Abstract
Objective
Our study examined the prognostic factors involved in the outcome of patients with chronic subdural hematoma (CSDH) who had undergone burr hole drainage procedures, and investigated the association between outcome and traumatic head injury. In addition, we explored factors related to recurrence.
Methods
This study enrolled 238 patients with CSDH who had undergone burr hole drainage. Patients with history of head injury were categorized into the head trauma group and were compared with the no head trauma group. Outcome was considered good when modified Rankin Scale scores improved from admission to discharge and the final follow-up.
Results
Among 238 patients, 127 (53.4%) were included in the head trauma group. One hundred thirty-three (55.9%) patients demonstrated good outcome at discharge, and 171 (71.8%) patients demonstrated good outcome at the final follow-up. None of the factors examined was significantly correlated with good outcome at discharge. However, only history of head injury (p=0.033, odds ratio 0.511, 95% confidence interval 0.277-0.946) was significantly correlated with poor outcome at long-term follow-up. Recurrence occurred in 20 (8.4%) cases in the total cohort and 11 (55%) patients in the head trauma group.
Conclusion
History of head trauma is correlated with poor outcome at long-term follow-up in CSDH patients having undergone burr hole drainage. Therefore, CSDH patients with history of head injury are susceptible to poor outcome, warranting more careful evaluation and treatment after burr hole drainage.
Go to : 
Chronic subdural hematoma (CSDH) is one of the most common types of intracranial hemorrhage and is a well-known traumatic disease caused by tearing of bridging veins after minor head injury.38) However, some patients develop CSDH from causes other than head injury, such as brain surgery, neovascularization of the hematoma capsule, or coagulation factors.710) In addition, some factors, such as old age, alcoholism, coagulopathy, neurological status at admission, hematoma density, and irrigation, are reported to be correlated with outcome.49121821) However, these results are still controversial, and the association between head trauma and outcome of CSDH has not yet been fully elucidated.
Therefore, the purpose of our study was to examine the prognostic factors for the outcome in patients with CSDH who had undergone burr hole drainage procedures and to determine the association between outcome and traumatic head injury. In addition, we explored factors related to recurrence of CSDH.
