This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
Immediate contralateral epidural hematoma (EDH) and traumatic intracerebral hematoma (T-ICH) after craniectomy for traumatic subdural hematoma (SDH) are rare but devastating post-operative complications. Their clinical features and outcomes are not well studied. In this report, we present the clinical features and outcomes of immediate contralateral acute hematoma cases requiring a second operation.
Methods
This study includes 10 cases of immediate contralateral EDH and T-ICH following bilateral craniectomy for the evacuation of traumatic SDH and contralateral hematoma between 2004 and 2015. Their medical records and radiographic findings were reviewed and analyzed retrospectively.
Results
Ten of the 528 patients (1.89%) who underwent craniectomy for the evacuation of traumatic SDH developed post-operative EDH (n=5), T-ICH (n=5). The trauma was caused by a fall in 5 patients and by a traffic accident in 5 patients. The patients who suffered trauma due to pedestrian accidents died. Seven patients had a low admission Glasgow Coma Scale (GCS; GCS≤8) score in the preoperative state (average admission GCS, 7.7; average discharge GCS, 3.4; and average discharge Glasgow Outcome Scale, 2.0). Severe intra-operative brain swelling was noted in all patients, while skull fracture was observed in 8. Multiple associated injuries and medication for heart disease were characteristic of patients who died.
Conclusion
The prognosis of delayed contralateral hematoma was very poor. Multiple associated injuries, past medical history and traffic accidents, especially pedestrians were seemed to be associated with higher mortality rates. Finally, contralateral skull fractures can indicate high risk of delayed contralateral acute intracranial hematoma.
Go to :

Keywords: Decompressive craniectomy, Hematoma, subdural, acute, Skull fractures
Introduction
Immediate contralateral epidural hematoma (EDH) and traumatic intracerebral hematoma (T-ICH) after craniectomy performed for traumatic subdural hematoma (SDH) are rare but devastating post-operative complications.
8) A delayed diagnosis of post-operative contralateral hematoma can be fatal.
The requirement for bilateral surgery after decompressive craniectomy is rare (1–4%). Consequently, its clinical features and outcome are not well studied.
511) In addition, the management guidelines for contralateral hematoma have not been established.
5)
In this study, we present the clinical features and outcome of 10 cases of immediate contralateral acute hematoma that required a second operation. This study can augment the understanding of this rare postoperative complication.
Go to :

Materials and Methods
Study design
A total of 528 patients who underwent craniectomy for the evacuation of traumatic SDH between 2004 and 2015 were studied at the Gachon University, Gil Medical Center. Of these 528 cases, data from 10 patients with immediate contralateral EDH and T-ICH were analyzed retrospectively.
Clinical data collection
Medical records including demographic data, mechanism of trauma, associated injuries, past medical history, lab finding, cause of accident, brain swelling during hematoma evacuation, and neurological examination were reviewed and analyzed. The neurological parameters included the Glasgow Coma Scale (GCS) score, the Glasgow Outcome Scale (GOS) score.
Radiographic data
The radiographic findings, including the initial and post-operative computed tomography (CT) findings, were reviewed. In our medical center, all the patients routinely underwent post-operative CT scans in 5 minutes. The location of hematoma and skull fracture (if any), the Rotterdam CT score including the compression of basal cisterns, midline shift, epidural mass lesion, intraventricular blood, and/or traumatic subarachnoid hemorrhage were assessed.
Statistical analysis
Data were analyzed using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). One-way analysis of variance was performed to evaluate the relationship between prognosis and potential prognostic factors including past medical history, mechanism of injury and numbers of associated injury. In this study, Difference between pre-operative GCS and discharge GCS was used for evaluation of patient prognosis.
