Case Report
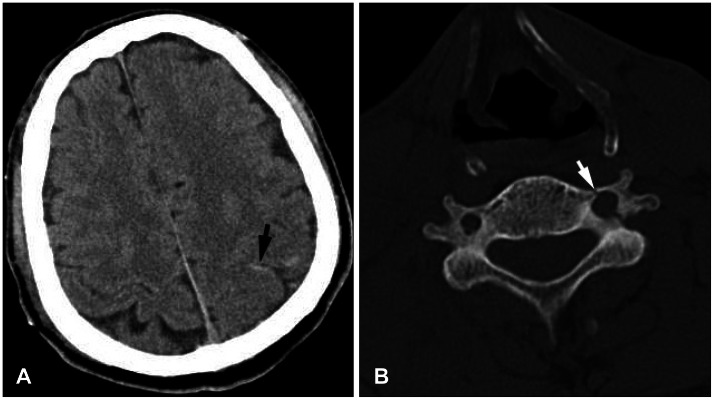
A 73-year-old man was referred from a local hospital with impaired consciousness and left hemiparesis after a motor car accident. He was diagnosed with traumatic subarachnoid hemorrhage on the left parietal lobe and left lateral mass fractures on C2, C5, and C6, involving the transverse foramen (
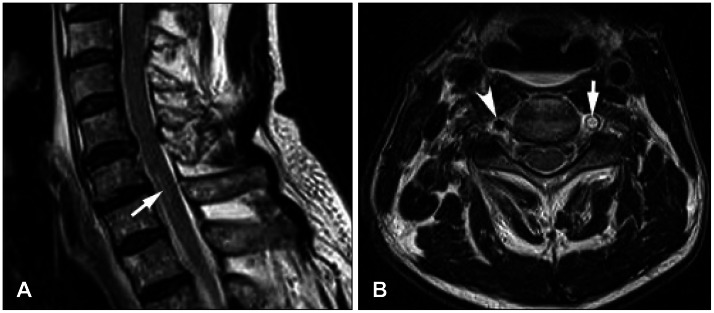
Figure 1). A neurological examination revealed stupor with a Glasgow Coma Scale score of 8. Severe grade 2 hemiparesis of the left arm and leg was detected. High signal was seen at the C6-7 levels of the spinal cord on a sagittal cervical spine magnetic resonance imaging (MRI). The signal void on the left vertebral artery was lost on the C6 axial image (
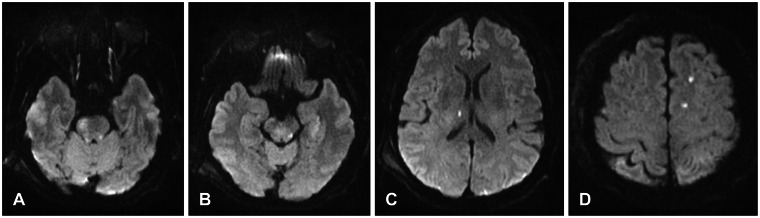
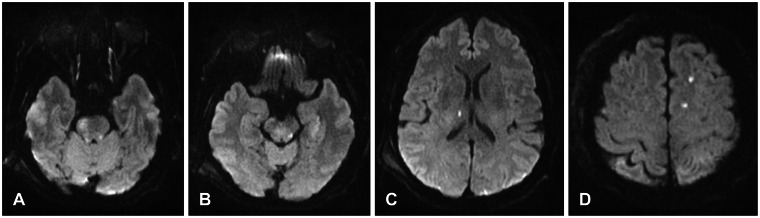
Figure 2). He was diagnosed with left VAD and was managed conservatively. Neck computed tomography (CT) angiography showed obliteration of the left second segment of the vertebral artery (V2) (
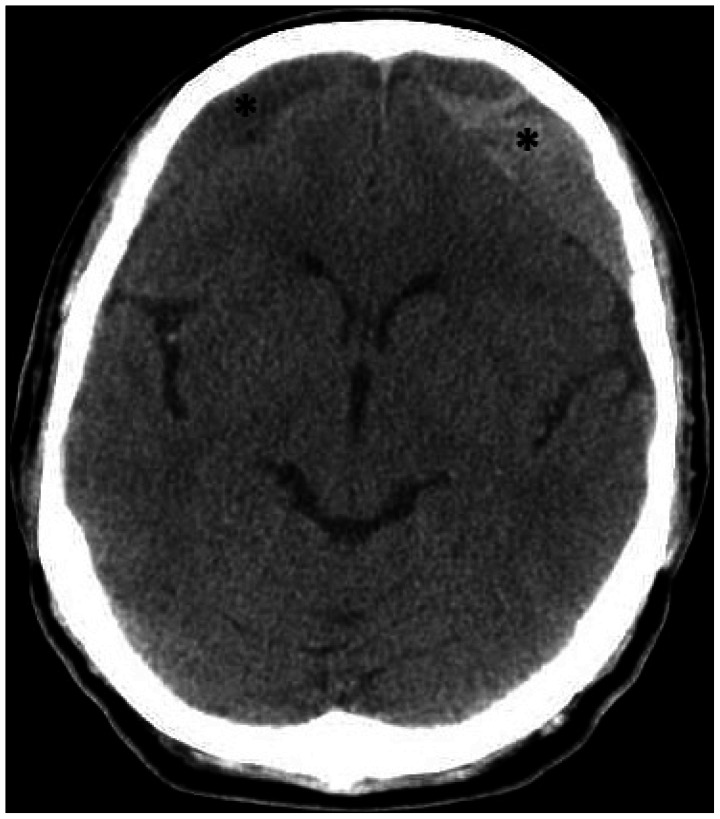
