This article has been
cited by other articles in ScienceCentral.
Abstract
Traumatic pseudoaneurysms of middle meningeal artery (MMA) and medial sphenoid wing dural arteriovenous fistula (dAVF) are rare. These lesions usually result from traumatic brain injury, and associated with skull fracture. In this paper, the authors report a case of a patient with a ruptured traumatic pseudoaneurysm of MMA and medial sphenoid wing dAVF presented with an intracerebral hemorrhage in the left temporal region and subarachnoid hemorrhage. These lesions were completely obliterated by endovascular treatment, and the patient was recovered without any neurologic deficit. However, 18-day after the procedure, delayed neurologic deficits were developed due to cerebral vasospasm.
Go to :

Keywords: Aneurysm, false, Arteriovenous fistula, Subarachnoid hemorrhage, traumatic
Introduction
Traumatic pseudoaneurysm of middle meningeal artery (MMA) is uncommon and possible cause for intracerebral hemorrhage (ICH).
146) Medial sphenoid wing dural arteriovenous fistula (dAVF) is rare disease entity, also.
1011) These lesions usually developed as a result of head trauma, and associated with skull fracture, and could be treated by using endovascular procedures. Symptomatic cerebral vasospasm occurs in <20% of patients with traumatic subarachnoid hemorrhage (SAH). However, in the case of traumatic SAH, surveillance for cerebral vasospasm was not routinely performed and there is no guidance for these. We present a case of a patient with a ruptured traumatic pseudoaneurysm of MMA and medial sphenoid wing dAVF presented with an ICH in the left temporal region and SAH. The patient was treated by using endovascular treatment and recovered without any neurologic deficits. However, delayed neurologic deficits were developed due to cerebral vasospasm of branches of middle cerebral artery (MCA).
Go to :

Case Report
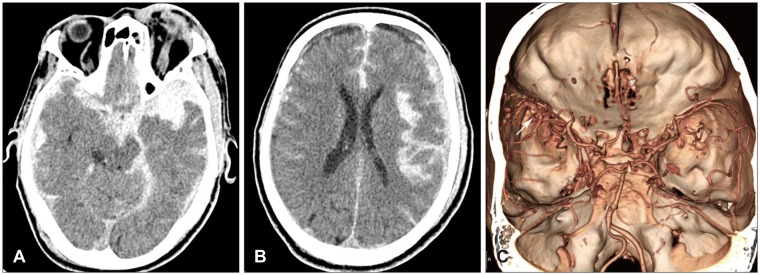
