This article has been
cited by other articles in ScienceCentral.
Abstract
A 15-year-old man presented with stupor following a motorcycle traffic accident. The patient was diagnosed with a traumatic left carotid cavernous fistula (CCF) with pseudoaneurysm of the left internal carotid artery. Brain magnetic resonance imaging (MRI) showed transiently restricted diffusion in the left centrum semiovale white matter and lower temporo-occipital area extending to the splenium of the corpus callosum, with high signal intensity on diffusion-weighted imaging. On the 35th day of admission, the patient had complete neurological recovery and a follow-up brain MRI revealed complete resolution of the lesions in the left centrum semiovale and splenium of the corpus callosum. These clinical and radiological features are highly suggestive of complete reversal of diffusion restriction after successful embolization of traumatic CCF.
Go to :

Keywords: Embolization, Carotid cavernous fistula, Diffusion restriction, Diffusion weighted imaging
Introduction
Carotid cavernous fistula (CCF) results from an abnormal communication between the carotid circulation and the cavernous sinus.
234567911) Traumatic CCF is usually type A CCF, which consist of direct high-flow shunt between the internal carotid artery (ICA) and the cavernous sinus.
234567911) Patients with traumatic direct CCF can experience exophthalmos, conjunctival injection, ophthalmoplegia and visual disturbance. Other presentations of traumatic direct CCF include fatal cerebrovascular complications such as intracerebral hemorrhage and cerebral ischemia.
23681011) Diffusion restriction can could be measured by reduced apparent diffusion coefficient (ADC) levels on magnetic resonance imaging (MRI) and is rarely reversible. However, reversible diffusion restriction has been found in patients with encephalopathy, traumatic brain injury (TBI), dural arteriovenous fistula (dAVF), hyperosmolar hyperglycemic state, cytotoxic lesions of the corpus callosum resulting from drug therapy, malignancy, infection, subarachnoid hemorrhage, metabolic disorders, trauma, and other entities.
146810) The authors report a case of traumatic direct CCF resulting in restricted diffusion that reversed following successful embolization of the direct CCF.
Go to :

Case Report
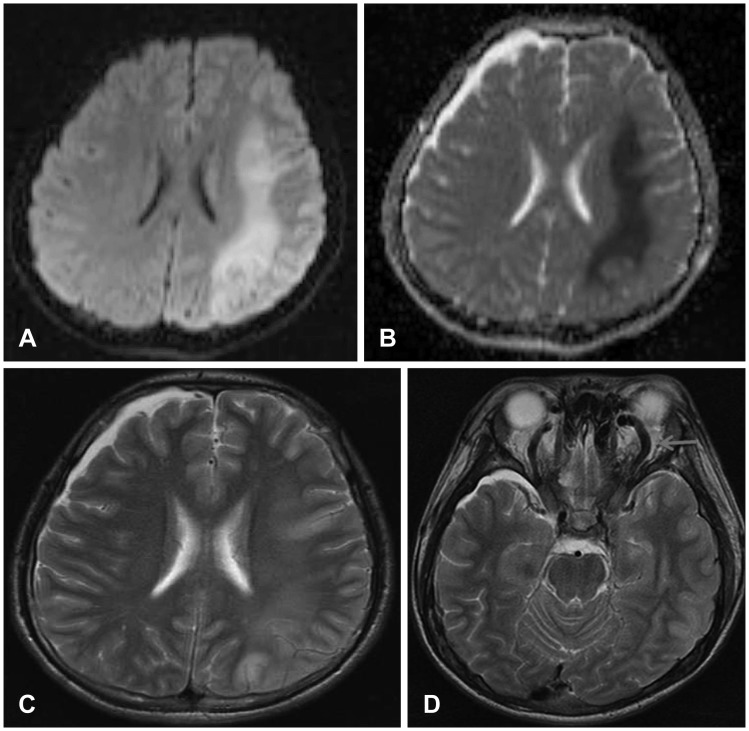
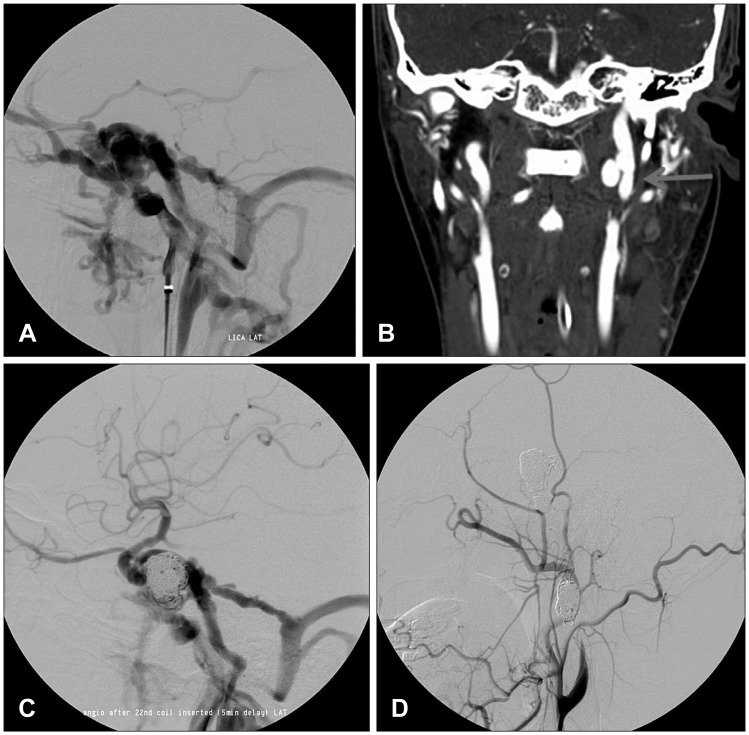
