Case Report
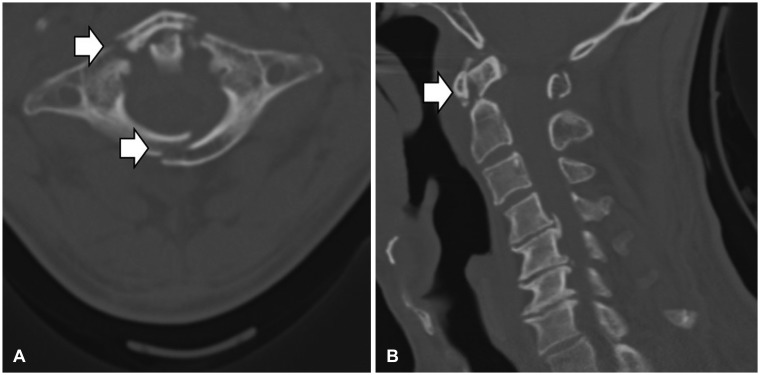
Here, we present a case of a 64-year-old man complained posterior cervical neck pain and bilateral shoulder pain after vehicle accident at April. He was ambulance driver at the time of the accident. The patient had a history of hypertension and was on medication. There was scalp laceration on vertex and no other trauma was evident. Neurological examination showed no consciousness, motor and sensory abnormality. A computed tomography (CT) scans of the cervical spine demonstrated C1 anterior, posterior arch, C2 fractures and posteriorly displaced odontoid process (
Figure 1). A magnetic resonance imaging (MRI) of the cervical spine showed no cord signal change except prevertebral soft tissue swelling and posterior soft tissue injury at C1/2 level. A fragmented odontoid process was holding back the spinal cord. There was degenerative spondylosis in the C4-5-6-7 levels. The CT angiography scan and 3-dimensional (3D) reconstruction showed occlusion of the left distal vertebral artery in the transverse foramen at the level of C2. (
Figure 2). On the following days, he underwent an arthrodesis O-C1 lateral mass-C2 pedicle - C3 pedicle fixation and on-lay graft (
Figure 3). There was a fracture in the C1 posterior arch during the operation. The C1/2/3 site was very unstable due to posterior ligament injury.
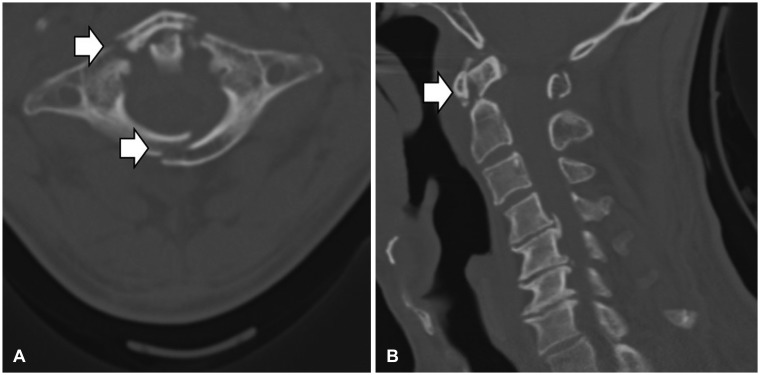 | FIGURE 1Computed tomography show fracture of C1 and C2. (A) Axial view show fracture lines (arrow) at anterior and posterior arch of atlas. (B) Sagittal reconstruction show displacement and angulation of odontoid process (arrow).
|
 | FIGURE 2Three dimension reconstruction of vertebral artery computed tomography angiography show occlusion (arrow) at the C2 transverse process level.
|
 | FIGURE 3Postoperative cervical lateral X-ray showed occipital-C1 lateral mass-C2 pedicle-C3 pedicle screw fixation and posterior on-lay bone graft.
|
The patient was discharged without any complication after surgery. Patients did not undergo preventive treatment such as aspirin for VAI. The patient complained of occipital pain for up to 3 months postoperatively, but there were no other abnormalities.
