Abstract
It is not a common case for neurosurgery department and the other departments to perform joint operation at the same time. Patients with severe head injury are a condition in which vital signs are unstable due to severe brain swelling and increased intracranial pressure, and emergency surgery is required. A 44-year-old man visited the trauma center with a motorcycle accident. The Glasgow Coma Scale score at the time of emergency department was 3 points, and the pupil was fixed at 6 mm on both sides. His medical history was unknown. His vital signs including blood pressure (BP), heart rate, respiratory rate and oxygen saturation were stable. Associated injuries included multiple fractures of whole body. Brain computed tomography revealed subarachnoid hemorrhage, intraventricular hemorrhage and severe cerebral edema. During the preparation of the craniectomy, abdominal ultrasonography performed because of decreased BP resulted in a large amount of hemoperitoneum. The bi-coronal craniectomy and splenectomy were performed simultaneously for about 4 hours. After fifty days of treatment, he was discharged with Glasgow Outcome Scale-extended 4 points and is undergoing rehabilitation. In severe polytrauma patients, active concurrent surgery is a good method to save their lives.
Go to : 
The polytrauma patients with severe head injury have a high mortality rate. Watson and colleagues19) reported that 30% of patients with severe splenic injuries had accompanying severe traumatic brain injury (TBI) of Glasgow Coma Scale (GCS) score ≤8. Nonoperative treatment of blunt splenic injuries is supported in hemodynamically stable patients, but splenic injury, which caused hypotension, requires splenectomy.918)
We report a rare case of concurrent operation of craniectomy and splenectomy as initial treatment in severe traumatic head injury.
Go to : 
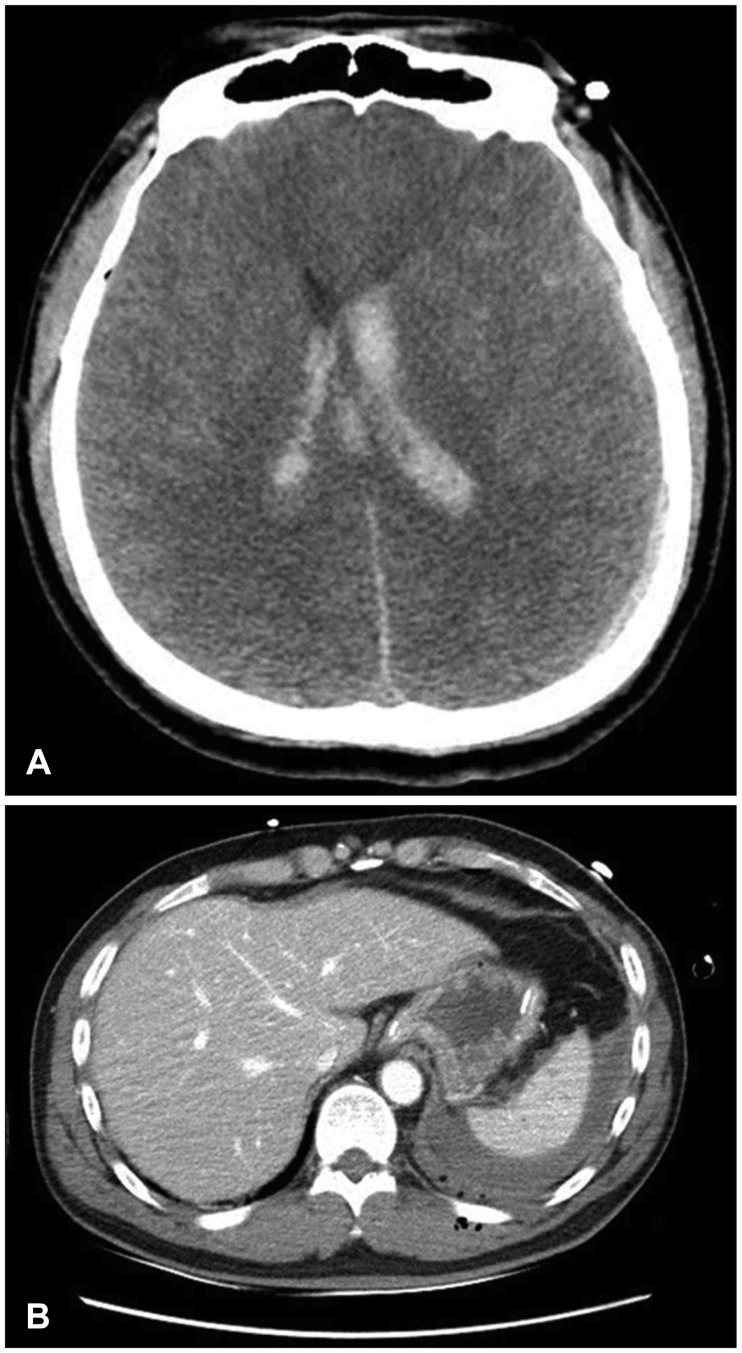
A 44-year-old man visited the trauma center with a motorcycle accident. The GCS score at the time of emergency department was 3 points, and pupils were fixed at 6 mm on both sides. He was unconscious, and hard to identify his medical history. Initial blood pressure (BP) was 135/85 mmHg, heart rate (HR) was 100 times/min, respiratory rate was 24 times/min, body temperature was 37.6℃ (99.68°F), and oxygen saturation was 95%. Also, it was identified that hemoglobin, hematocrit and platelet counts were 14.2 g/dL, 42.5% and 350×103/µL at laboratory test. Associated injuries included multiple fractures of whole body. Brain computed tomography (CT) revealed subarachnoid hemorrhage, intraventricular hemorrhage and severe cerebral edema and a small amount of hemoperitoneum was detected in abdominal CT (Figure 1).
During the preparation of the craniectomy in the operating room, BP was checked to 85/50 mmHg and HR was changed 131 times/min, and abdominal ultrasonography was performed emergently. As the result of that, a large amount of hemoperitoneum was confirmed. The blood tests at that time showed that hemoglobin and hematocrit dropped to 8 g/dL and 23.1%.
Hemoperitoneum was found to be the cause of hemodynamically unstable condition, and decompressive craniectomy was also urgently required to control cerebral edema and intracranial pressure (ICP). The bi-coronal craniectomy with duroplasty and splenectomy with vessel ligation were carried out simultaneously for about 4 hours. Because neurosurgeons and trauma surgeons had difficulty in secure their surgical space at the same time, the modified Mayo stand was installed. The surgery was well done under the close observation of the anesthesiologist (Figure 2). After fifty days of treatment, he was discharged with Glasgow Outcome Scale-extended (GOS-E) 4 points and is undergoing rehabilitation therapy.