Go to : 
Between January 2008 and December 2015, 284 patients with CSDH were admitted and treated in a single tertiary hospital. This study was approved by the institutional review board, and informed consent was waived. Inclusion criteria were as follows: patients must have undergone a burr hole drainage procedure for treatment of symptoms caused by mass effects of CSDH, and the follow-up assessment must have occurred more than 1 month after the initial operation. Eighteen patients with no follow-up history and 28 patients who had not undergone burr hole drainage procedures were excluded. Therefore, 238 total patients were enrolled this study.
Patient information was obtained via retrospective chart review. Factors shown to relate to prognosis and recurrence in previous studies were analyzed, including sex, age, diabetic status, hypertension, end-stage renal disease (ESRD), history of stroke, alcoholism, use of anticoagulant and antiplatelet agents, and previous head injury. Patients on insulin and/or oral hypoglycemic medications were considered to have diabetes. Patients were considered to have hypertension when oral hypertensive medications were prescribed to control blood pressure. ESRD was defined as kidney failure (glomerular filtration rate <15 mL/min/1.73 m2) requiring permanent renal replacement therapy, while stroke was defined as intracranial hemorrhage due to cerebral vascular conditions and/or cerebral infarction. Alcoholism was defined as consumption of more than 14 standard drinks per week or 4 drinks per day, and head trauma was defined as the occurrence of head injury within 3 months prior to hospital admission.
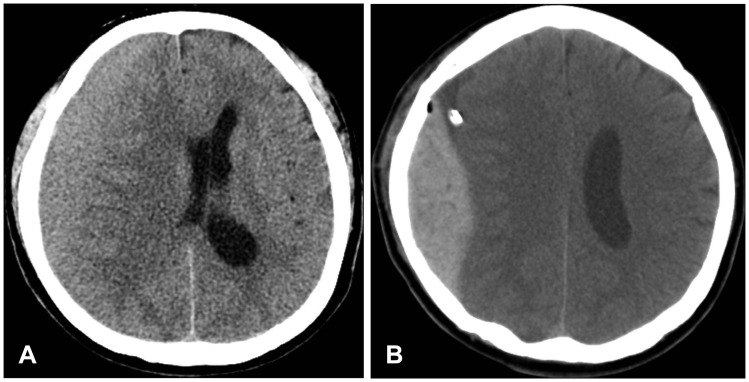
Patients who had complained of symptoms such as headache, general weakness, and/or neurological deficits were diagnosed with CSDH using computerized tomography (CT) scans of the brain. When CSDH was observed on brain CT scan, several parameters were assessed and documented: hematoma thickness, midline shifting based on pineal gland, hematoma density (classified as high, iso, low, or mixed based on brain parenchymal density), and location of hematoma (unilateral versus bilateral).17) In addition, patient status was evaluated and classified according to the modified Rankin Scale (mRS) and Glasgow Coma Scale (GCS). The mass