Abstract
Objective
Acute hemiparesis is often an early presentation of acute ischemic stroke, though it can occur in various disorders. This study aimed to investigate the improper use of thrombolytic agents for patients with acute hemiparesis, following the misdiagnosis of acute ischemic stroke.
Methods
We analyzed the clinical and radiological data of nine patients initially misdiagnosed with cerebral stroke in the emergency room from May 2013 to January 2017. All the patients were treated with tissue plasminogen activator (TPA) owing to the presence of acute hemiparesis. Subsequently, emergent computed tomography scan showed no intracranial hemorrhage. Clinical findings including neurological deficits, clinical course, and related complications were detected and analyzed.
Results
Acute hemiparesis was observed in the following conditions: spontaneous spinal epidural hematoma, Brown-Séquard syndrome caused by cervical disc herniation, cervical epidural abscess, hypoglycemia in the presence of an old stroke, and seizure or convulsion disorder. Although acute hemiparesis was regarded as a contraindication, inappropriate TPA administration did not aggravate the neurological condition in any of the patients who required surgery.
Go to : 
Cerebral stroke is generally suspected when patients present with acute hemiparesis but no evidence of hemorrhage on a computed tomography (CT) scan in the emergency room (ER). For intravenous (IV) thrombolytic agents to be effective in cerebral stroke, they should be administered within 3 to 4.5 hours of symptom onset.3614)
Owing to difficulties in the rapid diagnosis of cerebral stroke, thrombolytic agents such as tissue plasminogen activator (TPA) are sometimes prescribed to patients with non-stoke related acute hemiparesis in the emergency basis. Other pathologic conditions that often present with acute hemiparesis include epilepsy, spinal epidural hematoma and Brown-Séquard syndrome (BSS) caused by cervical disc herniation.27915)
Accidental administration of thrombolytic agents to a patient with acute hematoma requires surgical treatment, which may have a fatal outcome. Therefore, physicians should be aware of this possibility in diagnostic and therapeutic dilemmas.
In this report, we describe and analyze the administration of TPA following a misdiagnosis of cerebral stroke.
Go to : 
We performed a retrospective study of the medical charts and radiologic records of patients incorrectly administered with TPA for acute hemiparesis mimicking cerebral stroke. Review of the final diagnosis at discharge of all referred patients, who were considered as a cerebral stroke to the ER between May 2013 and January 2017 was conducted.
Among 138 patients, initially diagnosed with acute ischemic stroke and treated with TPA in the ER, nine patients (9/138 patients, 6.5%) were enrolled in this study. All patients met the following inclusion criteria: 1) no history of any trivial trauma injury; 2) acute hemiparesis, but no intracranial hemorrhage observed on emergent brain CT; 3) patients presented within a 3-hour window from symptom onset; 4) TPA was administered following a misdiagnosis of cerebral stroke; and 5) however, final diagnosis at discharge unrelated to transient ischemic attack (TIA) or acute ischemic stroke.
We evaluated the initial signs and symptoms observed in the patients, the true diagnosis, any adverse effects of TPA and the clinical course.
Go to : 
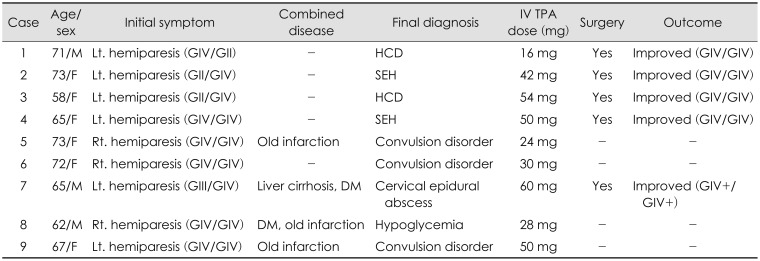
All of the patients presented with acute hemiparesis within a 3-hour window from symptom onset. Three men and 6 women, aged 58 to 73 (mean age, 67.3 years) were analyzed in this study. Further patient information including final diagnosis is summarized in Table 1. Most patients in this study, ER doctors had misused IV TPA and neurologists or NS doctor stopped IV TPA injection due to non-specific symptoms. As a result, the dosage varied according to the patients.
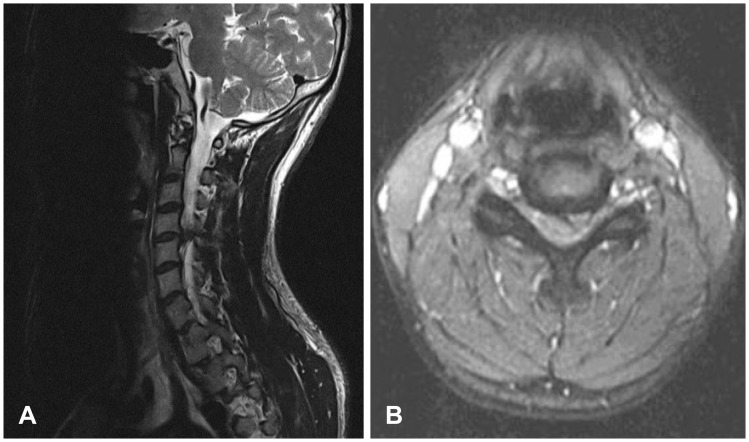
Various conditions were observed, which mimicked cerebral stroke; these included cervical disc herniation (causing BSS) in 2 cases, characterized by an ipsilateral loss of proprioceptive sensitivity with contralateral loss of pain and temperature sensitivity (Figure 1). Of these, one had no neck pain or cervical discomfort, a symptom that typically presents alongside cervical disc herniation.
Two patients were diagnosed spontaneous cervical epidural hematoma, a rare condition requiring urgent diagnosis and treatment. Neither patient's neurological condition changed following TPA administration; hence, magnetic resonance imaging (MRI) of the cervical spine was performed. This revealed a large spontaneous epidural hematoma. Both patients underwent emergent hematoma removal. Despite this, motor weakness was still apparent at the final follow-up evaluation.
