Abstract
Objective
Vertebroplasty is an effective treatment for vertebral compression fracture, but may progress gradual vertebral height decrease in spite of vertebroplasty. Gradual vertebral height decrease also may induce aggravation of kyphotic change without severe pain. The purpose of this study was to evaluate risk factors for gradual vertebral height decrease in the absence of recurrent severe back pain.
Methods
A retrospective analysis was performed on 44 patients who were diagnosed with a first osteoporotic compression fracture at a single level at the thoracolumbar junction. All patients were taken vertebroplasty. Possible risk factors for gradual vertebral height decrease, such as sex, age, bone mineral density, body mass index, level of compression fracture, volume of injected cement, cement leakage into disc space, and air clefts within fractured vertebrae, were analyzed.
Results
Gradual vertebral height decrease of augmented vertebrae occurred commonly when more than 4 cc of injected cement was used, and when air clefts within fractured vertebrae were seen on admission. In addition, the sagittal Cobb angle more commonly increased during the follow-up period in such cases.
Conclusion
Injection of more than 4 cc of cement during vertebroplasty and air cleft within fractured vertebrae on admission induced gradual vertebral height decrease in augmented vertebrae. Thus, longer follow-up will be needed in such cases, even when patients do not complain of recurrent severe back pain.
Go to : 
Osteoporotic vertebral compression fractures are a major cause of morbidity and disability among the elderly. Percutaneous vertebroplasty is a procedure used to treat a painful compression fracture in the absence of a neurologic deficit. Percutaneous vertebroplasty is a relatively safe and effective treatment for osteoporotic compression fractures.2) After vertebroplasty, progressive decrease of augmented vertebral body height is noted. The radiological differences between refracture and recollapse of augmented vertebrae are unclear. Recollapse of augmented vertebrae may also occur with reappearance of pain.6) When this occurs, aggravation of kyphotic change may be noted. Gradual vertebral body height decrease and kyphotic change may occur even without the reappearance of severe pain. Recollapse of augmented vertebrae may induce severe kyphotic deformity.22) The purpose of this study was to evaluate the risk factors for gradual vertebral body height decrease in augmented vertebrae after vertebroplasty.
Go to : 
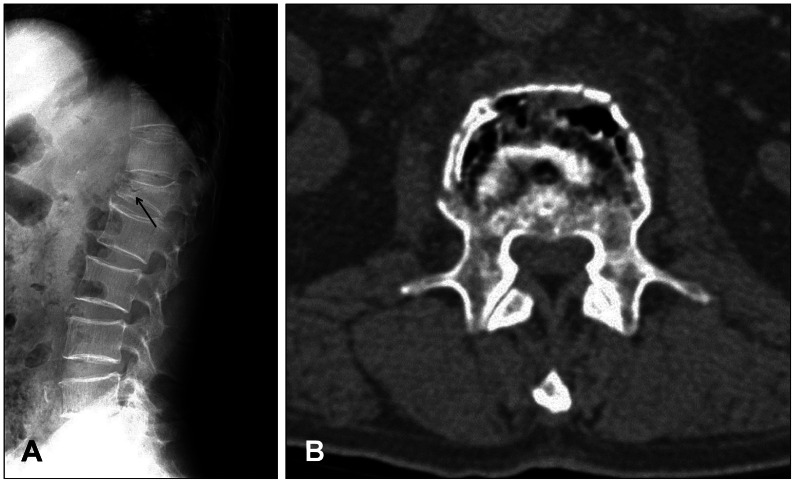
From January 2012 to December 2013, we performed 186 level vertebroplasties for compression fractures in 160 patients. We selected 44 patients, with a first occurrence of a single vertebral compression fracture at the thoracolumbar junction (from T11 to L2). Pathologic fractures were excluded. Patients with subsequent fractures during the follow-up period were also excluded. All patients underwent vertebroplasty using polymethyl methacrylate. Gradually collapsed vertebral fractures were diagnosed with serial radiography or magnetic resonance imaging. We analyzed sex, age, bone mineral density, body mass index (BMI), sagittal Cobb angle, volume of injected cement, level of compression fracture, presence of cement leakage into the disc space and presence of air cleft within the vertebral body on admission (Figure 1). Refracture was defined as recurrent fracture of the same cemented vertebra as on initial admission with severe back pain during follow-up, for which repeat vertebroplasty was performed. Patients with refracture were excluded from our study. Our selected patients did not complain of recurrent severe pain and did not undergo repeat vertebroplasty. In that cases, we defined recollapse or gradual vertebral height decrease in our study. All patients underwent routine follow-up.