effects of the hematoma were assessed, and procedures were performed under general anesthesia at the discretion of the surgeon as follows: either a single burr hole or two burr holes were trephined, and the site was either irrigated with saline or not irrigated. A silicone tube was inserted into the subdural space to allow for 1 to 3 days of drainage. If sufficient drainage had occurred at the time of the postoperative CT scan and/or the symptoms had improved, the silicone tube was removed.
Brain CT scans were performed at 1 month and 3 months post-operation through our outpatient department. Recurrence was defined as increasing hematoma thickness, based on brain CT scan at discharge, and worsening symptoms. When necessary, patients underwent one additional burr hole drainage procedure. Patient status was again assessed using the mRS at the final follow-up. Good outcome at discharge was indicated when mRS scores improved from admission to discharge. In addition, good outcome at the final follow-up was assessed using the same method.
Statistical analyses were performed using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). Baseline characteristics were assessed and compared between the two groups (no head injury and head injury) using the chi-square test, Fisher’s exact test, linear by linear test, and Student’s t-test. To assess good outcome and recurrence, univariate analysis of clinical, radiological, and neurological findings and operative technique was performed using a chi-square test, Fisher’s exact test, and a Student’s t-test. Variables with a p-value of <0.2 in univariate analysis were then chosen for multivariate analysis using a logistic regression model. The result of head injury was included in multivariate analysis regardless of the result of univariate analysis, as this was the variable of interest in this study. In all analyses, p-value of less than 0.05 were defined as statistically significant.
Go to : 
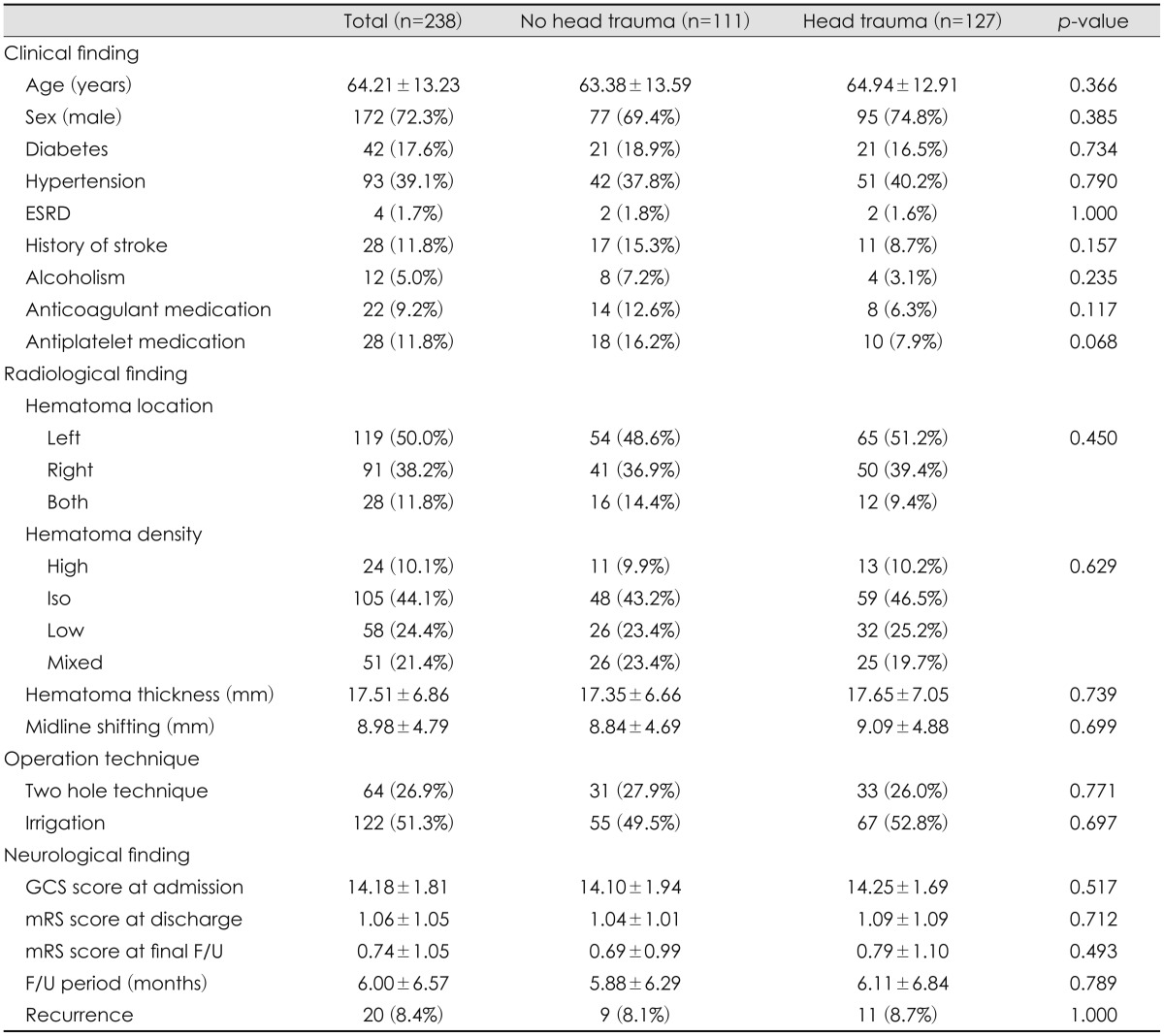
Among the 238 patients who had undergone burr hole drainage procedures, 127 (53.4%) patients were included in the head trauma group and compared with the no head trauma group. With regard to baseline characteristics, no factor was significantly different between the two groups (Table 1).