A 15-year-old man presented with stupor (Glasgow Coma Scale [GCS] 8) following a motorcycle accident. Initial computed tomography (CT) of the head and face revealed a left mandibular fracture with minimal left frontal subdural hemorrhage. Initially, the patient was diagnosed with diffuse axonal injury (DAI). On the tenth day of admission, right-sided hemiparesis developed (right arm, grade 3/5; right leg, grade 3/5), even though he was still stuporous. A brain MRI showed lesions with high signal intensity lesions on diffusion weighted imaging (DWI) (
Figure 1A) and low signal intensity on an ADC map (
Figure 1B) of the left centrum semiovale white matter and lower temporo-occipital area extending to splenium of the corpus callosum. T2-weighted axial imaging showed lesions with high signal intensity in the left centrum semiovale white matter (
Figure 1C) and a dilated tortuous superior ophthalmic vein suggestive of vascular pathology (
Figure 1D). This finding prompted intracranial CT angiography and subsequent four-vessel digital subtraction cerebral angiography which showed a left high-flow direct CCF with complete blood steal (
Figure 2A) and a pseudoaneurysm arising from the left upper cervical ICA (
Figure 2B). On the eleventh day of admission, we attempted the trans-arterial balloon-in-stent technique. Neurological examination upon immediately before surgery showed stupor. A neuroform stent (4.5/20 mm; Boston Scientific, Natick, MA, USA) was placed across the fistulous portion of the ICA and coil embolization was performed with temporary occlusion utilizing a Hyperglide balloon (Micro Therapeutics, Irvine, CA, USA) placed within the stent to prevent reflux of the embolization material into the ICA. Nine platinum coils (guglielmi detachable coil [GDC] 18–360°: 11 mm/30 cm, 9 mm/30 cm; Tornado: 5 mm/2 mm × 5; Tornado: 4 mm/2 mm × 2) were detached initially in the fistula and repeat injection showed no improvement of the arteriovenous shunting. Subsequently, five more platinum coils (GDC 2D: 6 mm/20 cm × 2, Tornado: 4/2 mm; GDC 2D: 5 mm/15 cm; Morpheus 3D: 6 mm/20 cm) achieved only stoppage of flow into the ophthalmic vein, and another six platinum coils (GDC 18–360°: 8 mm/20 cm; GDC 18–360°: 10 mm/30 cm; Tornado: 5/2 mm; Tornado: 4/2 mm × 2; Morpheus 3D: 6 mm/20 cm) were injected to achieve significant fistula obstruction. Although the final angiography (
Figure 2C) still revealed a significant fistula flow into petrosal sinus, it was decided to wait before performing a second embolization. After the first embolization, the patient showed progressive improvement of neurological function. On the 14th day of admission, his status had improved from stupor to drowsiness and the right-sided hemiparesis had improved to 4/5.