Go to : 
Severe trauma is the main cause of death among younger people. Annual deaths worldwide due to trauma are expected to increase from five million to more than eight million by 2020.10)
TBI contributes to immediate and complicated physiologic changes, including cerebral hemodynamics instability and elevated ICP. These changes cause secondary insults and unfavorable outcomes in TBI patients.8) Also, cardiovascular abnormality in severe head trauma have been well known.4) Sympathetic nervous hyperactivity as measured by plasma and urinary epinephrine and norepinephrine levels has been verified in brain injury and in other medical conditions.720) After TBI, hypotension, hypoxia and hypercapnia have been shown to result in secondary brain injury that can lead to increased mortality and disability.2) It is important to find out the main cause that the vital signs became unstable, because the prognosis of patients with severe TBI and a low GCS score depends on how early the essential function is supported.16)
The spleen is the most common injured organ by blunt abdominal trauma, especially when it is already pathologically enlarged.13) In most of the 20th century, splenectomy was the treatment of choice for splenic damages.12) Recently, many investigators have reported that their good results with nonoperative treatment in children and adults and in hemodynamically stable patients.318) Alabbasi et al.1) reported analysis to evaluate two strategies (instant splenectomy and nonoperative management) for managing hemodynamically stable patients with blunt splenic injuries and severe brain injury.1) The overwhelming post-splenectomy sepsis syndrome is one of the main reasons for the increased emphasis on splenic conservation in current literature. It is a frequent and acute complication with an incidence of up to 1% after splenectomy, and an associated mortality of 50% to 70%.17) The decision on the surgical treatment strategy depended on the severity-level of the splenic damage, on associated injuries as well as the cardiovascular situation of the patient.6)
Uncontrolled post-traumatic bleeding is the cause of potentially preventable death among injured patients.14) As a result of only head trauma as well as polytrauma, cerebral blood flow (CBF) irregularities vary abnormally from low to high.11) Low CBF leads to decreased brain metabolism and ischemia, whereas increased CBF deteriorates brain swelling and high ICP.15)
Hildebrand et al.6) suggested the surgical treatment in a hemodynamically instable patient with grade 2 or greater splenic injury through the therapy algorithm. Surgical treatment of brain injury was also required to control cerebral edema and ICP and to prevent secondary brain damages. Our case report demonstrates the first experience of simultaneous surgery for reasons of hemodynamical and neurological deterioration.
In 2009, Goldschlager et al.5) reported a case of simultaneous craniotomy and caesarean section on extreme situation of trauma.
Go to : 
References
1. Alabbasi T, Nathens AB, Tien H. Blunt splenic injury and severe brain injury: a decision analysis and implications for care. Can J Surg. 2015; 58:S108–S117. PMID: 26100770.