At admission, 114 (47.8%) patients had headache, 4 (1.7%) patients had dizziness, 9 (3.8%) patients had dysarthria or aphasia, 2 (0.8%) patients had numbness, 12 (5.0%) patients had gait disturbance or weakness in both legs, 27 (11.3%) patients had decreasing mentality, 68 (28.6%) patients had hemiparesis, and 2 (0.8%) patients had seizure. After the burr hole drainage procedure, mRS score improved from 1.93±1.27 at admission to 1.06±1.05 at discharge and 0.74±1.05 at the final follow-up.
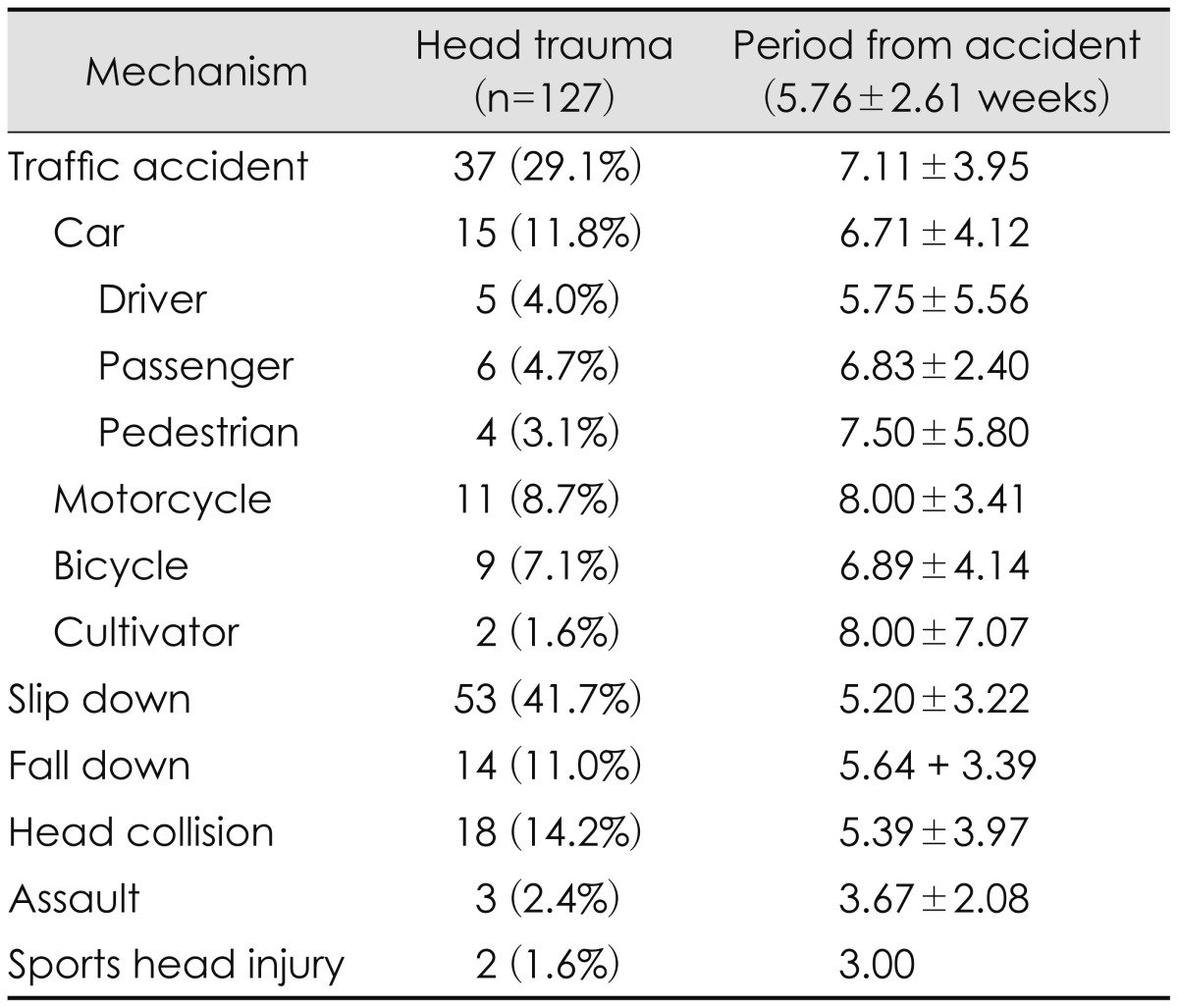
Mechanisms of head trauma included traffic accident total 37 (29.1%), car 15 (11.8%), motorcycle 11 (8.7%), bicycle 9 (7.1%), cultivator 2 (1.6%), slip down 53 (41.7%), fall down 14 (11.0%), head collision 18 (14.2%), assault 3 (2.4%), and sports head injury 2 (1.6%). In addition, the mean period from accident was 5.76±2.61 weeks. The longest period was traffic accident (7.11±3.95 weeks), and the shortest period was sports head injury (3.00 weeks) (Table 2).
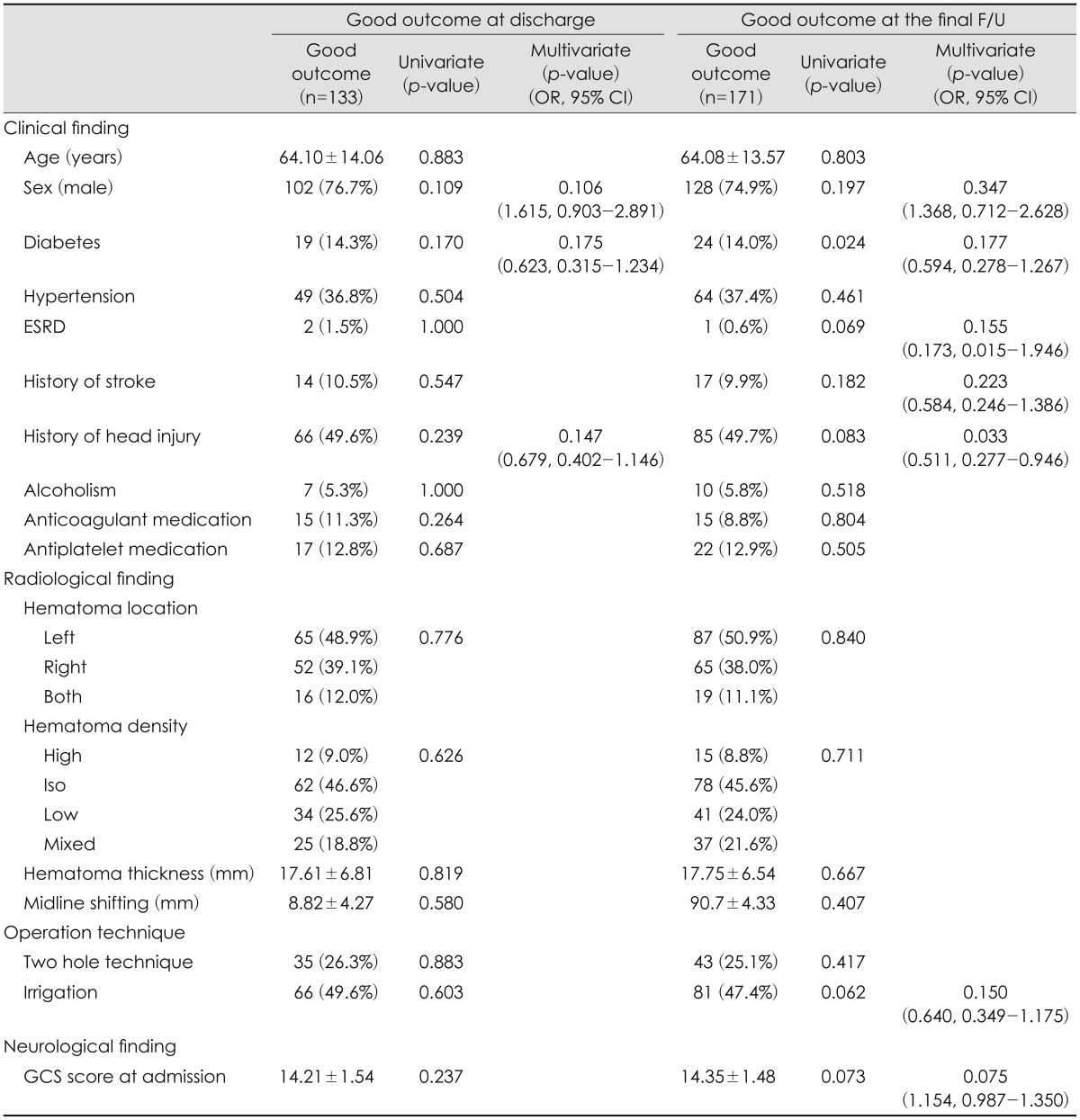
One hundred thirty-three (55.9%) patients showed good outcome at discharge, and 171 (71.8%) patients showed good outcome at the final follow-up. None of the factors was significantly correlated with outcome at discharge. However, some factors correlated with outcome at the final follow-up. Diabetes (p=0.024) was statistically significant in univariate analysis, but in multivariate analysis, only history of head injury (p=0.033, odds ratio [OR] 0.511, 95% confidence interval [CI] 0.277-0.946) was significantly correlated with outcome (Table 3).
Three patients (1.3%) expired after burr hole drainage procedure, one had pneumonia associated with decreasing mentality, one had peritonitis with unknown origin, and one had sudden cardiac arrest. Additional complications included post-operative infection in one patient and epidural hematoma related to burr hole drainage in another (Figure 1).
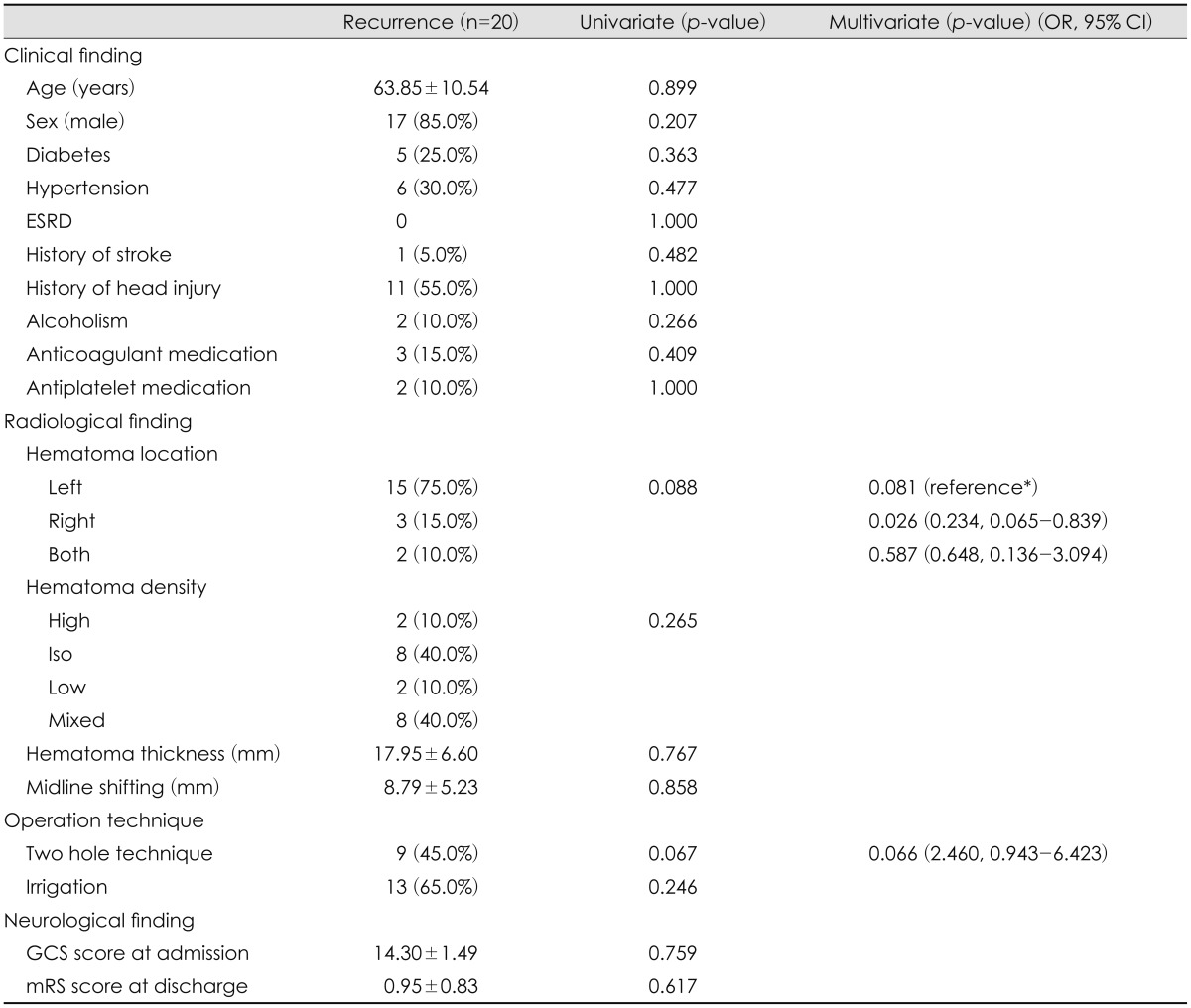
Recurrence occurred in 20 (8.4%) cases in the total group: 9 (45%) patients in the no head injury group and 11 (55%) patients in the head injury group, and there was no significant difference between them. Although there were no significant factors in the univariate analysis, in multivariate analysis of recurrence, right side hematoma (p=0.026, OR 0.234, 95% CI 0.065-0.839) alone was statistically significant (Table 4).
Go to : 