Figure 3). The obliteration of the V2 segment remained on 2-week follow-up CT angiography. A brain MRI was performed to evaluate the cause for impaired consciousness and motor weakness. Diffusion weighted images revealed multiple area of abnormally high signals in the right side of the pons, left side of the midbrain, right thalamus, corpus callosum splenium, both parietal lobes, and the left frontal lobe, indicating multiple acute cerebral infarctions (
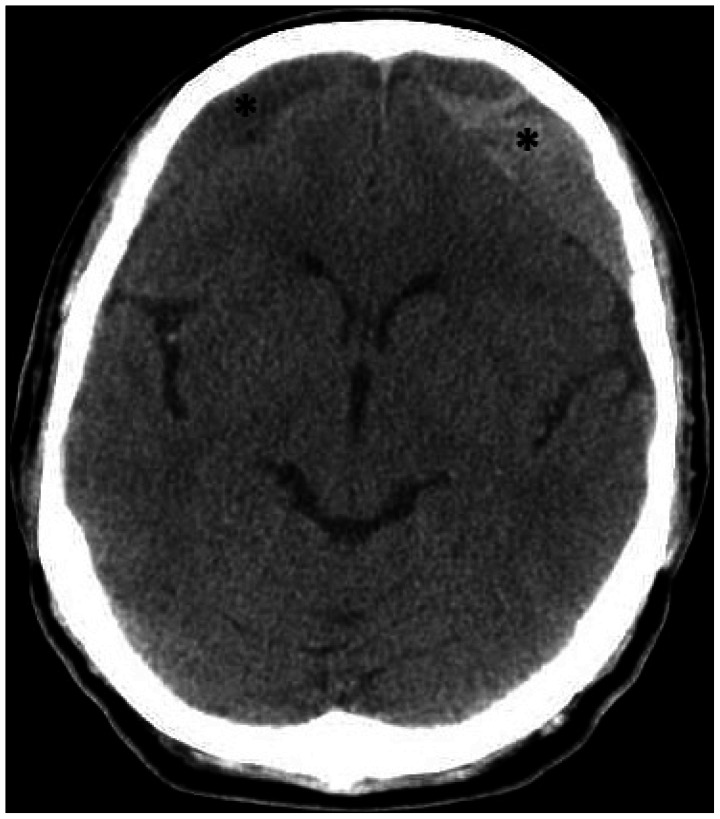
Figure 4). Ischemic areas were diffusely distributed to the anterior and posterior circulation of the Circle of Willis. Ischemic stroke occurred immediately after cervical spine trauma and neurological deficits after trauma resulted from brain ischemia. Aspirin was started for antiplatelet therapy 1 week after the trauma after confirming disappearance of the acute traumatic hemorrhage. He was discharged from the hospital on aspirin to receive neurological follow-up and rehabilitation therapy. A brain CT scan at discharge showed subdural fluid collection in both frontal lobes. His motor weakness and consciousness state were improving gradually to a grade 4 weakness and alert state on follow-up examination. Bilateral chronic subdural hematomas (CSDHs) were observed with headache 4 months after the trauma (
Figure 5). Burr hole trephinations were performed on both sides for the CSDHs.
