This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To evaluate the radiographic and clinical outcomes of percutaneous vertebroplasty (PVP) in patients with Kümmell's disease.
Methods
A retrospective review was conducted for 19 vertebrae in 18 patients, between January 2012 and June 2016. A visual analogue scale (VAS) score was used to determine each patient's subjective level of pain (0=no pain to 10=severe pain) preoperative, immediately postoperative and at the last follow-up (at least 12 months after PVP).
Radiographic parameters such as regional and global kyphotic angle, lumbar lordosis (LL), thoracolumbar junction (TLJ) angle, vertebral height, cement leakage, refracture, and adjacent level fracture were evaluated by the clinician preoperative, immediate postoperative and at the last follow-up.
Results
The mean VAS score significantly decreased after PVP and the decrease was maintained through to the final follow-up (p<0.05). However, the regional and global kyphotic angle, LL, and TLJ angle were not improved. Cement leakage was observed in 5 cases (26.3%): however, there were no cases of cement leakage into the spinal canal. No neurological deterioration was observed, even among patients with cement leakage. Adjacent level fractures were detected in 3 cases (15.8%).
Conclusion
PVP can be considered as an effective treatment option for pain relief and maintenance of sagittal balance in patients with Kümmell's disease.
Go to :

Keywords: Bone cement, Kümmell's disease, Vertebroplasty
Introduction
Kümmell's disease has been known since 1891, when Kümmell reported 5 cases of post-traumatic vertebral collapse syndrome with no signs or symptoms for months, or even years, after a minor trauma. Intravertebral vacuum phenomenon (i.e., cleft sign, an intravertebral gas cleft) is one of the common findings.
8) The difference between Kümmell's disease and vertebral compression fracture is that Kümmell's disease has progressive osteonecrosis of the anterior vertebral body with new bone formation and fibrosis around it.
Kaneda et al.
6) reported that surgical treatment was needed to prevent delayed neurologic symptoms in Kümmell's disease. Surgical treatment, including posterior fixation, has been preferred.
91015) However, there have been recent reports of the use of percutaneous vertebroplasty (PVP) or balloon vertebroplasty procedures rather than surgical treatment for Kümmell's disease.
1214)
This study was designed to evaluate the radiologic and clinical results of PVP for Kümmell's disease.
Go to :

Materials and Methods
From January 1, 2013 to June 30, 2016, 18 patients who underwent PVP for Kümmell's disease were enrolled in this study. A total of 19 vertebrae were evaluated (there were two lesions in 1 patient).
The average age at the time of the procedure was 80.3 years (range, 69–88 years). The average follow-up period was 14.4 months (range, 12–45 months). The sites of the disease were in the following thoracic (T) or lumbar (L) vertebrae: T9 (1 case). T11 (3 cases), T12 (6 cases), L1 (4 cases), L2 (2 cases), and L3 (3 cases). Patients with decreased height of the vertebral body and the presence of a gas cleft identified by plain radiography were evaluated for Kümmell's disease using magnetic resonance imaging (MRI) (
Figure 1). MRI criteria were as follow: collapse of the vertebral body, fracture line that appeared as a line of low signal intensity on T1-weighted images (WI) or a band-like high signal intensity on T2-WI, and, confirmation of a gas-filled cleft.
13) The diagnosis was confirmed if the radiologist's reading was consistent with these criteria.
 | FIGURE 1Magnetic resonance image (MRI) of Kümmell's disease. MRI of the lumbar spine shows a well-defined fluid signal intensity lesion surrounding dark rim with at L1 vertebral body. (A) Sagittal T2-weighted image (WI) showing band-like gas in the vertebral body. (B) Sagittal T1-WI showing a band-like low intensity signal. (C) Sagittal computed tomography image showing a recent compression fracture with retropulsion, and L1 intravertebral fluid and air-densities. (D) Sagittal X-ray image showing intravertebral gas cleft at L1.
|
PVP was performed under local anesthesia. The patient's position was fixed for maximal lordosis. Monitoring devices such as blood pressure, oxygen saturation, and electrocardiography were used. Antibiotics were administered 15 to 20 minutes before the procedure. A transpedicular approach was used to access the vertebral body under C-arm fluoroscopy. A Jamshidi needle was placed in the anterior one-third of the vertebral body and polymethyl methacrylate cement was injected through the needle. The mean amount of bone cement injected was 3.9 mL.
Each patient evaluated their level of pain using a visual analogue scale (VAS) ranging from 0=no pain to 10=severe pain. The clinician measured neurologic complications.
Radiologic parameters including regional kyphotic angle, global kyphotic angle, lumbar lordosis (LL), thoracolumbar junction (TLJ) angle, and the height of the anterior, middle, and posterior walls of the fractured vertebral bodies were measured. The presence of adjacent fractures and cement leakage were identified. LL was the Cobb's angle between the lower endplate of T12 and the upper endplate of the first sacral vertebra, and the TLJ angle was measured between the lower endplate of T10 and the upper endplate of L2.
Statistical analysis was performed using SPSS version 19.0 (IBM Corp., Armonk, NY, USA) and the results were analyzed using a paired student t-test.
Go to :