The patient re-visited with dysphasia on July 31st. The patient drank a lot of alcohol during the three days, and he said that he sweated a lot. The maximum temperature for three days was about 30℃. Neurological examination showed a clear consciousness, no motor and sensory abnormality. The patient was unable to swallow, the right pupil was 5 mm, and the left pupil was 3 mm. Uvular was deviated to the right.
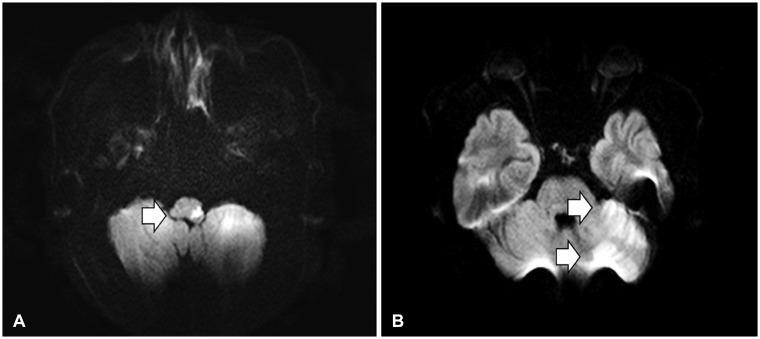
Left lateral & posterior medulla, left cerebellar hemisphere and cerebellar vermis on brain MRI with Diffusion imaging showed diffusion restriction (
Figure 4). The patient underwent conservative treatment including heparin and aspirin under the diagnosis of left lateral medullary syndrome.
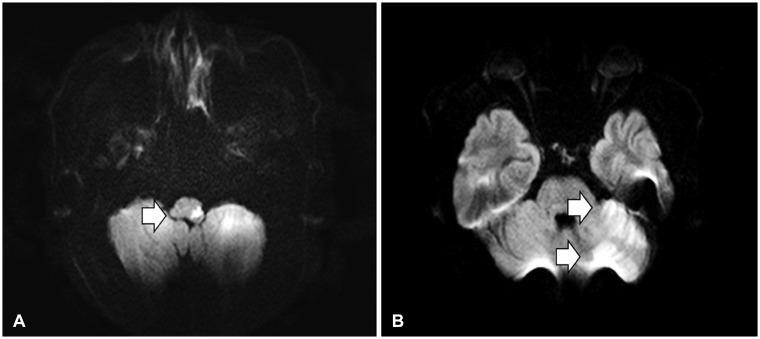 | FIGURE 4Diffusion magnetic resonance imaging show restriction (arrow) at the level of medullar (A) and cerebellar (B).
|
One month after the onset of symptoms, the patient was discharged with improved dysphagia.
The patient was followed for 40 months after the occurrence of stroke. The dysphagia has been completely restored and there is no motor and sensory abnormality besides neck pain.
Go to :

Discussion
This is a case of VA area infarction that occurred 3 months after surgical treatment of C1 and 2 fractures with VAI in a 64-year-old man. Dehydration and hypercoagulability due to hot summer weather and excessive drinking was presumed to be the causative factors. Patients did not undergo preventive treatment such as aspirin for VAI. Here, we briefly review VAI after cervical trauma and discuss prophylactic aspirin.
The incidence of VAI after trauma varies widely. It is reported that about 2% of all trauma patients, 20% of head injured patients, from 13% to 46% of blunt cervical trauma, and 7% of cervical fractures are VAI.
48) Bilateral VAI are estimated to occur at approximately 10% of the frequency of unilateral VAI.
7) Clinical considerations are needed because posterior circulatory ischemia may result.