Some recent studies have reported on the diagnosis of minor head injury, but currently, no established optimal guidelines exist. Previously, in cases of minor head injury, the status of the damaged brain was evaluated solely using brain CT, but more recently, magnetic resonance imaging (MRI) and/or diffuse tensor imaging (DTI) techniques for the evaluation of white matter damage and/or axonal injury have been studied.21516) In our study, because the standard protocol for evaluating CSDH and minor head trauma used only brain CT, it is possible that this procedure was not sensitive enough to determine the true extent of damage. For this reason, although history of head trauma was not correlated with outcome at discharge, it may be correlated with poor outcome at the final follow-up. Recently, some reports have supported the use of MRI and/or DTI for evaluation of minor head trauma.1319) As such, patients with CSDH should be considered candidates for these evaluation methods.
Many studies report that GCS score at admission is strongly correlated with outcome. In a study by Amirjamshidi et al.1), lower initial GCS and higher Glasgow Outcome Scale scores upon discharge were associated with negative outcomes. In our study, GCS score at admission was 14.18±1.81 in the total cohort, and scores of the head trauma group (14.25±1.69) and the no head trauma group (14.10±1.94) were not significantly different. In addition, GCS score at admission was not correlated with good outcome at discharge or good outcome at the final follow-up. Because good outcome was defined as improvement of mRS score from admission to discharge or the final follow-up. If not the initial state is corrected, it is considered that the initial state will have a too significant impact on the result.
Old age has also been considered a strong risk factor for CSDH outcome due to age-related brain atrophy. Fukuhara et al.5) reported that brain surface elasticity is an important factor in CSDH. Ro et al.14) reported correlation of old age and poor outcome due to brain expansion. In our study, age was not significantly correlated with outcome at discharge and the final follow-up. However, there were three mortality cases (1.3%), and these patients were elderly (more than 70 years old). Although we observed no association with burr hole drainage procedure directly, conditions associated with aging may contribute to poor outcome.