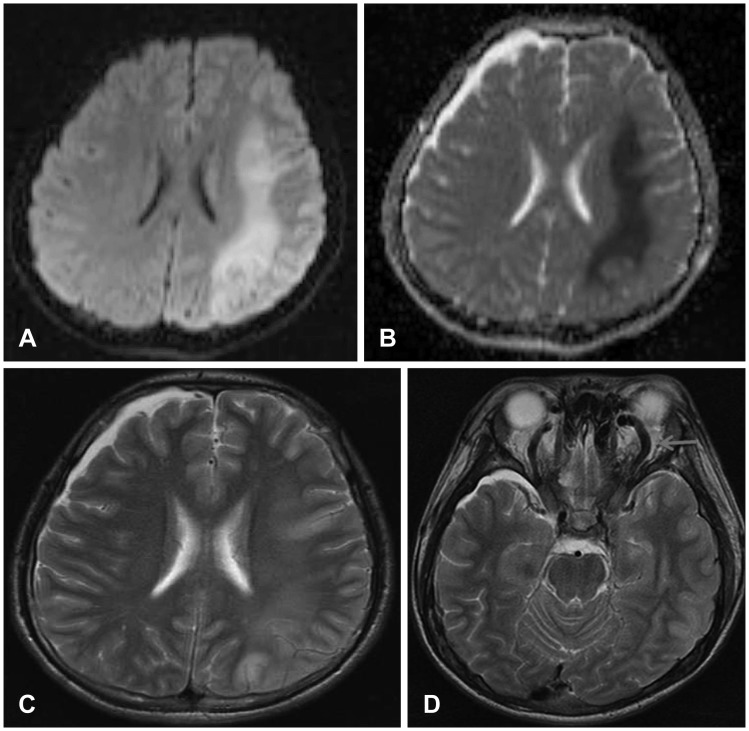 | FIGURE 1Diffusion weighted image (A) showing high signal intensity in the subcortical white matter of left centrum semiovale and lower temporo-occipital area. (B) Apparent diffusion coefficient map signal reduction is seen in the same region. (C) T2-weighted axial magnetic resonance imaging (MRI) demonstrating high signal intensity in the same region. (D) T2-weighted axial MRI demonstrating the dilated tortuous superior ophthalmic vein.