VAI is classified as traumatic and non-traumatic depending on the cause. Traumatic injuries are classified by penetrating injury and blunt trauma, and non-traumatic VAI occur when sudden hyperextension and rotation of the neck occurs. VAI commonly accompany blunt cervical trauma. This complication has also occurred as a result of yoga exercises, calisthenics, football injuries, bow hunting. Structurally, it occurs on fixed segment and mobile segment junctions. The C6 transverse foramen is the most common and the C1/2 site is the second most common.
11) It is com-mon in children with V2 segments and adults with V3 segments.
4) In this case, the C2 transverses foramen, the border between V2 and V3, is the VAI site.
Pathologic finding in the autopsy revealed fatal dissection of the vertebral arteries.
12) In such cases, dissection
12) or occlusion of the vertebral or basilar arteries from thromboembolism caused brainstem ischemia and subsequent sudden death of the patient. To be noted that even small traumatic lesions in the vertebral arteries could cause brain infarction in the absence of occlusion of the vertebral or basilar arteries; subsequent death would occur from complications.
6)
Clinical features range from asymptomatic to fatal posterior circulation infarction. Unilateral VA occlusion is rarely ymptomatic because of collateral blood supply from the contralateral VA and the circle of Willis.
9) Moreover, injuries to the non-dominant VA are not likely to be symptomatic.
3) However, unlike unilateral VA occlusion, in which only 20% of patients are symptomatic, most patients with bilateral VA occlusion are symptomatic.
14) Bilateral or dominant VA occlusion may cause rapid and fatal ischemic damage to the cerebellum and brain stem.
Symptoms include ischemia-induced symptoms in the brain stem, cerebellum, and occipital lobe. It can cause mild headache, sensory abnormality, muscle weakness, dizziness, disappearance of co-ordination, visual defect, Horner syndrome and lateral medullary syndrome, loss of consciousness and death.
There is a controversy about aggressive screening in VAI because it is relatively small compared to the number of head trauma patients. VAI after blunt cervical trauma was previously considered to be rare. It is also argued that the early diagnosis of VAI due to aggressive screening does not significantly affect the outcome of the treatment.
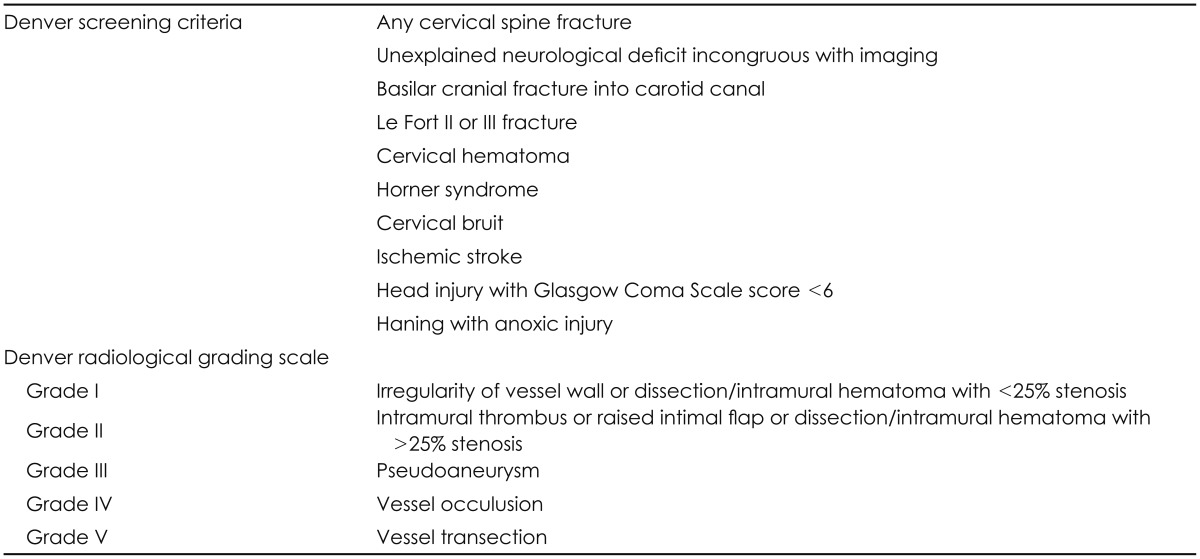
13) The recent increase in incidence is mainly due to improvements in diagnosis, particular in imaging techniques such as digital subtraction angiography (DSA), MR angiography (MRA), and CT angiography (CTA). CTA in particular is a first-choice diagnostic tool for VAI because it is non-invasive with respect to the vascular system, is easy to use, and has a high detection rate.