Results
Clinical outcomes
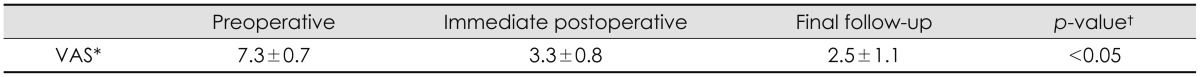
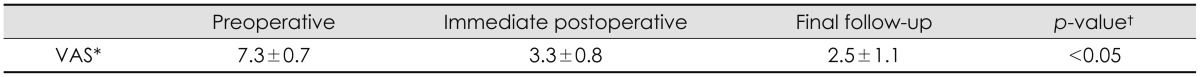
VAS scores are summarized in
Table 1. Back pain, as measured on the VAS, was statistically significantly reduced after PVP. Mean (± standard deviation) VAS scores preoperative, immediate postoperative, and final follow-up were 7.3±0.7, 3.3±0.8, and 2.5±1.1, respectively (
p<0.05).
TABLE 1
Comparison of VAS scores for back pain

Radiographic outcomes
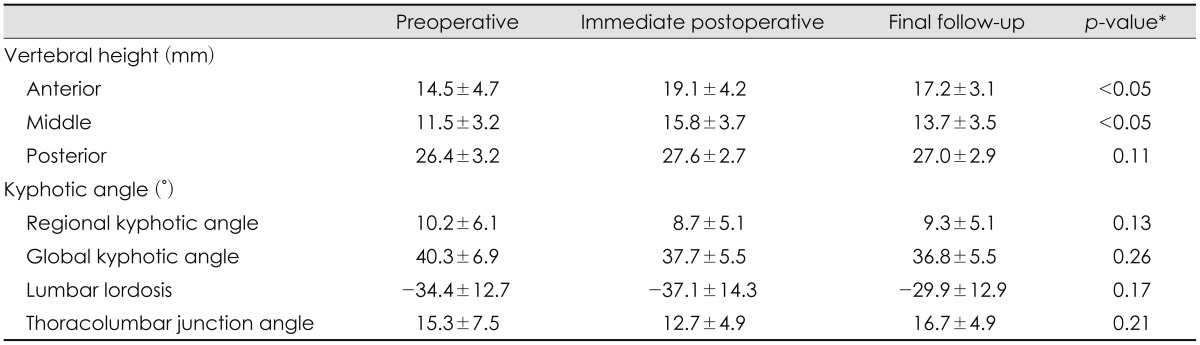
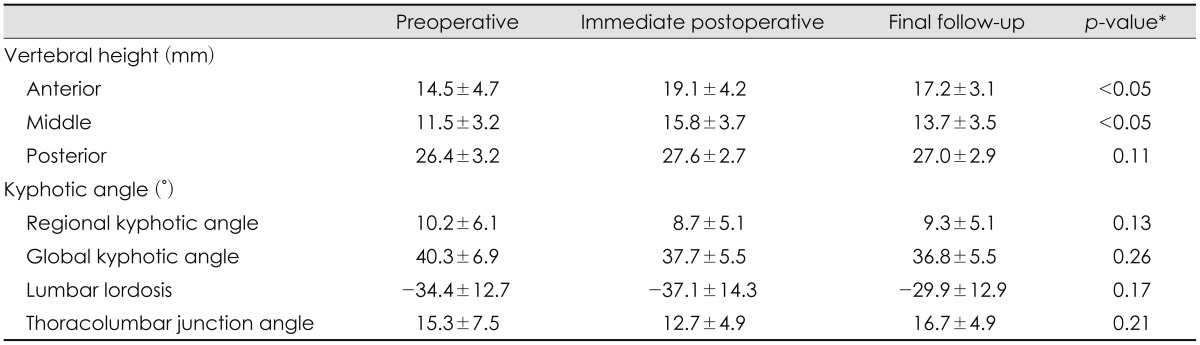
The results of the radiographic measurements are summarized in
Table 2. The heights of the anterior and middle vertebral bodies ware significantly increased after PVP (
p<0.05). There was no statistically significant change in the height of the posterior vertebral body (
p=0.11). No statistically significant changes were observed in the kyphotic angle measurements (
p=0.13).
TABLE 2
Radiographic parameters: measurements of vertebral height and kyphotic angle

Complications
Cement leakage occurred in 5 of 19 cases (26.3%). However, there was no leakage into the spinal canal. No neurologic complications, such as paraparesis or paresthesia of the lower limbs, were reported.
Adjacent level fracture
Adjacent level compression fracture occurred in 3 cases (15.8%). Two cases occurred in patients with cement leakage, and one case without cement leakage. The sites of the fractures were as follows: at L1 in a patient with Kümmell's disease at L3, at L2 in a patient with Kümmell's disease at L3, and in L1 in a patient with Kümmell's disease at T11. All were treated with additional PVP.
Go to :