One patient, who presented with a history of liver cirrhosis and diabetes mellitus (DM), was misdiagnosed with cerebral stroke and was finally diagnosed with cervical epidural abscess. Another patient had an old cerebral infarction and DM. The patient was finally diagnosed with hypoglycemia.
Seizure and convulsion disorders accounted for the rest of the cerebral stroke mimics in our study. Although all of these cases showed unilateral hemiparesis, the lack of information regarding events prior to the clinical presentation precluded the diagnosis of a condition that mimicked stroke.
Although the administered dosage varied according to the patients, TPA administration did not aggravate the neurologic status in any of the patients described in this study. Even the 5 patients who underwent surgical treatment, there had been no case showing worse than before the surgery.
Go to : 
Acute hemiparesis can develop in response to a wide variety of cerebral diseases including intracerebral hemorrhage and acute ischemic stroke.512)
Based on the patients' medical history and the presence of acute hemiparesis, brain CT is intended to rule out intracerebral hemorrhage. Absence of abnormal findings on brain CT scan would lead to suspicion of acute ischemic stroke.
IV thrombolytic agents initiated within 3 hours of symptom onset are approved for the treatment of acute ischemic stroke and are the only proven, effective treatment.10) Owing to the limited time window, prompt and accurate diagnosis is essential for the treatment of acute cerebral stroke.
However, stroke mimicking diseases may account for one fourth of suspected ischemic stroke presentations.3913) Among them, seizures and convulsion disorders account for around 20% of the stroke mimics.8)
The final diagnoses of the stroke mimics that we observed, reflected those described in several reports that evaluated patients initially diagnosed with cerebral stroke, who were not treated with thrombolytic agents. In a study including 169 patients with suspected cerebral stoke, Ferro et al.4) reported that 9% of patients were misdiagnosed. Of these, most of the true conditions were of neurological origin. Kothari et al.11) also assessed 365 patients who were admitted with suspected stroke. They found that 19 cases were of non-stroke origin. Final diagnoses included the following: paresthesia or numbness of unknown origin (3 patients), seizure (2 patients), complicated migraines (2 patients), peripheral neuropathy (2 patients), cranial nerve neuropathy (2 patients), psychogenic paralysis in (1 patient), and other conditions (7 patients).
In our report, 3 patients were finally diagnosed with seizures and convulsion disorders. Initial administration of TPA did not cause any bleeding tendency in these patients.
Hand et al.7) reported that various cervical spinal lesions can mimic acute cerebral stroke. In our series, we found 2 patients with BSS produced by a herniated cervical disc, 2 patients with spontaneous cervical spinal epidural hematoma and 1 patient with cervical epidural abscess. These presentations can be categorized as cervical spinal diseases. Among these patients, 3 did not complain of significant neck discomfort and none of the patients had a history of trauma to the head and neck. Owing to the presence of hemiparesis, these patients were treated with TPA injection following brain CT scan before cervical spine MRI and brain MRI study with diffusion-weighted imaging.
TPA administration to patients with spinal epidural hematoma can be dangerous and may result in significant neurological deficits. In our study, hemorrhagic complications or neurologic decline did not occur following TPA injection in the patients with cervical spinal epidural hematoma. However, the inappropriate use of TPA for restoring cerebral blood flow may increase the risk of intracranial hemorrhage. Previous studies have reported that patients with spontaneous cervical spinal epidural hematoma, who present with acute hemiparesis and no neck pain, can be misdiagnosed with cerebral stroke and may be mistakenly treated with antiplatelet therapy.115)
In conclusion, 6.5% of patients treated with TPA in our study had final diagnosis that did not match TIA or acute ischemic stroke.
Hemorrhagic complications or any adverse effects did not occur in any patients in our series. However, due to its small number of the mimics, safety can't be ensured with meaningful statistical analysis between group characteristics.
Go to : 
Various clinical conditions can mimic stroke symptoms, thereby ensuring that a correct diagnosis is made is essential. Some of these conditions, particularly cervical spinal disorders, require immediate treatment to reduce the risk of permanent disability. Therefore, we conclude that all physicians should ensure that careful and thorough diagnoses are made, prior to treatment with thrombolytic agents.
Go to : 
References
1. Adamson DC, Bulsara K, Bronec PR. Spontaneous cervical epidural hematoma: case report and literature review. Surg Neurol. 2004; 62:156–159. PMID: 15261513.