A 69-year-old male patient presented with stuporous mentality after fall from 2-meter height. On admission, the patient's Glasgow Coma Scale (GCS) score was 7/15. Neurological exam revealed no further abnormalities. Brain computed tomography (CT) scan revealed an ICH in the left temporal lobe with diffuse SAH and subdural hemorrhage (
Figure 1A and B). A brain CT angiography revealed a pseudoaneurysm of MMA (
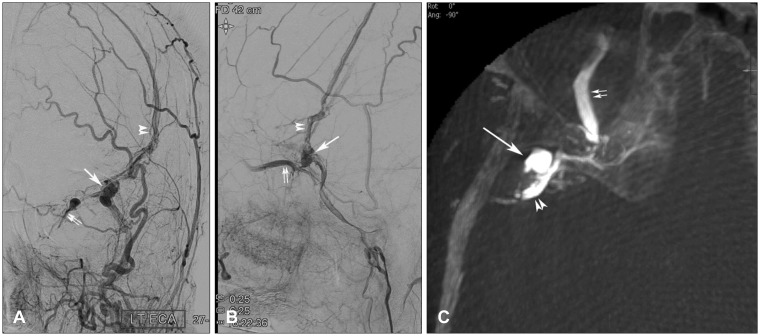
Figure 1C). Sequentially, the patient was submitted to cerebral angiography and the left external carotid angiogram revealed a pseudoaneurysm arisen from the anterior branch of the MMA accompanied by dAVF at the middle segment of sphenoid ridge (
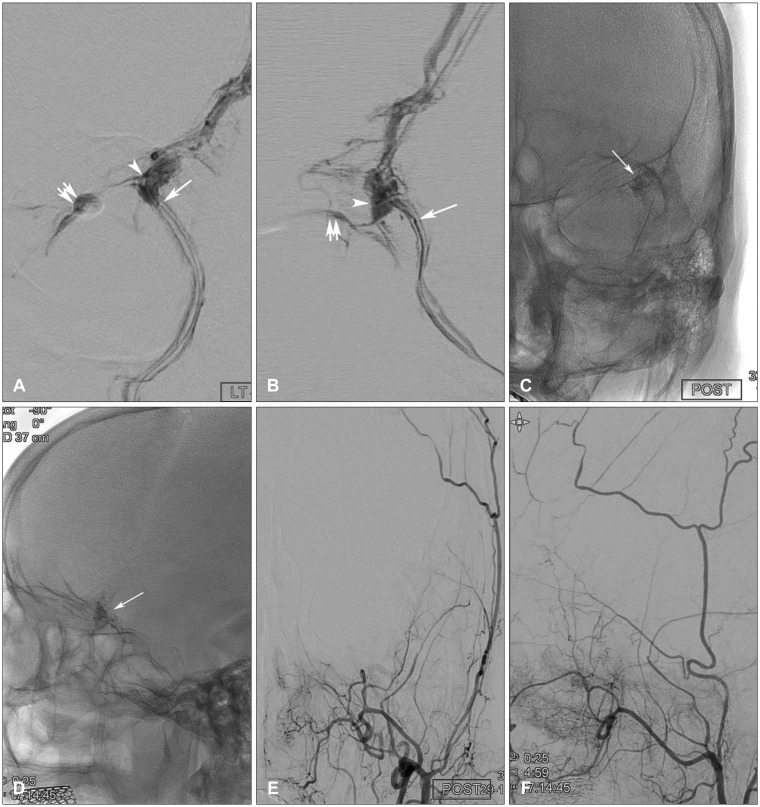
Figure 2). Through the right common femoral artery, a guiding catheter (Envoy 6 Fr; Cordis/Johnson & Johnson, Miami, FL, USA) was positioned in the left external carotid artery. We carefully naviated a microcatheter pre-shaped 45 degrees (Excelsior SL-10; Stryker Neurovascular, Fremont, CA, USA) under the guidance of a 0.014-inch microguidewire (Synchro 14; Stryker Neurovascular) to reach the juxtaproximal to the pseudoaneurysm via MMA. After the confirmation of the appropriate position of the microcatheter via repetitive superselective angiography (
Figure 3A and B), embolization of a pseudoaneurysm and MMA was performed using 25% n-butyl cyanoacrylate (NBCA) (Hystoacryl; B. Braun, Melsnagen, Germany) mixed with iodized oil (Lipiodol; Guerbet, Aulnay-sous-Boid, France). We achieved angiographically complete occlusion of a pseudoaneurysm and dural AVF (
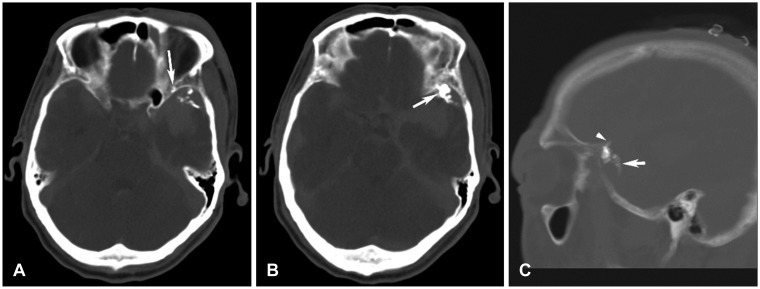
Figure 3). Follow-up brain CT scan showed no significant hematoma enlargement and well penetrated glue cast at the all the vascular lesions (
Figure 4).
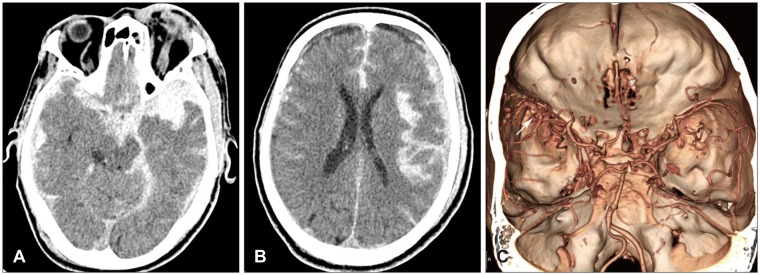 | FIGURE 1Initial radiological images after trauma. (A, B) Brain computed tomography (CT) showed intracerebral hemorrhage in the left temporal lobe with diffuse and large amount of subarachnoid hemorrhage and subdural hemorrhage at the left hemisphere. (C) Brain CT angiography revealed that abnormal vascular structure, considered as pseudoaneurysms, at the distal segment of the left lesser sphenoid ridge (arrow).