Investigation of factors relating to recurrence of CSDH revealed that only location of the hematoma in the right hemisphere significant correlated with low recurrence. Although it was not statistically significant, location of the hematoma in the left hemisphere was also more strongly correlated with low recurrence than bilateral location of the hematoma. To confirm these results, subgroups divided by hematoma location were analyzed. Among 210 patients (right/left: 119/91) with unilateral hematoma, 115 patients (54.8%, left/right: 61 [51.3%]/54 [59.3%]) received irrigation during the operation, and among 28 patients with bilateral hematoma, 7 patients (25.0%) received irrigation. Irrigation (p=0.006) was a significant factor in linear by linear analysis. Although irrigation was not correlated with outcome in multivariate analysis in our study, irrigation may have some effects on recurrence. Many studies have shown correlation between recurrence of CSDH and irrigation.61120) To determine the important effects of irrigation on recurrence, well-designed and larger prospective studies are necessary.
There are several limitations in our study. First, this study is limited by its retrospective nature. Therefore, it may be subject to selective bias and compounding effects. To prevent these problems, the outcome was defined in such a way as to exclude the initial state. Second, to evaluate brain damage after minor head trauma, MRI and DTI were not performed. To determine whether other lesions affected outcome, a prospective study using MRI and/or DTI would be necessary. Third, mechanisms of head trauma and time periods following accidents were studied, and we found that larger vector mechanisms, such as traffic accidents, were associated with longer periods of time before CSDH occurrence. Thus, we predict that mechanisms with larger vectors should be observed for longer periods than minor vector mechanisms. Because this was outside the scope of our study, further investigation is needed.
Go to : 
In conclusion, history of head trauma is correlated with poor outcome at long-term follow-up in CSDH patients following burr hole drainage. Therefore, CSDH patients with history of head injury are susceptible to poor outcome, warranting more careful evaluation and treatment after burr hole drainage. In addition, further study is needed to investigate the correlation between irrigation and recurrence of CSDH following burr hole drainage.
Go to : 
References
1. Amirjamshidi A, Abouzari M, Eftekhar B, Rashidi A, Rezaii J, Esfandiari K, et al. Outcomes and recurrence rates in chronic subdural haematoma. Br J Neurosurg. 2007; 21:272–275. PMID: 17612917.

