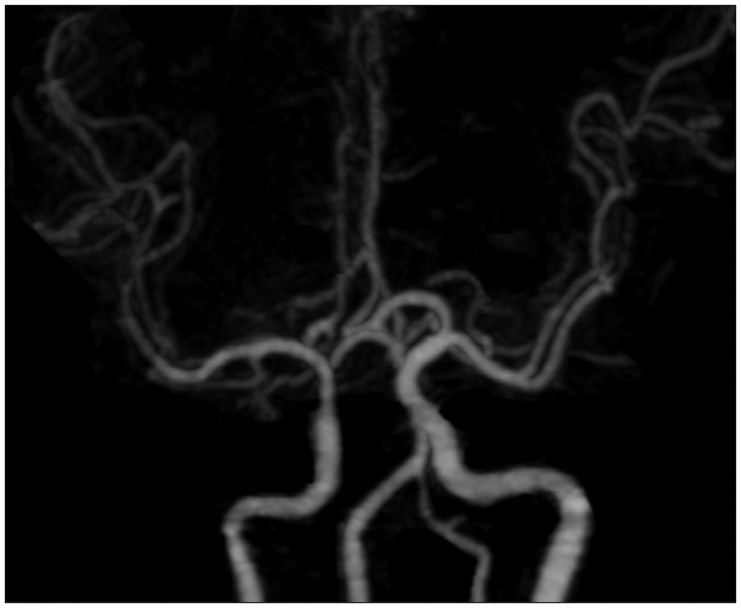 | FIGURE 4Computed tomography angiography showing almost normal vascularity of the left middle cerebral artery. 
|
Go to :

Discussion
In 1993, Schievink et al.
10) reported that the annual incidence of spontaneous ICAD was 2.6 per 100,000 population. The occurrence of CCAD, however, is very rare. Chen et al.
2) reported that although 10% of young patients with ischemic stroke had ICAD at their institution, only 0.8% of young patients with ischemic stroke had CCAD. Zach et al.
17) reported 47 cases of CCAD, which consisted of 20 cases of spontaneous CCAD, 11 cases of traumatic CCAD, 4 cases of iatrogenic CCAD, and 12 cases of CCAD associated with aortic arch dissection. Thus, traumatic CCAD is extremely rare. Therefore, the clinical aspect of traumatic CCAD is not entirely known.
In spontaneous ICAD, headache was the most common symptom.
18) While focal cerebral ischemic symptoms were the most common in traumatic ICAD.
7) In traumatic CCAD, hemiparesis was the most common symptom (50%), which our patient also showed.
17) In our case, due to the stuporous mental state and sedative effects, it was difficult to check the symptoms early. The infarcted lesions, however, already showed low density in the brain CT. In patients with multiple severe trauma, more careful attention of neurological changes are required.
The most frequent injured location in blunt carotid injuries is the internal carotid artery just distal from the bifurcation.
5816) Chen et al.
2) reported locations of spontaneous CCAD in 9 patients, of whom, 6 patients (66.7%) had dissections involving the common carotid bifurcation. CCAD in the patient reported here, however, did not involve the common carotid bifurcation, but was located 2 cm proximal from the carotid bifurcation. As seen in
Figure 2, the lesion was located at the lower part of the carotid CT angiographic image. This would not have been visible if the CT angiographic image was acquired from a little further up. Thus,in cases of possible CCAD, we recommend that examination is started from the aortic arch.
Typical angiographic findings of ICAD are irregular and often tapered stenosis with a characteristic “string sign”.
18) Zach et al.
17) found hyperechoic lesions (57.1%), intimal flaps (28.6%), a change in flow (28.6%), occlusion (28.6%), double lumen (14.3%), and mural hematomas (14.3%) in 7 cases of traumatic CCAD. Our patient did not have occlusion; the CT angiographic scan only showed the intimal flap and the MCA revealed almost normal vascularity. Steinke et al.
12) reported that 68% of ICAD cases recanalized according to follow up sonographic examinations. The interval from the onset of symptoms to recanalization of the dissection ranged from 2 days to 1 year. They suggested that some of the angiographic variations may be due to different stages of recanalization, rather than different types of dissection. Weinberger et al.
15) reported that arterial dissection can form a nidus for distal embolization. In the current case, we postulated that embolization from the common carotid artery to MCA had occurred, occluding the MCA. Overtime, the MCA might be recanalized.
There is still debate as to which treatment (anticoagulation or antiplatelet agents) is optimal for ICAD. Although there have been no randomized trials comparing them, the use of anticoagulation is generally widely advocated.
413) Lyrer and Engelter
6) reported that they did not find any differences in death, ischemic stroke between antiplatelets and anticoagulants. However, symptomatic intracranial hemorrhages(5/627; 0.8%) and major extracranial hemorrhages (7/425; 1.6%) only occurred in the anticoagulation group. In addition to severe trauma, our patient also had extracranial hemorrhages. Thus, we favored antiplatelets treatment in patients with multiple severe trauma.
The prognosis for ICAD is generally good. Schievink et al.
9) reported that the 10-year survival rate for the study population was 95.5%. Zach et al.
17) reported 7% mortality in CCAD. In traumatic CCAD, 1 case of death (10%), 8 cases of persistent neurologic deficit (80%), and 1 case of complete recovery (10%) have been reported. Including our case, the mortality associated with traumatic CCAD was 13.3%(2/15), which is almost three times that of the mortality associated with ICAD. However, since the case numbers are too small to compare mortality, this remains to be validated in the future.
Go to :

Conclusion
Here, we reported a rare case of traumatic CCAD in a patient with multiple extracranial injury. Given its rarity, the clinical aspect of traumatic CCAD is not entirely known. However, CCAD should be considered when neurologic function decreases in patients with trauma. Although CCAD is rare, this report provides useful information to trauma surgeons regarding the treatment and diagnosis of similar cases.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download