|
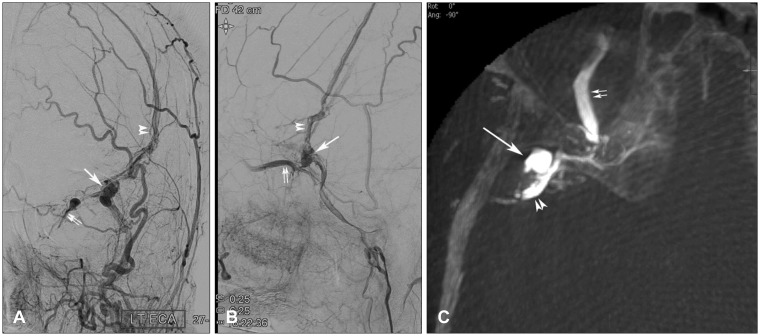 | FIGURE 2Left external carotid angiogram. (A) anteroposterior view, (B) lateral view showed a multilobulated pseudoaneurysm at the distal segment of the lesser sphenoid ridge (large arrow). Retrograde contrast filling through the left superior ophthalmic vein (double arrow) and middle meningeal artery-middle meningeal vein fistula (double arrow head) was also shown. (C) Cone-beam computed tomography image showed a multilobulated pseudoaneurysm at the distal segment of the lesser sphenoid ridge (large arrow) and the left superior ophthalmic vein (double arrow). Between these, complex vascular connections at the lesser sphenoid ridge resulting in medial sphenoid ridge dural arteriovenous fistula was shown.
|
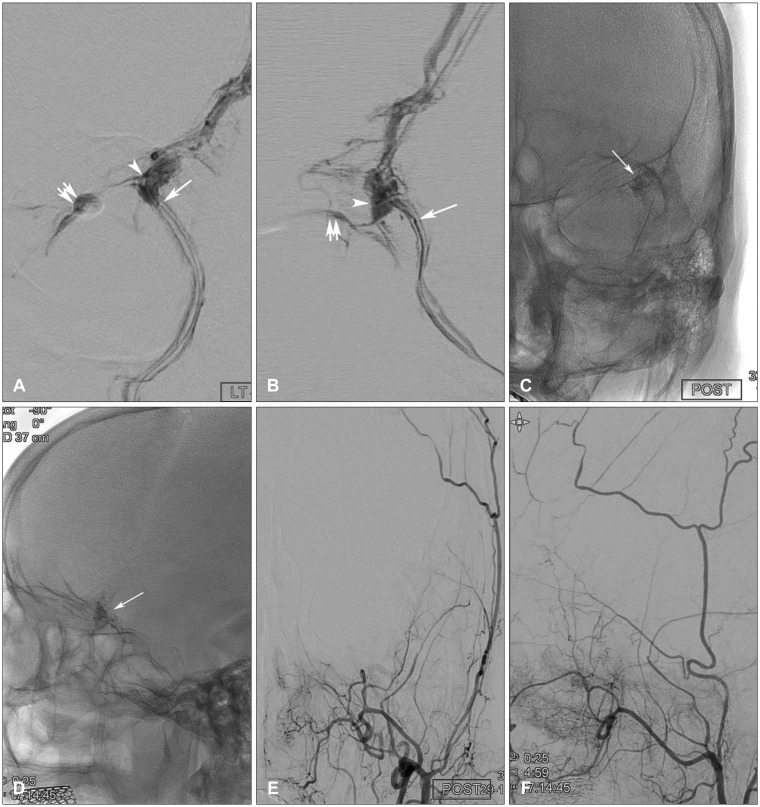 | FIGURE 3Superselective angiogram of the left middle meningeal artery (MMA). (A) anteroposterior view, (B) lateral view revealed an appropriate position of distal microcatheter tip (large arrow) showing a pseudoaneurysm (arrow head) and retrograde contrast filling through the left superior ophthalmic vein (double arrow). (C, D) N-butyl cyanoacrylate cast after embolization (large arrow). (E, F) Post-embolization external carotid angiogram showed complete occlusion of pseudoaneurysm, medial sphenoid ridge dural arteriovenous fistula and MMA-middle meningeal vein fistula.
|
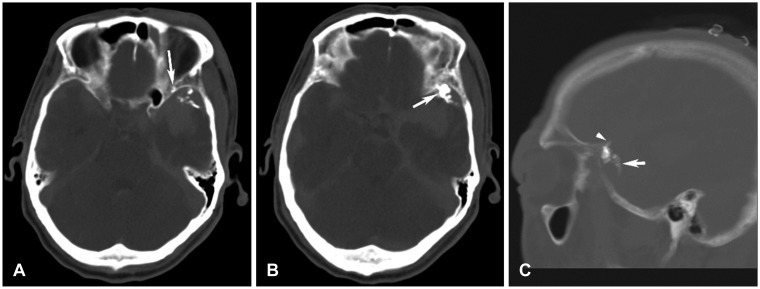 | FIGURE 4(A) Post-embolization computed tomography showed n-butyl cyanoacrylate cast at the dural vascular channel (arrow), (B) psneudoaneurysm (arrow), (C) proximal and distal segment of the left middle meningeal artery according to a pseudoaneurysm (arrow and arrow head, respectively).