|
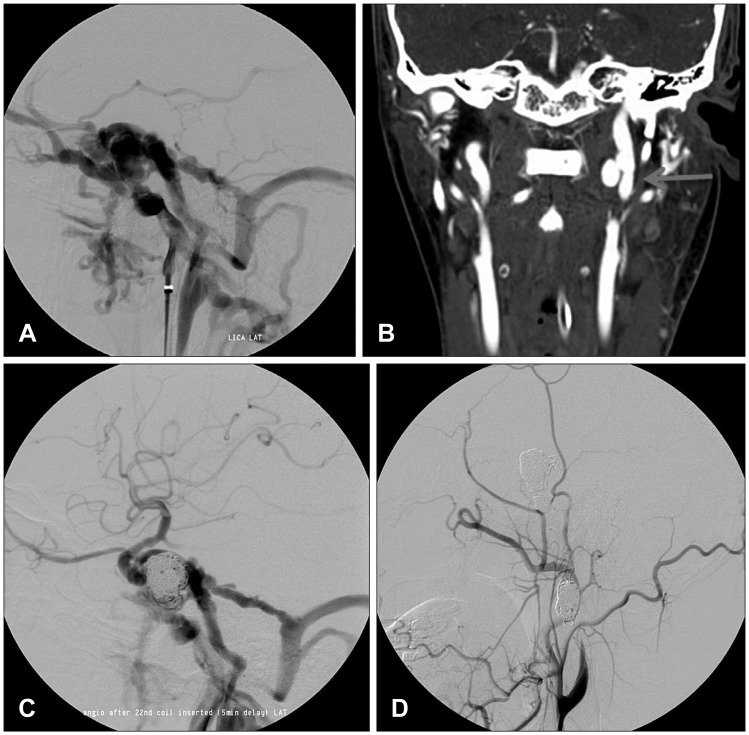 | FIGURE 2(A) Left internal carotid artery (ICA) angiogram showing a direct carotid cavernous fistula that drains into the superior ophthalmic vein, sphenoparietal sinus, and inferior petrosal sinus. (B) Intracranial computed tomography angiography demonstrating a large pseudoaneurysm arising from the left upper cervical ICA. (C) Postembolization angiography revealing a significant fistula flow into petrosal sinus. (D) Final angiography after second embolization showing complete occlusion of left ICA and a successful embolization of the pseudoaneurysm.
|
Seven days after the initial embolization, his status had improved from drowsiness to alertness and the second coil embolization was attempted, this time using a trans-venous approach. Briefly, we tried to place Nester coils (Cook Medical Inc., Bloomington, IN, USA) into the fistulous sac four times, but the fourth Nester coil intruded into the proper ICA tube, resulting in a mounting decrease in anterograde flow to the middle cerebral artery. Therefore, we attempted intra-arterial occlusion of the fistula and ICA. During this intervention, the left ICA was occluded and sacrificed to completely close the fistula using coils (GDC 2D: 6 mm/20 cm × 1; GDC 18–360°: 5 mm/15 cm × 2; 3 Nester coils). Postoperative right ICA injection showed adequate collateral-flow through the anterior communicating artery from the contralateral ICA, without retrograde blood steal to the CCF. In addition, the 15-mm cervical ICA pseudoaneurysm was successfully embolized with coils (GDC 2D: 15 mm/40 cm × 2, 10 Nester coils) (
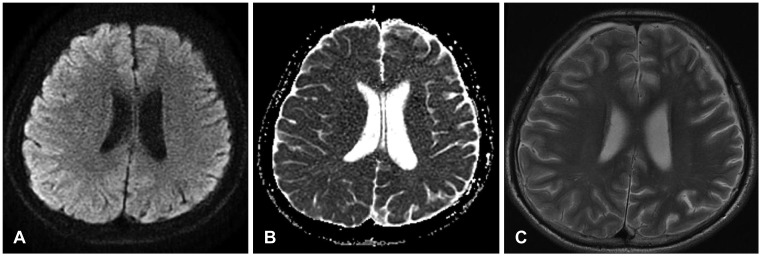
Figure 2D). The patient recovered well with no neurological compromise after the second embolization. On day 35 after his initial presentation, the patient had complete neurological recovery (GCS 15) and a follow-up brain MRI revealed complete reversal of the diffusion restriction in the left centrum semiovale and splenium of the corpus callosum (
Figure 3).
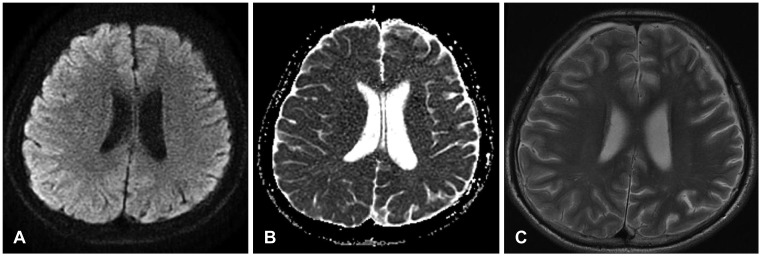 | FIGURE 3A 5-week follow-up (A) diffusion weighted image, (B) apparent diffusion coefficient map, and (C) T2-weighted image demonstrating complete reversal of diffusion restriction in the left centrum semiovale.
|
Go to :

Discussion
Traumatic CCF is an uncommon condition, occurring in only 0.1% to 0.17% of TBI cases.