Go to :

Results
A total of 528 patients underwent craniectomy for the evacuation of traumatic subdural hemorrhage in a single center. Among them, 10 patients (1.89%) developed immediate post-operative EDH (n=5), T-ICH (n=5) (
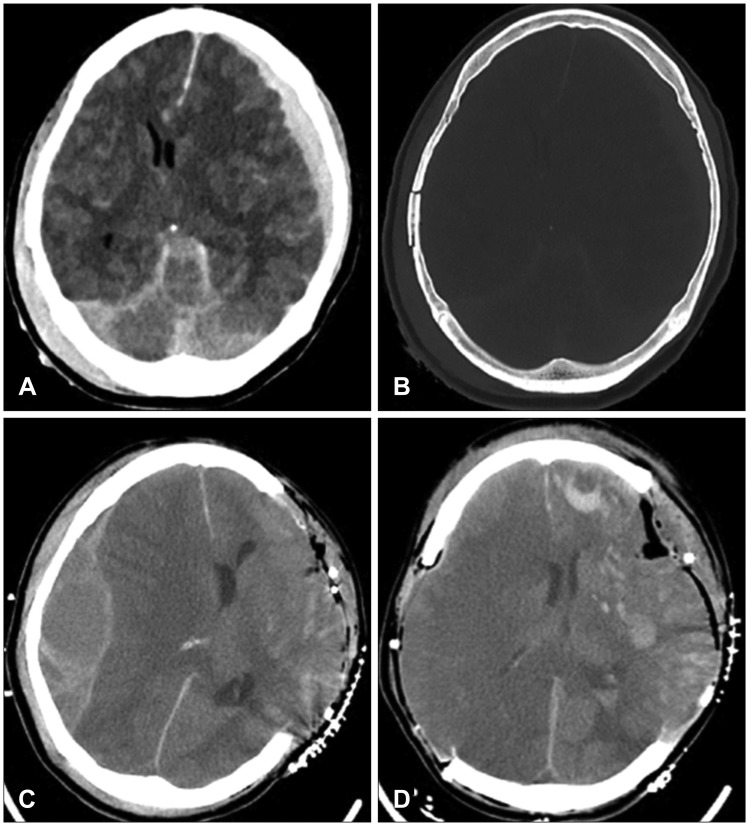
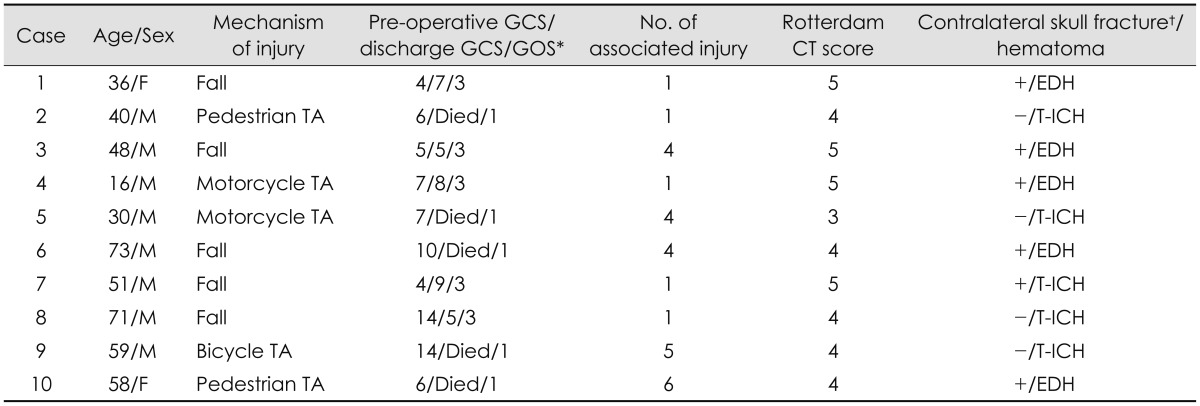
Figure 1). All patients received mannitol infusions to control the increased intracranial pressure (ICP) before hemorrhage evacuation. The clinical features and radiographic data are noted in
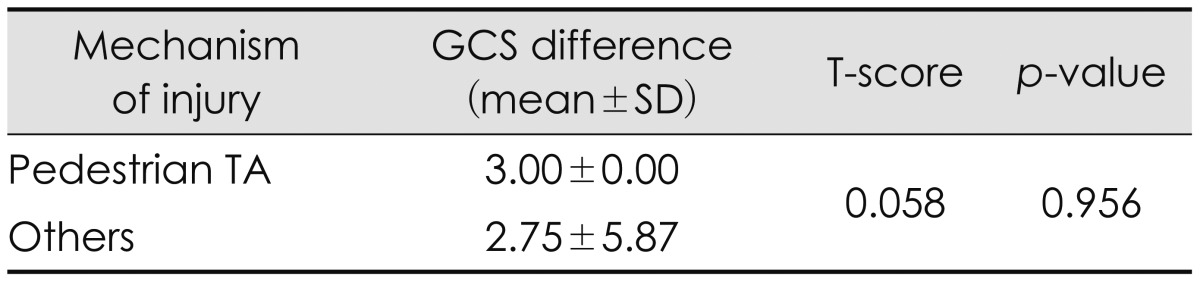
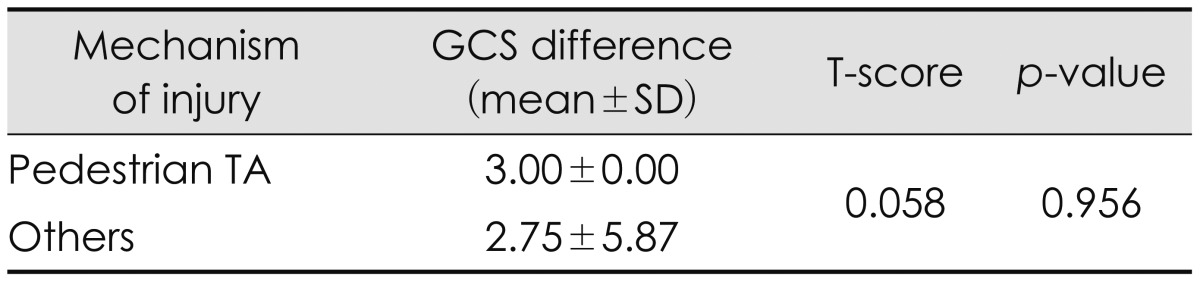
Table 1. The mechanisms of trauma were recorded as traffic accidents (n=5) and accidental falling (n=5). Among patients who suffered trauma due to traffic accidents, there were two cases of pedestrian traffic accidents, both there patient died. Mechanism of injury seems to be one of the important prognostic factors. However, in this study, it cannot show statistical significance (
Table 2). Seven patients had a low admission GCS (GCS≤8) score, while three patients had a high admission GCS (GCS>8) score in the preoperative state. The average admission GCS score was 7.7. Five patients died (50%) and the overall prognosis was very poor. The average discharge GCS score was 3.4, while the average discharge GOS score was 2.0. Displacement and severe intra-operative brain swelling were noted in all the patients. CT findings revealed, skull fractures in the contralateral hematoma in six patients, and the basal cisterns of all cases were compressed. The average Rotterdam CT score was 4.3. A skull fracture over the contralateral EDH was found in all the EDH cases (n=5).