|
The patient presented an improvement in consciousness for GCS score 15 after 12 days. However, at the 18-day after the procedure, the right side weakness and dysarthria were developed. Brain CT angiography and subsequent left internal carotid angiography revealed cerebral vasospasm at the distal segment of MCA with multiple low densitied at the left MCA territories (
Figure 5). Cerebral vasospasm was treated using intra-arterial (IA) nimodipin infusion, and it was improved. At discharge, dysarthria was improved, but right side weakness was remained (Grade 3).
 | FIGURE 5Radiologic images 15 days after endovascular embolization with motor weakness and dysarthria. (A, B) Brain computed tomography (CT) showed multifocal low density lesions at the left middle cerebral artery (MCA) territory. (C) CT angiography revealed sparse vasculature of distal segment of the left MCA preserving M1 patency (large arrows). (D) Left internal carotid angiogram showed multiple luminal irregularities and narrowing at the distal segment of MCA (small arrows).
|
Go to :

Discussion
Usually, traumatic pseudoaneurysms of MMA cause extradural hematoma.
7) However, pseudoaneurysm of the MMA, even though rare, has been considered as a possible etiology of ICH.
149) Pseudoaneurysms of MMA tend to gradually enlarge, resulting in a delayed rupture and clinical deterioration, which is associated with a mortality up to 50%.
16) These lesions usually associated with skull fracture. In the present case, however, skull fracture was not detected by brain CT and skull X-ray. On the other hand, angiogram showed a pseudoaneurysm of MMA and medial sphenoid wing dAVF accompanied by MMA-middle meningeal vein (MMV) fistula. Arterial contributories of the lesser sphenoid wing arise predominantly from the MMA, and abnormal connection between MMA and sphenoparietal sinus result in medial sphenoid wing dAVF.
10) These lesion also associated with skull fracture or blunt head injury.
811) In this case, we considered that a pseudoaneurysm of MMA and medial sphenoid wing dAVF were developed by blunt head trauma, and it was treated by using NBCA. We achieved complete obliteration of pseudoaneurysm and dAVF.
Nowadays, neurointerventional therapy is widely used as the first approach for some traumatic neurovascular lesions, being minimally invasive, feasible, and effective.
1) In term of endovascular techniques treating a pseudoaneurysm, a definitive treatment can be obtained with occlusion of the proximal parent vessel segment, the pseudoaneurysm lumen, and the distal segment, avoiding the risk of distal retrograde filling. Definitive embolic agents are obviously preferable, with glue being the most used. Because the adhesive characteristic of NBCA, only one session of procedure is permitted per one selected feeding artery. Especially, medial sphenoid wing dAVF was accompanied in the present case, it is important to identify the exact vascular structure around the lesions for the position of the microcatheter. To achieve complete occlusion of a pseudoaneurysm and medial sphenoid wing dAVF via one session of glue injection, we performed repetitive superselective angiography to identify the exact vascular structure of pseudoaneurysm and dAVF, and confirm the most appropriate position of the microcatheter. Finally, we could achieve a complete occlusion of all the vascular lesions using one session of procedure. Postoperative CT revealed glue cast at the pseudoaneurysm, dural vascular channel, proximal and distal segment of MMA according to a pseudoaneurysm.
In this case, delayed neurologic deterioration was developed after full recovery. Angiogram revealed vasospasm of the left MCA, especially distal segment of MCA was mainly involved. There are important differences and similarities between cerebral vasospasm that occurs as a result of traumatic brain injury compared with aneurismal SAH, e.g. 20% to 30% of aneurismal SAH, and less than 20% with traumatic brain injury.
25) For these reasons, even though SAH is accompanied, the importance of vasospasm usually underestimated in case of traumatic brain injury, and any practice guidelines do not recommend routine surveillance for cerebral vasospasm in patient with traumatic brain injury of any severity.
2) Moreover, there is no suggested monitoring period for symptoms of delayed cerebral ischemia as there is for patient with aneurismal SAH.
3) In the same manner as aneurysmal SAH, high suspicion level for cerebral vasospasm should be maintained in case of traumatic SAH.
Go to :

Conclusion
Ruptured pseudoaneurysm of MMA and medial sphenoidal ridge dAVF is uncommon, but a ruptured pseudoaneurysm has a potential aggressive natural history. Therefore, once diagnosed, it must be treated. These lesions usually treated by using NBCA, and identification of an exact vascular structures and appropriate position of microcatheter is crucial to achieve complete occlusion of the pseudoaneurysm and dAVF using only one session of glue injection. In addition, cerebral vasospasm should not be neglected in case of traumatic SAH after complete obliteration of primary focus.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download