1. Anderson PA, Froyshteter AB, Tontz WL Jr. Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. J Bone Miner Res. 2013; 28:372–382. PMID:
22991246.

2. Buchalter D, Kahanovitz N, Viola K, Dorsky S, Nordin M. Three-dimensional spinal motion measurements. Part 2: A noninvasive assessment of lumbar brace immobilization of the spine. J Spinal Disord. 1988; 1:284–286. PMID:
2980256.
3. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009; 361:557–568. PMID:
19657121.

4. Cha KH, Cho TG, Kim CH, Lee HK, Moon JG. Comparative study on the period of absolute bed rest of vertebral compression fracture. Korean J Spine. 2013; 10:144–148. PMID:
24757476.

5. Cherasse A, Muller G, Ornetti P, Piroth C, Tavernier C, Maillefert JF. Tolerability of opioids in patients with acute pain due to nonmalignant musculoskeletal disease. A hospital-based observational study. Joint Bone Spine. 2004; 71:572–576. PMID:
15589442.

6. Denaro V, Longo UG, Denaro L. Vertebroplasty versus conservative treatment for vertebral fractures. Lancet. 2010; 376:2071–2072. PMID:
21168046.

7. Esses SI, McGuire R, Jenkins J, Finkelstein J, Woodard E, Watters WC 3rd, et al. American academy of orthopaedic surgeons clinical practice guideline on: the treatment of osteoporotic spinal compression fractures. J Bone Joint Surg Am. 2011; 93:1934–1936. PMID:
22012531.
8. Farrokhi MR, Alibai E, Maghami Z. Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine. 2011; 14:561–569. PMID:
21375382.

9. Grond S, Radbruch L, Lehmann KA. Clinical pharmacokinetics of transdermal opioids: focus on transdermal fentanyl. Clin Pharmacokinet. 2000; 38:59–89. PMID:
10668859.
10. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009; 361:569–579. PMID:
19657122.

11. Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006; 6:479–487. PMID:
16934715.

12. Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010; 376:1085–1092. PMID:
20701962.

13. Lantz SA, Schultz AB. Lumbar spine orthosis wearing. II. Effect on trunk muscle myoelectric activity. Spine (Phila Pa 1976). 1986; 11:838–842. PMID:
3810302.
14. Li Y, Hai Y, Li L, Feng Y, Wang M, Cao G. Early effects of vertebroplasty or kyphoplasty versus conservative treatment of vertebral compression fractures in elderly polytrauma patients. Arch Orthop Trauma Surg. 2015; 135:1633–1636. PMID:
26559063.

15. Longo UG, Denaro V. Spinal augmentation: what have we learnt? Lancet. 2009; 373:1947. author reply 1947-1948. PMID:
19501742.

16. Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Joint Surg Br. 2012; 94:152–157. PMID:
22323677.
17. Lukert BP. Vertebral compression fractures: how to manage pain, avoid disability. Geriatrics. 1994; 49:22–26.
18. Lyles KW. Management of patients with vertebral compression fractures. Pharmacotherapy. 1999; 19:21s–24s. PMID:
9915558.

19. McGuire R. AAOS clinical practice guideline: the treatment of symptomatic osteoporotic spinal compression fractures. J Am Acad Orthop Surg. 2011; 19:183–184. PMID:
21368100.

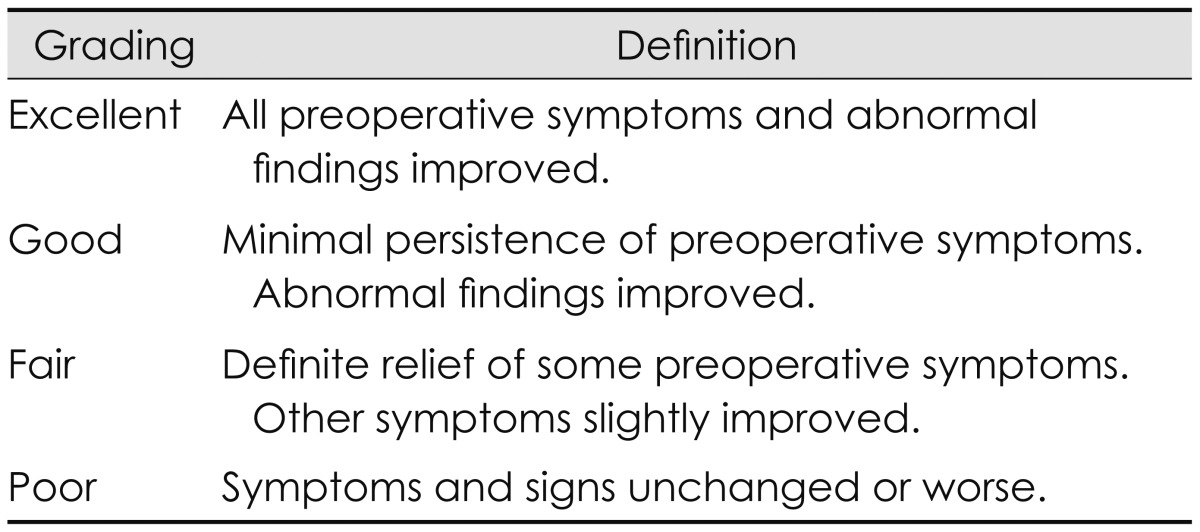
20. Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958; 166:23–28. PMID:
13491305.

21. Park JH, Kim JH, Yun SC, Roh SW, Rhim SC, Kim CJ, et al. Evaluation of efficacy and safety of fentanyl transdermal patch (Durogesic D-TRANS) in chronic pain. Acta Neurochir (Wien). 2011; 153:181–190. PMID:
20821238.
22. Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004; 83:177–186. PMID:
15043351.
23. Pfeifer M, Kohlwey L, Begerow B, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2011; 90:805–815. PMID:
21681065.
24. Pneumaticos SG, Triantafyllopoulos GK, Giannoudis PV. Advances made in the treatment of thoracolumbar fractures: current trends and future directions. Injury. 2013; 44:703–712. PMID:
23287553.

25. Prather H, Watson JO, Gilula LA. Nonoperative management of osteoporotic vertebral compression fractures. Injury. 2007; 38(Suppl 3):S40–S48. PMID:
17723791.

26. Rousing R, Andersen MO, Jespersen SM, Thomsen K, Lauritsen J. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine (Phila Pa 1976). 2009; 34:1349–1354. PMID:
19478654.
27. Soultanis KC, Mavrogenis AF, Starantzis KA, Markopoulos C, Stavropoulos NA, Mimidis G, et al. When and how to operate on thoracic and lumbar spine fractures? Eur J Orthop Surg Traumatol. 2014; 24:443–451. PMID:
24158740.

28. Stevenson M, Gomersall T, Lloyd Jones M, Rawdin A, Hernandez M, Dias S, et al. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for the treatment of osteoporotic vertebral fractures: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2014; 18:1–290.

29. Stillo JV, Stein AB, Ragnarsson KT. Low-back orthoses. Phys Med Rehabil Clin North Am. 1992; 2:57–94.

30. Voormolen MH, Mali WP, Lohle PN, Fransen H, Lampmann LE, van der Graaf Y, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol. 2007; 28:555–560. PMID:
17353335.
31. Wardlaw D, Cummings SR, Van Meirhaeghe J, Bastian L, Tillman JB, Ranstam J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009; 373:1016–1024. PMID:
19246088.

32. Wood KB, Li W, Lebl DR, Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014; 14:145–164. PMID:
24332321.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download