2. Dimou J, Jithoo R, Bush S. A patient with delayed traumatic cervical spinal epidural haematoma presenting with hemiparesis. J Clin Neurosci. 2010; 17:404–405. PMID: 20074959.

3. Fernandes PM, Whiteley WN, Hart SR, Al-Shahi Salman R. Strokes: mimics and chameleons. Pract Neurol. 2013; 13:21–28. PMID: 23315456.

4. Ferro JM, Pinto AN, Falcão I, Rodrigues G, Ferreira J, Falcão F, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke. 1998; 29:1106–1109. PMID: 9626279.
5. Förster A, Griebe M, Wolf ME, Szabo K, Hennerici MG, Kern R. How to identify stroke mimics in patients eligible for intravenous thrombolysis? J Neurol. 2012; 259:1347–1353. PMID: 22231865.

6. Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329. PMID: 18815396.

7. Hand PJ, Kwan J, Lindley RI, Dennis MS, Wardlaw JM. Distinguishing between stroke and mimic at the bedside: the brain attack study. Stroke. 2006; 37:769–775. PMID: 16484610.
8. Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ, Ford GA. Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke. 2003; 34:71–76. PMID: 12511753.

9. Hemmen TM, Meyer BC, McClean TL, Lyden PD. Identification of nonischemic stroke mimics among 411 code strokes at the University of California, San Diego, Stroke Center. J Stroke Cerebrovasc Dis. 2008; 17:23–25. PMID: 18190817.

10. Korean Stroke Society. Stroke. ed 2. Seoul: Panmuneducation;2015.
11. Kothari RU, Brott T, Broderick JP, Hamilton CA. Emergency physicians. Accuracy in the diagnosis of stroke. Stroke. 1995; 26:2238–2241. PMID: 7491643.
12. Lemmens R, Ceuppens J, Wilms G, Depreitere B. Transient hemiparesis caused by spontaneous cervical epidural hematoma. Acta Neurol Belg. 2012; 112:291–293. PMID: 22565778.

13. Libman RB, Wirkowski E, Alvir J, Rao TH. Conditions that mimic stroke in the emergency department. Implications for acute stroke trials. Arch Neurol. 1995; 52:1119–1122. PMID: 7487564.
14. Park H, Hwang GJ, Jin SC, Bang JS, Oh CW, Kwon OK. Intra-arterial thrombolysis using double devices: mechanicomechanical or chemicomechanical techniques. J Korean Neurosurg Soc. 2012; 51:75–80. PMID: 22500197.

15. Wang CC, Chang CH, Lin HJ, Lin KC, Kuo JR. Misdiagnosis of spontaneous cervical epidural haemorrhage. Eur Spine J. 2009; 18(Suppl 2):210–212. PMID: 19005691.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download