ROP is frequently associated with RA.
38121314) In RA, the pannus formation is attributed to inflammation of the synovial membrane, resulting in overgrowth of the hyaline cartilage and peri-articular inflammation.
4) Consequentially, inflammation, ligament laxity, and bone erosion result in C1-2 joint laxity and subluxation. Although uncommon, a ROP can be developed due to AAS in patients without RA.
13) AAS exerts mechanical stress and injury on the transverse ligament of the atlas, resulting in a reactive hypertrophied mass. Therefore, AAS may play an important role in the development of ROP.
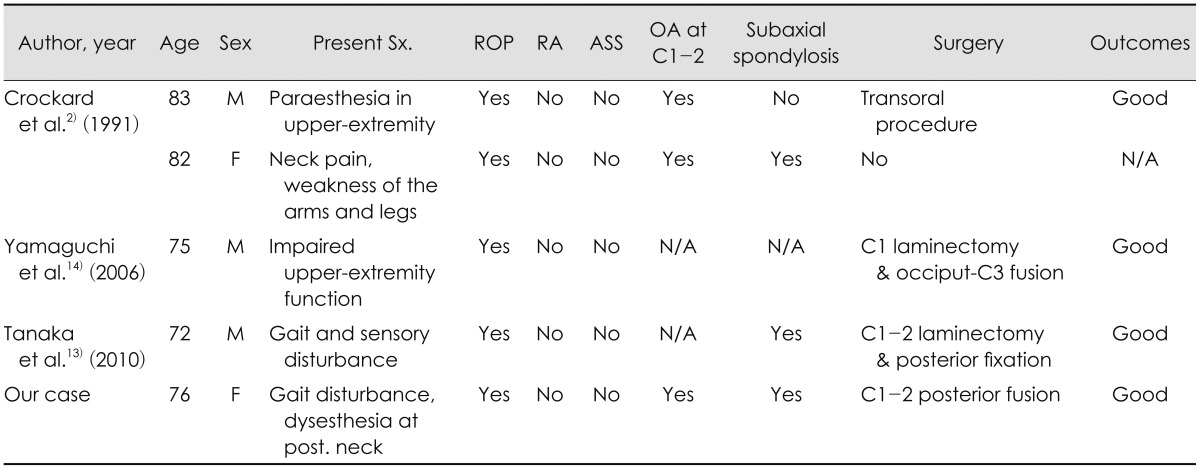
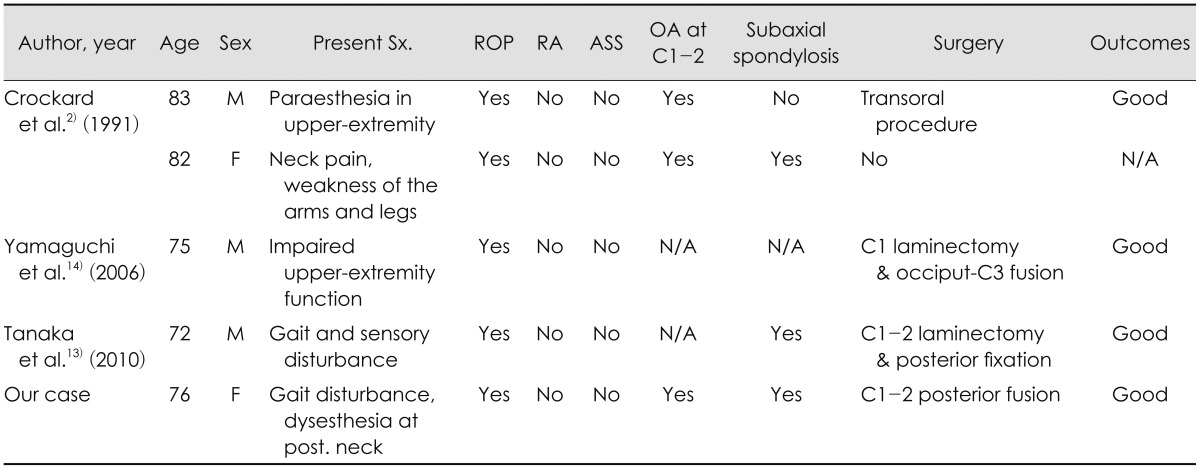
61012) However, like our case, a ROP unassociated with both AAS and RA is extremely rare. Only four cases of ROP unassociated with both AAS and RA have been previously reported (
Table 1).