2. Bigler ED. Neuropathology of mild traumatic brain injury: correlation to neurocognitive and neurobehavioral findings. In : Kobeissy FH, editor. Brain neurotrauma: molecular, neuropsychological, and rehabilitation aspects. Boca Raton, FL: CRC Press/Taylor & Francis;2015. p. 433–450.
3. De Bonis P, Trevisi G, de Waure C, Sferrazza A, Volpe M, Pompucci A, et al. Antiplatelet/anticoagulant agents and chronic subdural hematoma in the elderly. PLoS One. 2013; 8:e68732. PMID: 23874740.

4. Delgado PD, Cogolludo FJ, Mateo O, Cancela P, Garcia R, Carrillo R. Early prognosis in chronic subdural hematomas. Multivariate analysis of 137 cases. Rev Neurol. 2000; 30:811–817. PMID: 10870192.
5. Fukuhara T, Gotoh M, Asari S, Ohmoto T, Akioka T. The relationship between brain surface elastance and brain reexpansion after evacuation of chronic subdural hematoma. Surg Neurol. 1996; 45:570–574. PMID: 8638244.

6. Ishibashi A, Yokokura Y, Adachi H. A comparative study of treatments for chronic subdural hematoma: burr hole drainage versus burr hole drainage with irrigation. Kurume Med J. 2011; 58:35–39. PMID: 22027196.