Discussion
In 1891, Dr. Herman Kümmell reported a disease in which patients developed severe back pain and angular kyphosis ranging from months to years after experiencing a trauma that had been asymptomatic. Schmorl and Junghanns
11) demonstrated delayed post-traumatic vertebral fracture pathologically.
Kempinsky et al.
7) attempted post decompression via total laminectomy in Kümmell disease patient. Shikata et al.
12) performed decompression with total laminectomy and removed the bony fragments that were projecting posteriorly.
2) Kaneda et al.
6) reported that the lamina should be preserved because it is important for stabilization of sagittal balance. They reported that an anterior approach for decompression and reconstruction was effective in osteoporotic patients, and there was a very low incidence of instrumentation failure and very low morbidity.
In patients with Kümmell's disease with neurologic complications, surgical treatment is more appropriate. However, most patients with Kümmell's disease complain of back pain without neurologic symptoms. It has a risk for elderly patients to undergo surgery under general anesthesia. Conservative treatments such as bed rest and analgesics could be another treatment option for these patients. However, the long-term immobilization might lead to secondary complications such as pneumonia, pulmonary embolism, and pressure sores.
5)
Since Deramond et al.
3) successfully treated vertebral hemangioma using PVP and bone cement in 1984, PVP has been used to relieve pain by stabilizing the vertebral body. However, because of the characteristic osteonecrosis and vacuum phenomenon associate with Kümmell's disease, it was generally considered that PVP would result in leakage after the cement injection and was therefore not an appropriate treatment.
14) In spite of these concerns, many authors have described the efficacy of PVP for treating patients with Kümmell's disease. Cho et al.
2) reported that osteoporotic patients with Kümmell's disease without neurologic complications showed improvement in pain after PVP. Ha et al.
4) showed that PVP can effectively alleviate pain in patients with. Back pain decreased after PVP in our study as well.
With regards to radiographic outcomes, vertebral height increased after PVP for both the anterior and middle vertebrae and this was maintained until the last follow-up evaluation (
p<0.05). For some patients, this was as long as 45 months after the procedure. The parameters associated with sagittal balance, such as regional kyphotic angle, global kyphotic angle, LL, and TLJ angle were not corrected. However, there was no deterioration in the measurements and stasis was maintained at the follow-up assessment (
Figure 2).
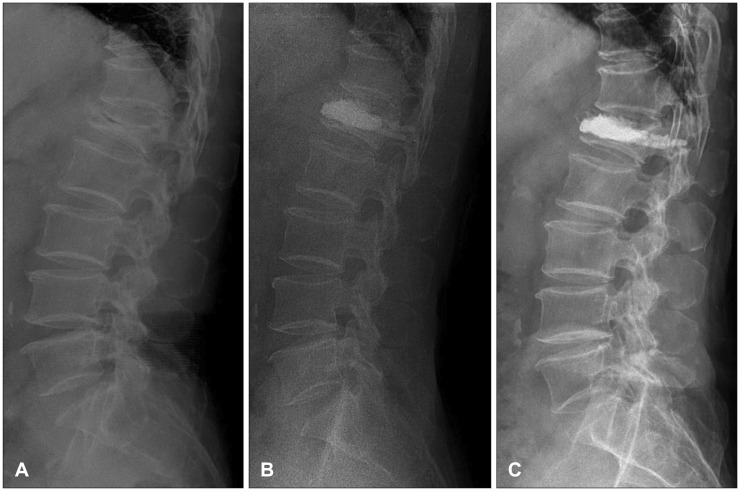 | FIGURE 2A case of Kümmell's disease treated with percutaneous vertebroplasty. (A) There was acute vertebral body collapse and diminished vertebral height at L1. An intravertebral vacuum cleft (intravertebral vacuum phenomenon) was seen on a preoperative radiograph as a horizontal linear radiolucency within the L1 vertebral body. (B) Immediate postoperative lateral standing plain radiography showed a cement mass in the L1 vertebral body. Bone cement was injected to fill the gap and stabilize the fractured site. (C) At the 1-year follow-up, a lateral standing plain radiography image showed no cement leakage and no adjacent vertebral body fracture. Bone cement was filled into the injection site.
|
The results of this study show that PVP for Kümmell's disease can alleviate back pain. In addition, the preoperative sagittal balance for these patients can be maintained, although it cannot be corrected.
The limitations of this study are as follows. First, the number of cases was small. Second, the follow up period was at least 1 year, but was not a long-term follow-up. Long-term follow-up is needed. Third, this study was a retrospective analysis.
Go to :

Conclusion
PVP can be considered as an effective treatment option for pain relief and maintenance of sagittal balance in patients with Kümmell's disease.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download