2. Badjatia N, Carney N, Crocco TJ, Fallat ME, Hennes HM, Jagoda AS, et al. Guidelines for prehospital management of traumatic brain injury 2nd edition. Prehosp Emerg Care. 2008; 12(Suppl 1):S1–S52. PMID: 18203044.

3. Brasel KJ, DeLisle CM, Olson CJ, Borgstrom DC. Splenic injury: trends in evaluation and management. J Trauma. 1998; 44:283–286. PMID: 9498498.
4. Clifton GL, Robertson CS, Kyper K, Taylor AA, Dhekne RD, Grossman RG. Cardiovascular response to severe head injury. J Neurosurg. 1983; 59:447–454. PMID: 6886758.

5. Goldschlager T, Steyn M, Loh V, Selvanathan S, Vonau M, Campbell S. Simultaneous craniotomy and caesarean section for trauma. J Trauma. 2009; 66:E50–E51. PMID: 19088560.

6. Hildebrand P, Roblick UJ, Schloricke E, Czymek R, Bruch HP, Bürk C. The role of organ preservation in the surgical therapy of traumatic spleen injury. Acta Chir Iugosl. 2011; 58:21–25.

7. Hörtnagl H, Hammerle AF, Hackl JM, Brücke T, Rumpl E, Hörtnagl H. The activity of the sympathetic nervous system following severe head injury. Intensive Care Med. 1980; 6:169–177. PMID: 7391345.

8. Leung LY, Wei G, Shear DA, Tortella FC. The acute effects of hemorrhagic shock on cerebral blood flow, brain tissue oxygen tension, and spreading depolarization following penetrating ballistic-like brain injury. J Neurotrauma. 2013; 30:1288–1298. PMID: 23461630.

9. Meguid AA, Bair HA, Howells GA, Bendick PJ, Kerr HH, Villalba MR. Prospective evaluation of criteria for the nonoperative management of blunt splenic trauma. Am Surg. 2003; 69:238–242. PMID: 12678481.
10. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997; 349:1498–1504. PMID: 9167458.

11. Obrist WD, Langfitt TW, Jaggi JL, Cruz J, Gennarelli TA. Cerebral blood flow and metabolism in comatose patients with acute head injury. Relationship to intracranial hypertension. J Neurosurg. 1984; 61:241–253. PMID: 6737048.
12. Pachter HL, Guth AA, Hofstetter SR, Spencer FC. Changing patterns in the management of splenic trauma: the impact of nonoperative management. Ann Surg. 1998; 227:708–717. discussion 717-709. PMID: 9605662.
13. Resende V, Petroianu A. Subtotal splenectomy for treatment of severe splenic injuries. J Trauma. 1998; 44:933–935. PMID: 9603106.

14. Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care. 2016; 20:100. PMID: 27072503.

15. Sarrafzadeh AS, Peltonen EE, Kaisers U, Küchler I, Lanksch WR, Unterberg AW. Secondary insults in severe head injury-do multiply injured patients do worse? Crit Care Med. 2001; 29:1116–1123. PMID: 11395585.

16. Stocchetti N, Furlan A, Volta F. Hypoxemia and arterial hypotension at the accident scene in head injury. J Trauma. 1996; 40:764–767. PMID: 8614077.

17. Traub A, Giebink GS, Smith C, Kuni CC, Brekke ML, Edlund D, et al. Splenic reticuloendothelial function after splenectomy, spleen repair, and spleen autotransplantation. N Engl J Med. 1987; 317:1559–1564. PMID: 3120008.

18. Velanovich V. Blunt splenic injury in adults: a decision analysis comparing options for treatment. Eur J Surg. 1995; 161:463–470. PMID: 7488658.
19. Watson GA, Rosengart MR, Zenati MS, Tsung A, Forsythe RM, Peitzman AB, et al. Nonoperative management of severe blunt splenic injury: are we getting better? J Trauma. 2006; 61:1113–1118. PMID: 17099516.

20. Wilmore DW, Long JM, Mason AD Jr, Skreen RW, Pruitt BA Jr. Catecholamines: mediator of the hypermetabolic response to thermal injury. Ann Surg. 1974; 180:653–669. PMID: 4412350.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download