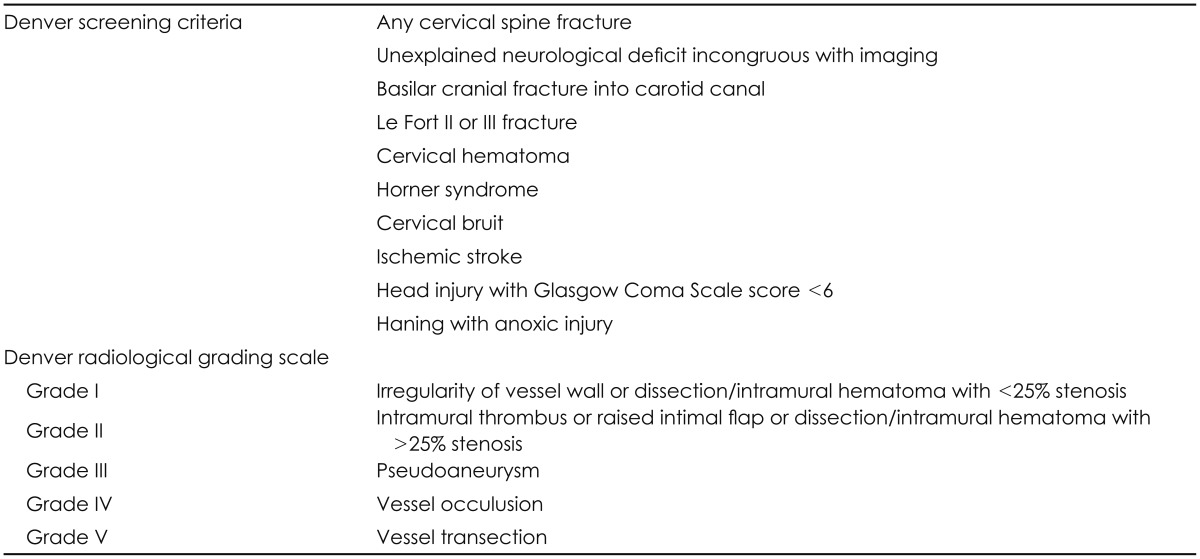
4) In this reason, CTA is a recommended for patients who are eligible for modified Denver Screening Criteria for suspected VAIs (
Table 1).
5)
TABLE 1
The Denver screening criteria for blunt cerebrovascular injury and Denver radiological grading scale of blunt cerebrovascular injury

Treatment of VAI includes anticoagulation, antiplatelet, endovascular intervention, surgical vessel sacrificing, and no treatment depending on the situation. However, there are no clear guidelines yet. According to several authors, recurrent transient ischemic attacks, stroke or death could occur within weeks unless anticoagulation or antiplatelet use.
124513) Desouza et al.
4) recommend that patients with VAI start anticoagulation and then change to antiplatelet, regardless of the presence or absence of VAI. However, Harrigan et al.
5) have recommended a multicenter, randomized, and prospective study of anticoagulation and antiplatelet efficacy for asymptomatic patients.
In this case, asymptomatic patient developed posterior circulation ischemia 4 months after VAI. The authors recommend antiplatelet because the use of antiplatelet will be more beneficial given the age of 64 and the risk factors for stroke, such as drinking, hypertension, and smoking.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download