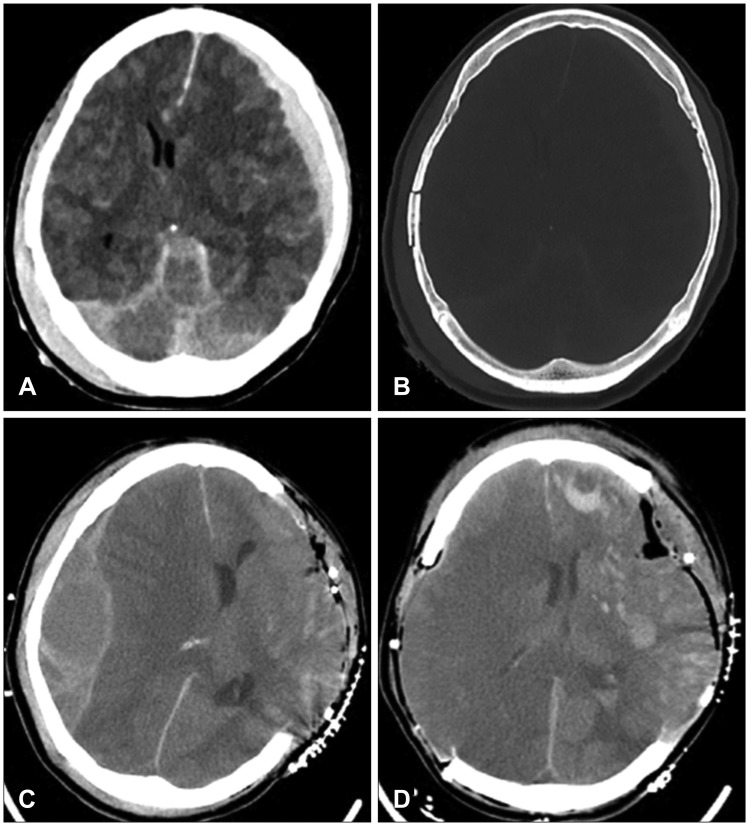 | FIGURE 1A 58-year-old woman requiring bilateral craniectomy caused by delayed epidural hematoma (EDH) after craniectomy for acute subdural hematoma (SDH). (A) Pre-operative computed tomography (CT) scan show traumatic SDH and subarachnoid hemoorhage on the left frontotemporoparietal region. (B) Pre-operative CT (bone setting) show skull fracture on right temporoparietal bone. (C) Post first operative CT show left craniectomy state and contralateral EDH. (D) CT taken after bilateral craniectomy.
|
TABLE 1
Clinical features and radiographic data of 10 cases with delayed contralateral acute intracranial hematoma after decompressive surgery
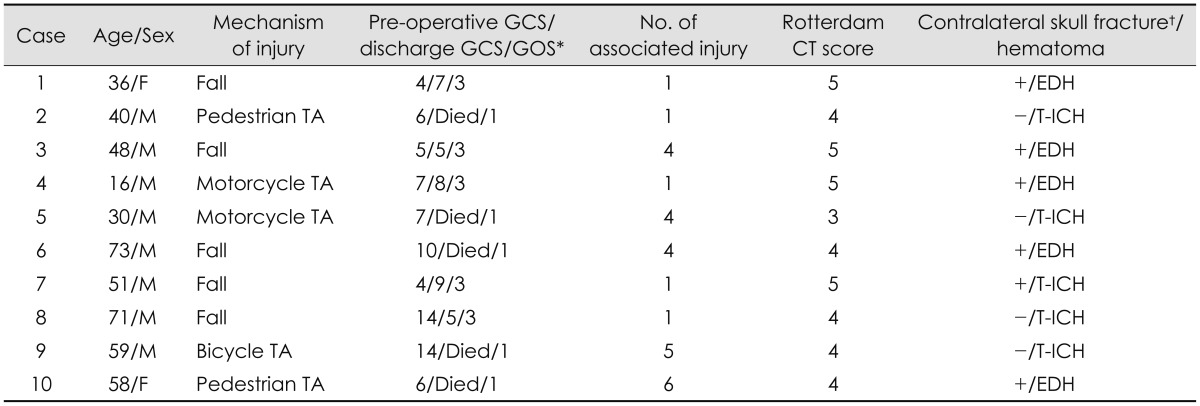

TABLE 2
Comparisons of difference between pre-operative GCS and discharge GCS from patients who with pedestrian traffic accident and patients who have other trauma mechanisms

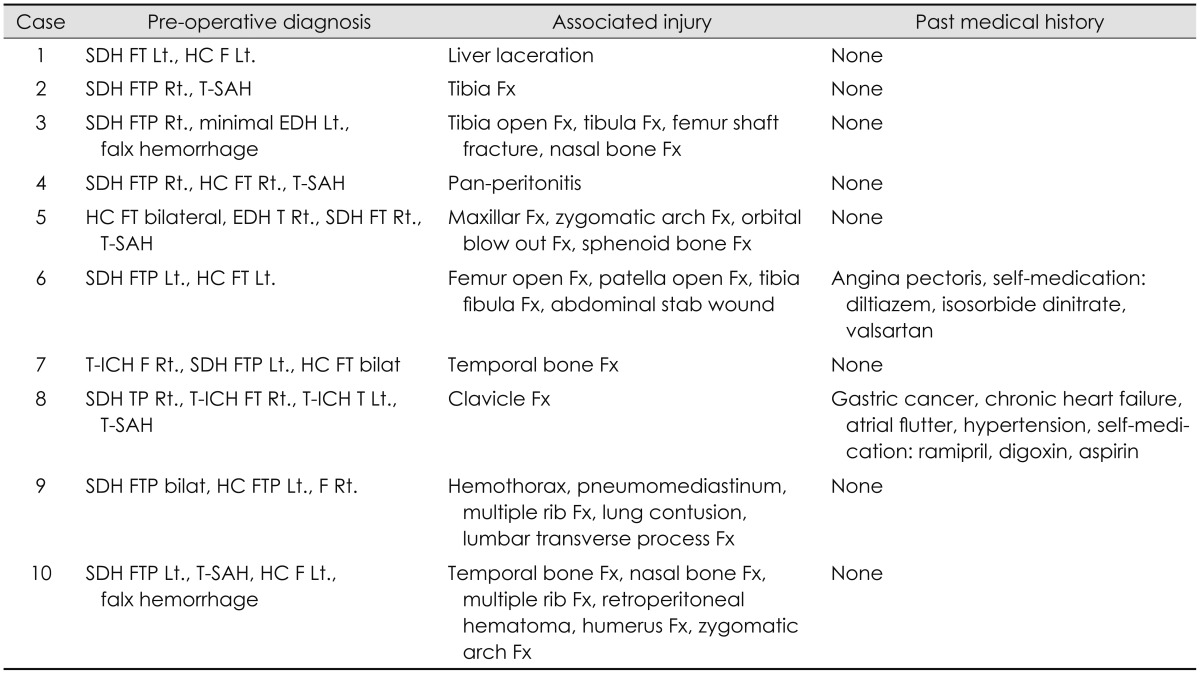
The associated injuries of cases of bilateral decompressive surgery are described in
Table 1 and
3. Multiple associated injuries with at least 4 fractures were characteristic of all the patients who died (except case 3). The patients died after organ donation.