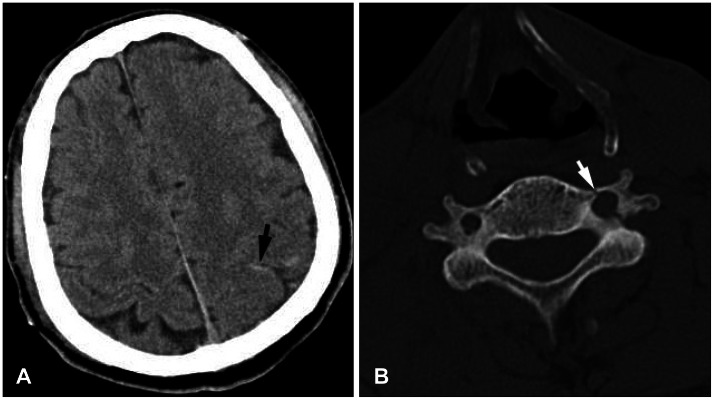 | FIGURE 1A: Brain computed tomography (CT) scan showing traumatic subarachnoid hemorrhage (arrow) on the left parietal lobe after trauma. B: Cervical CT scan demonstrating fracture of the left transverse process of C6 (arrow) with encroachment on the neural foramen.
|
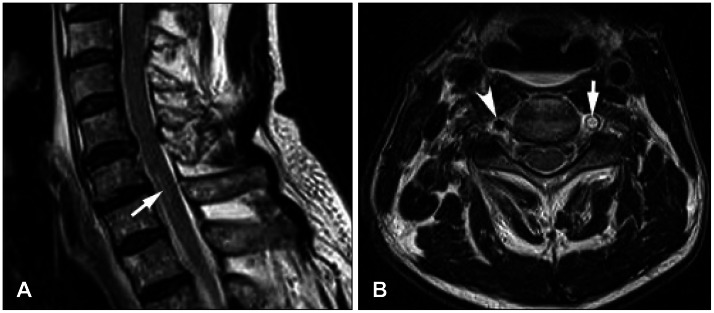 | FIGURE 2Cervical spine magnetic resonance imaging. A: Sagittal T2 weighted image showing a high signal (arrow) on the C6-7 cord on a sagittal image. B: Loss of the signal void was detected on the left vertebral artery (arrow) on the C6 axial T2 weighted image. See the normal signal void of the right vertebral artery (arrowhead).
|
 | FIGURE 3Neck computed tomography angiography showing obliteration of the V2 segment on the left vertebral artery (arrow).
|
 | FIGURE 4Brain magnetic resonance imaging showing multiple high signals on diffusion weighted images of the pons (A), midbrain (B), thalamus (C), and frontal lobe (D).
|
 | FIGURE 5Brain computed tomography scan showing chronic subdural hematomas on both frontal lobes (*) 4 months after the trauma.
|
Go to :

Discussion
The incidence of vertebral artery injury after blunt trauma of the cervical spine is unknown, as it is rarely symptomatic and therefore easily overlooked.
3) Vertebral artery injury may be more prevalent than commonly believed after cervical spine fracture. Traumatic VAD following severe neck trauma was first reported in 1955, and most cases result from chiropractic maneuvers of the neck or traffic accidents.
5) The possibility of vertebral artery injury should be considered when establishing the clinical management scheme for blunt trauma of the cervical spine.