5) It occurs when there is a leakage of arterial flow from the carotid artery into the venous system caused by direct injury from the skull base fracture or indirect injury from subsequent stretching forces.
25) In CCF, venous drainage patterns and shunt flow rate influence the clinical presentation. Anterior drainage can lead to orbital congestive symptoms including orbital bruit, chemosis, and pulsating exophthalmos.
234567911) Posterior and inferior drainage may induce cranial nerve palsy (cranial nerve III, IV, V, and VI) due to rising pressure within the cavernous sinus and compression of its contents.
234567911) Traumatic CCFs are usually high-flow and direct-type fistulae, and treatment is therefore always recommended. The gold standard for treatment utilizes the transarterial route, with occlusion of the fistula and preservation of blood flow through the ICA, using a detachable balloon or detachable platinum coils.
5)
In recent years, reversible lesions with transiently reduced diffusion have been reported in patients with various entities including encephalopathy, TBI, cytotoxic lesions of the corpus callosum, and dAVF.
1468) High signal intensity on DWI and decreased ADC values correspond to a decreased movement of highly mobile extracellular water molecules due to their shifting into intracellular compartment, i.e. restricted diffusion.
1) Hyperintense signals on T2 and fluid attenuated inversion recovery imaging are also observed within the lesions.
8) This diffusion restriction reflects cellular edema, which is considered to result in an irreversible lesion and cellular death.
1) In these previous case, the lesions disappeared or improved significantly on follow-up MRI performed a couple of months later.
DAI is a diffuse brain injury leading to cytotoxic edema in the intramyelinic white matter and reversibility of diffusion restriction due to abundant intracellular glutamate.
110) dAVF is a heterogeneous collection of conditions characterized by arteriovenous shunting from dural vessels and has been reported to leads to reversible diffusion restriction due to venous hypertension and/or encephalopathy.
46) Venous hypertension resulting from retrograde cortical venous drainage of dAVF could decrease the local perfusion pressure and cerebral blood flow, thereby causing cytotoxic edema that leads to diffusion restriction.
4) In the present case, the patient remained stuporous until the 13th hospital day even though initial CT showed only minimal right frontal subdural hemorrhage and he was diagnosed with DAI. On the 10th day of admission, however, right-sided hemiparesis occurred and brain MRI showed diffusion restriction in the left centrum semiovale white matter and lower temporo-occipital area extending to the splenium of the corpus callosum. Therefore, we assumed that reversible restricted diffusion could result from a high-flow direct CCF because of the following reasons. First, DWI in DAI patients often shows reversible restricted diffusion in the splenium of the corpus callosum or the genu.
10) Second, the diffusion restriction in the left centrum semiovale white matter was consistent with left-sided large CCF. Right-sided hemiparesis could have occurred as a result of blood flow being diverted away from the ICA, with the collaterals insufficient to supply the ipsilateral hemisphere.
In our case, cerebral angiography confirmed a high-flow direct CCF with complete blood steal and an initial brain MRI suggested diffusion restriction. Interestingly, the diffusion restriction was completely reversed after treatment of the CCF. Although high-flow shunting may cause cerebral ischemia due to steal phenomena, venous congestion or venous hypertension, altered venous drainage is more likely to produce severe reduction of cerebral blood flow resulting in diffusion restriction, because complete reversal of the diffusion restriction could be achieved even after total occlusion of the left ICA.
Go to :

Conclusion
Post-traumatic CCF is a direct, high flow fistula and can present with diffusion restriction on MRI due to cytotoxic edema associated with decreased cerebral blood flow secondary to steal phenomena, venous congestion, or venous hypertension resulting in lower local perfusion pressures. The diffusion restriction on DWI caused by traumatic CCF could be reversed if the lesion is treated adequately and expeditiously.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download