TABLE 3
Associated injury and past medical history of bilateral decompressive surgery cases
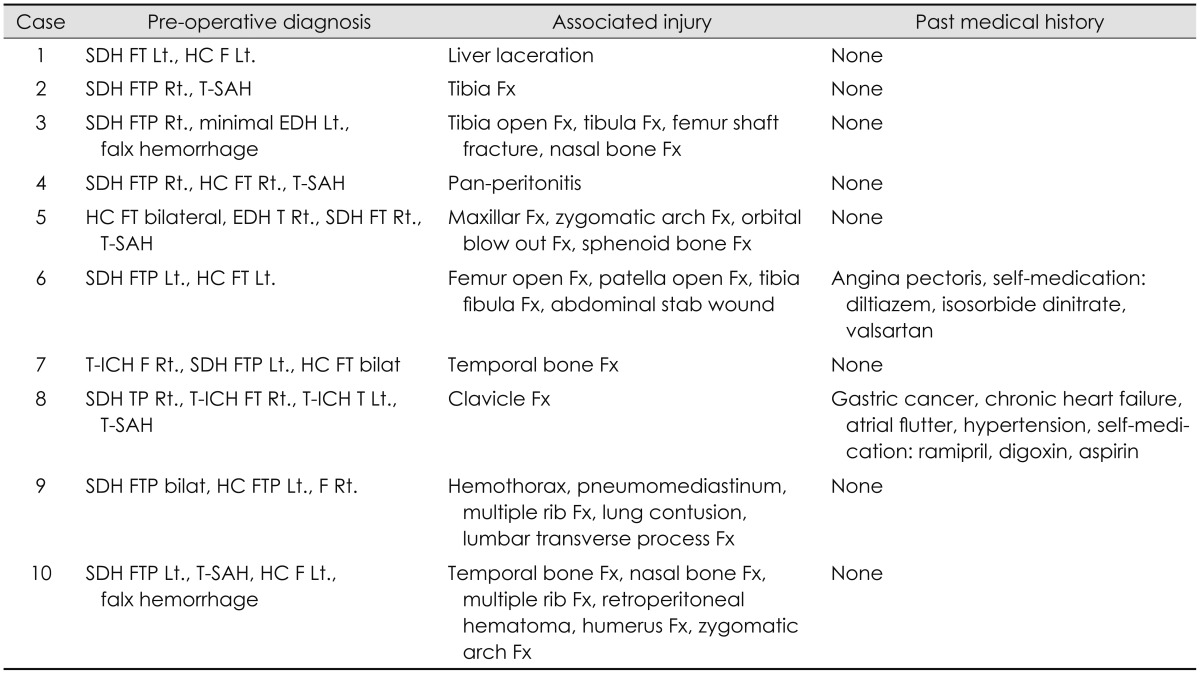

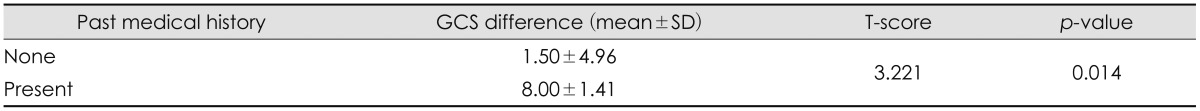
Cases 6 and 9 showed an acute aggravation of the GCS score, which decreased by over seven points after surgery compared to the admission score. These patients on medication for heart disease, which increased their bleeding tendency. The past medical history and medications are described in
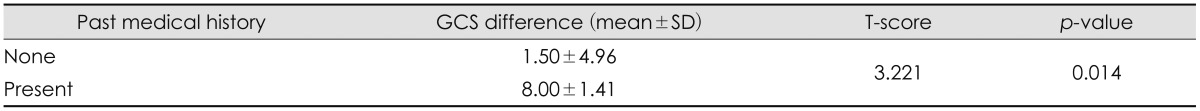
Table 3. Statistical analysis showed significant differences between pre-operative GCS and discharge GCS from patients with past medical history and patient don't have past medical history (
Table 4).
TABLE 4
Comparison of difference between pre-operative GCS and discharge GCS from patients with past medical history and patient don't have past medical history

Preoperative diagnoses of intracranial hematoma are described in
Table 3. In case 3, Amount of EDH was increased after first craniectomy so that case requiring a second operation for increasing EDH. In another cases we cannot find out relationship between preoperative diagnoses of intracranial hematoma and kinds of immediate contralateral intracranial hematoma that requiring second surgery.
We review preoperative lab finding which include platelet count, prothrombin time (PT), activated partial thromboplastin time (aPTT) and international normalized ratio (INR). Each patient had more than 100,000 platelets and all patients had a normal PT, aPTT and INR.
Go to :

Discussion
Contralateral acute intracranial hematoma after decompressive surgery following acute SDH is rare but potentially lethal.
8)
The overall prognoses of bilateral craniectomy cases are bad. Methods to predict the prognosis have not yet been investigated. In order to predict the prognosis of immediate contralateral hematoma cases, considering the mechanism of brain injury is important. In this study, all the patients who suffered trauma due to pedestrian traffic accidents died. This result probably relate to a severe brain injury such as diffusion axonal injury that could not be visualized on a CT scan.
4) Diffuse axonal injury in deep structures is known to show poor outcomes.