271314) The exact mechanism of pannus formation is unclear. However, the previous reports suggested that loss of mobility at middle and lower cervical segment, and resultant excessive motion of the C1-2 segment transfer the mechanical stress to the atlantoaxial joint, resulting in pannus formation.
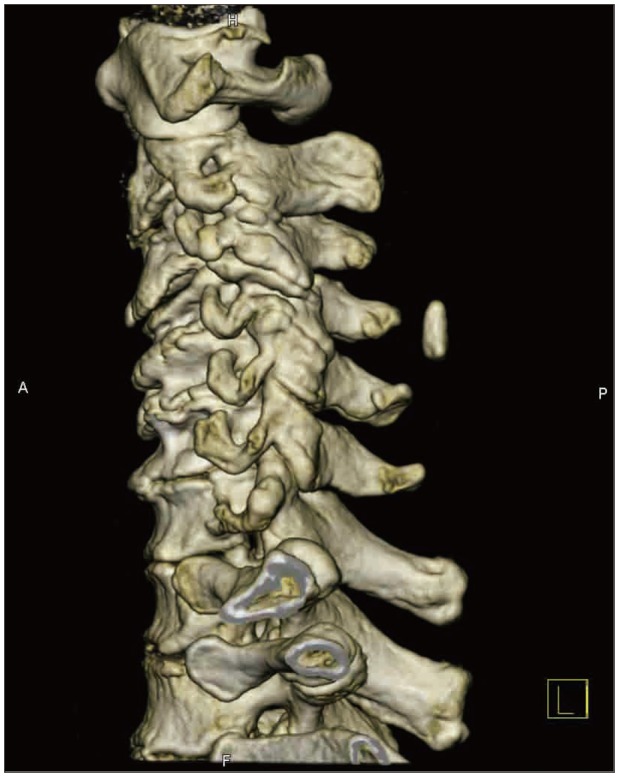
1315) In the case, mobility below the C2 cervical spine was limited by spondylosis and facet fusion at C2-3-4 levels. In our case, severe multiple spondylotic change of subaxial cervical spines were also found. However, in the other reports, a ROP developed in patients with mild spondylosis or without spondylosis in subaxial cervical spine.
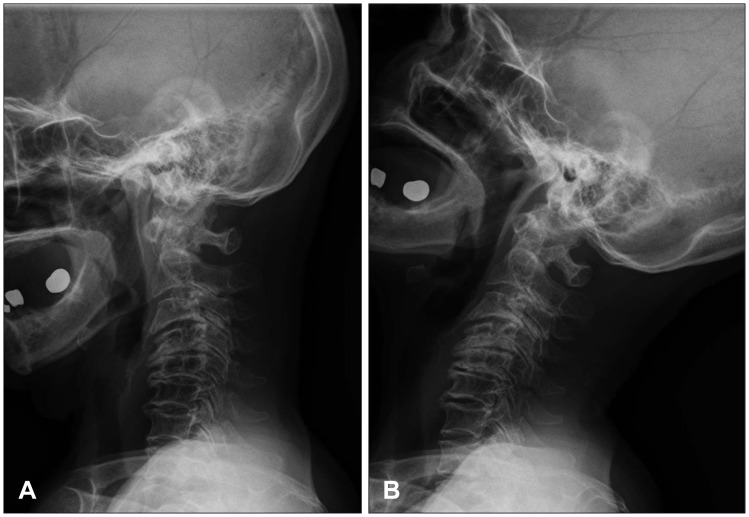
61011) Therefore, only loss of mobility associated with subaxial cervical spondylosis is difficult to completely explain the mechanism of ROP formation in patients without AAS. Reviewing the reported cases and our case, we found two common points in the patients. All patients were more than 70 years old and most had moderate or severe osteoarthritic change at atlantoaxial joint. Thus, we speculated that moderate or severe osteoarthritis of C1-2 itself causes a partial tear or degradation of the transverse ligament. Resultant vicious cycle of repair and injury may lead to progressive ROP. However, unlike RA, the ROP in the elderly may be not associated with overt AAS. Instead, we suggest that stiffness due to severe osteoarthritis of lateral atlantoaxial joints may prevent the overt AAS, offsetting the effect of loose transverse ligament. Nevertheless, we still believe that C1-2 instability play a key role in development or progression of ROP because most of ROP associated with AAS and often resolve spontaneously after C1-2 fusion.
5678121314) In the elderly with osteoarthritis, even though C1-2 instability is not "overt AAS" on the radiographs, "micro-instability" may be exist and affect the progression of ROP.