7. Kageyama H, Toyooka T, Tsuzuki N, Oka K. Nonsurgical treatment of chronic subdural hematoma with tranexamic acid. J Neurosurg. 2013; 119:332–337. PMID: 23641825.

8. Kolias AG, Chari A, Santarius T, Hutchinson PJ. Chronic subdural haematoma: modern management and emerging therapies. Nat Rev Neurol. 2014; 10:570–578. PMID: 25224156.

9. Lee JJ, Won Y, Yang T, Kim S, Choi CS, Yang J. Risk factors of chronic subdural hematoma progression after conservative management of cases with initially acute subdural hematoma. Korean J Neurotrauma. 2015; 11:52–57. PMID: 27169065.

10. Lee KS. Chronic subdural hematoma in the aged, trauma or degeneration? J Korean Neurosurg Soc. 2016; 59:1–5. PMID: 26885279.

11. Liu W, Bakker NA, Groen RJ. Chronic subdural hematoma: a systematic review and meta-analysis of surgical procedures. J Neurosurg. 2014; 121:665–673. PMID: 24995782.

12. Miranda LB, Braxton E, Hobbs J, Quigley MR. Chronic subdural hematoma in the elderly: not a benign disease. J Neurosurg. 2011; 114:72–76. PMID: 20868215.

13. Mu W, Catenaccio E, Lipton ML. Neuroimaging in blast-related mild traumatic brain injury. J Head Trauma Rehabil. DOI: 10.1097/htr.0000000000000213. [epub ahead of print March 28, 2016].

14. Ro HW, Park SK, Jang DK, Yoon WS, Jang KS, Han YM. Preoperative predictive factors for surgical and functional outcomes in chronic subdural hematoma. Acta Neurochir (Wien). 2016; 158:135–139. PMID: 26602235.

15. Talavage TM, Nauman EA, Leverenz LJ. The role of medical imaging in the recharacterization of mild traumatic brain injury using youth sports as a laboratory. Front Neurol. 2015; 6:273. PMID: 26834695.

16. Toth A. Magnetic resonance imaging application in the area of mild and acute traumatic brain injury: implications for diagnostic markers?. In : Kobeissy FH, editor. Brain neurotrauma: molecular, neuropsychological, and rehabilitation aspects. Boca Raton, FL: CRC Press/Taylor & Francis;2015. p. 329–340.
17. van Havenbergh T, van Calenbergh F, Goffin J, Plets C. Outcome of chronic subdural haematoma: analysis of prognostic factors. Br J Neurosurg. 1996; 10:35–39. PMID: 8672256.
18. Villagrasa J, Prat R, Díaz JF, Comuñas F. Analysis of prognostic factors in adults with chronic subdural hematoma. Neurologia. 1998; 13:120–124. PMID: 9608218.
19. Wylie GR, Freeman K, Thomas A, Shpaner M, M OK, Watts R, et al. Cognitive improvement after mild traumatic brain injury measured with functional neuroimaging during the acute period. PLoS One. 2015; 10:e0126110. PMID: 25962067.

20. Xu C, Chen S, Yuan L, Jing Y. Burr-hole irrigation with closed-system drainage for the treatment of chronic subdural hematoma: a meta-analysis. Neurol Med Chir (Tokyo). 2016; 56:62–68. PMID: 26377830.

21. Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S. Independent predictors of recurrence of chronic subdural hematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg. 2003; 98:1217–1221. PMID: 12816267.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download