13)
The exact mechanism of contralateral postoperative EDH formation is debatable.
3) The most accepted hypothesis is that initial decompression surgery for contrecoup injury has a compression effect on the contralateral hematoma.
11) The reduced ICP and tamponade effect contribute to the formation of a contralateral hematoma in case of coup injury.
11) A recent study of risk factors for the development of contralateral EDH following decompressive craniectomy shows that age and the number of bone plate fractures are important risk factors.
10) Our results also support that hypothesis. In previous studies, severe brain swelling and a contralateral skull fracture were indicators of high risk of contralateral acute intracranial hematoma.
1289) In this study, similar to the previously reported results, severe brain swelling and a contralateral skull fracture appears as a warning sign of contralateral acute intracranial hematoma.
CT findings such as the Rotterdam CT classification have been used as predictors of outcomes in patients undergoing decompressive craniectomy.
612) However, in this study, the predictive ability of the Rotterdam CT classification is limited and lacks clarity. The mean score of patients undergoing bilateral decompressive craniectomy was 4.3. We believe the uneven distribution of the score reduced the predictive ability.
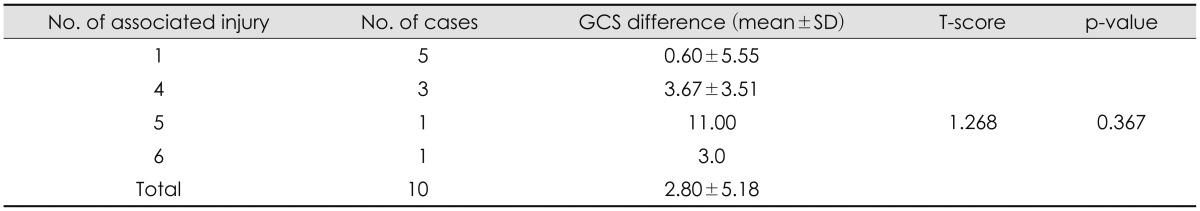
Interestingly, associated injury seems to be an important prognostic factor. All the patients who died (except case 3) had four or more associated injuries. More Severe trauma mechanisms lead to multiple associated injury and severe brain damage. A previous study has shown that severed extremities and external injury are most common in pedestrians among road traffic accidents. Another previous study found that 40% of the pedestrians had three regions injured.
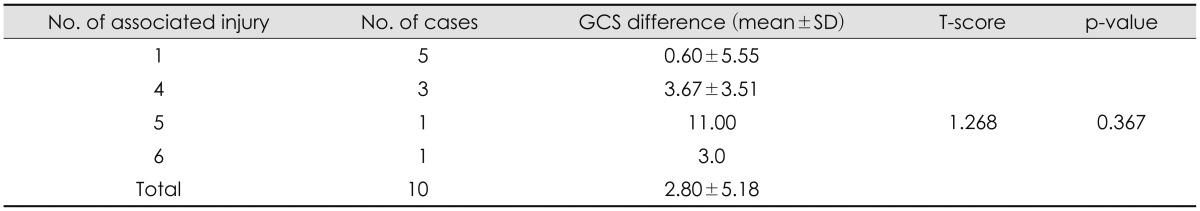
7) However, this study cannot show statistical significance (
Table 5).
TABLE 5
Comparisons of difference between pre-operative GCS and discharge GCS from patients with difference number of associated injury

Another noticeable result from our study is that medical history of the patients seems to be an important prognostic factor. Statistical significant is shown in
Table 4.
It was difficult to find statistical significance in our results given the small sample size. In further study, the more cases are needed to confirm statistical significance. However, while considering the fact that overall incidence is small, this study is of value in understanding clinical features and outcome of bilateral craniectomy.
Go to :

Conclusion
Prognosis of immediate contralateral hematoma is very poor, specially, in cases involving accidents of pedestrian traffic. Severe brain swelling and contralateral skull fractures appear as warning signs of contralateral acute intracranial hematoma. Associated injury and medical history seem to be important prognostic factors.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download