TABLE 1
Clinical and radiologic features of retro-odontoid pseudotumors without rheumatoid arthritis and atlantoaxial subluxation

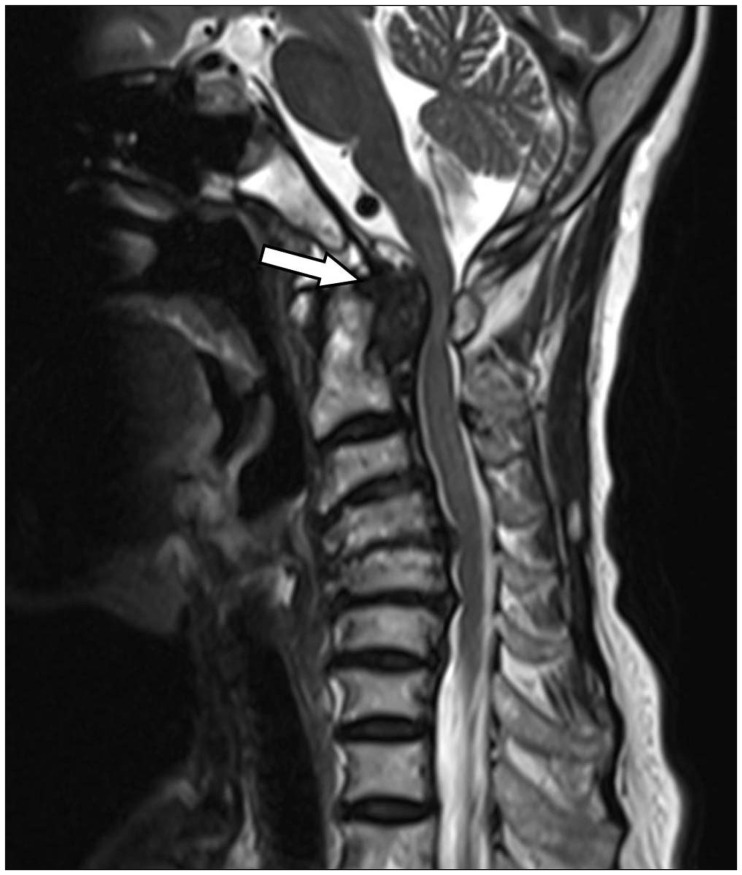
Surgical treatment of ROP can be classified into two modalities: 1) direct excision of the mass and 2) posterior decompression and fusion aiming spontaneous tumor regression.
114) Direct excision of the mass can be performed by the transoral approach and epidural or transdural approach by posterior laminectomy.
1911) However, The transoral approach is vulnerable to cerebrospinal fluid leakage, postoperative infection and postoperative instability.
911) The epidural approach may force retraction of the nerve root and spinal cord and have hemorrhagic risk.
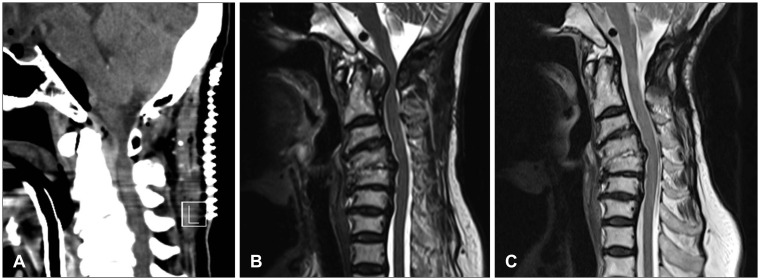
11) A posterior transdural approach may decrease the distance needed to reach the ROP and does not require retraction of the spinal cord and nerve root. However, if the mass located in the midline of cervical axis or presented with huge size, the posterior transdural approach is limited used for radical resection due to risk of injuries. In our case, differential diagnosis of tumorous lesion or disc herniation should be necessary due to absence of AAS and RA.
613) Therefore, in the first operation, we performed direct mass debulking and biopsy by transdural approach with minimal hemilaminectomy. However, the direct mass excision and hemilaminectomy can unexpectedly new-onset AAS associated with additional ligament injury, resulting in re-growth of ROP and neurological aggravation. Recently, posterior decompression and fusion may be considered as first choice of treatment for ROP with AAS.
68121314) In our case, C1 lateral mass-C2 pedicle screw fixation without further laminectomy or mass removal was performed and the ROP regressed completely. Goel and Dange
4) reported the immediate postoperative regression of ROP after lateral mass reconstruction in the patient with RA.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download