10)
Although the mechanisms are not absolutely clear, there seems to be an important relationship between arterial dissection and cervical trauma. Giacobetti et al.
1) reported that flexion distraction-type injuries are the most common mechanism of non-penetrating vertebral artery injuries, followed by a flexion compression mechanism. Because of their unique course through four or five transverse foramen, the vertebral arteries are particularly prone to direct traumatic damage.
5) Fractures involving the lateral masses, particularly fractures of the transverse foramen, may damage the artery within its bony confines. The initial injury to the artery most likely involves intimal disruption through excessive distraction and stretching of the artery between two adjacent transverse foramens.
10) Unilateral occlusion of the vertebral artery seldom results in symptomatic ischemic stroke. Our case with normal contralateral vertebral artery rarely developed neurological deficits due to embolic infarction, considering thrombosis had not extended distally to the basilar trunk. A delay in clinical presentation has been attributed to propagation of distal extension of the dissection, mural thrombus into the basilar system, and embolization to the brain.
11) Blunt trauma on the vertebral artery can result in occlusion, which is not necessarily confined to the level of the bony injury. The site of dissection can serve as a site of progressive thrombosis or artery-to-artery emboli, the latter causing occlusion of the distal branch artery.
68)
Clinical symptoms of VAD after neck trauma consist of neck and/or head pain, often localized to the site of intimal disruption, which are common warning symptoms of dissection. Symptoms are often only minor and there may be no neurologic deficits. However, patients who develop vertebrobasilar ischemia often die or are severely impaired.
5) Vertebrobasilar ischemia after cervical spine injury was first described in 1955.
7) In this report, the posterior inferior cerebellar artery (PICA) syndrome developed several days after a C5 fracture. Unilateral VAD with subsequent thrombosis may not lead to clinical symptoms due to adequate blood supply through PICA from the contralateral side and/or reconstitution through the intramuscular collateral vessels of the thyrocervical trunk.
4) Willis et al.
10) reported on a prospective clinical study in which none of 26 patients with a vertebral artery injury clearly developed neurological dysfunction or other sequelae. Our patient is rare, as he presented with ischemic brain stroke at anterior and posterior circulation of the Circle of Willis. Cerebral infarction sequelae remained, such as limb weakness resulting from the pons infarction. Parent et al.
4) reported a retrospective review of 640 patients with cervical spine fractures in which five patients had a lateral dislocation of the cervical spine and injuries to the vertebral arteries. Three of these patients developed symptoms of vertebrobasilar ischemia, which led to a VAD diagnosis based on angiographic or postmortem findings. Conventional angiography remains the gold standard but Doppler ultrasound, duplex sonography, MRI, and MR angiography demonstrate vessel stenosis or occlusion, and a hematoma may be seen in the vessel wall.
2) It is important to detect VAD before ischemic sequelae occur. Recent progress in neuroradiology and neurosonography allows a noninvasive approach to diagnose VAD.
Treatment for traumatic VAD is controversial. No guidelines have been established for the timing or means of anticoagulation or interventional therapy. However, the therapeutic goal for acute stage VAD remains preventing ischemic stroke. Antiplatelet or anticoagulation therapy is generally recommended for intimal disruption.
9) However, anticoagulation in a patient with trauma causes a significant hemorrhagic risk. Interventional therapy is an alternative in patients with severe vertebral artery injuries or symptoms of a vertebrobasilar embolism.
12)
The prognosis for VAD is highly variable, but usually remains good, depending on the extent of the damage and the presence of adequate collateral circulation. VAD does not usually cause a critical manifestation. The rate of VAD-associated ischemia in patients with cervical spine trauma is low because the opposite vertebral artery fills the intracranial portion of the occluded vessel. However, if collateral blood flow is inadequate, an occlusion may present severe vertebrobasilar stroke. In addition, a thrombus in an occluded segment of the vertebral artery can create an embolic shower, as shown here. Early recognition of VAD following cervical injury and considering the natural history of VAD may lead to proper treatment and improve survival.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download