All statistical analyses were performed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA). The chi-square test (Pearson) was used to compare the groups. A p-value of less than 0.05 was considered statistically significant.
Go to : 
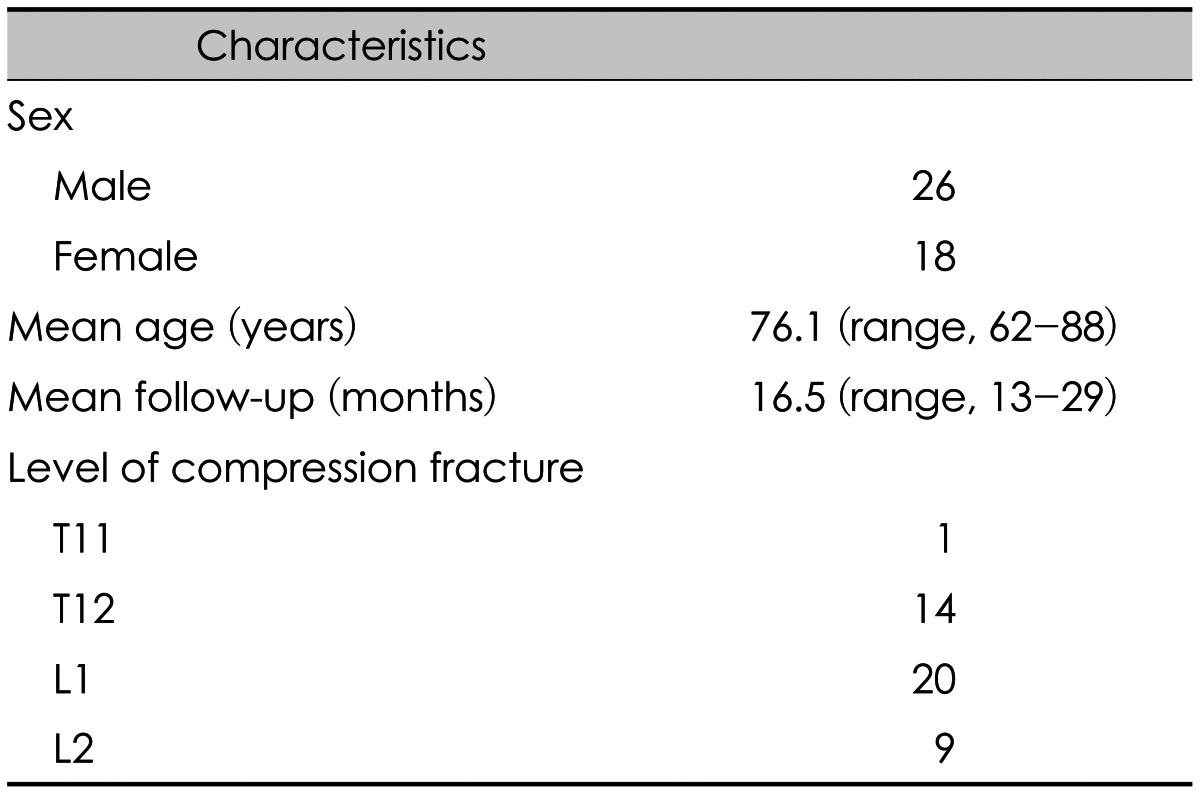
Of the 44 patients, 26 were males and 18 were females. The average age was 76.1 years (range, 62-88 years). The average follow-up period was 16.5 months (range, 13-29 months). The fractured vertebrae, included 1 at T11, 14 at T12, 20 at L1, and 9 at L2 (Table 1). Gradual height decreases were seen in half of the patients.
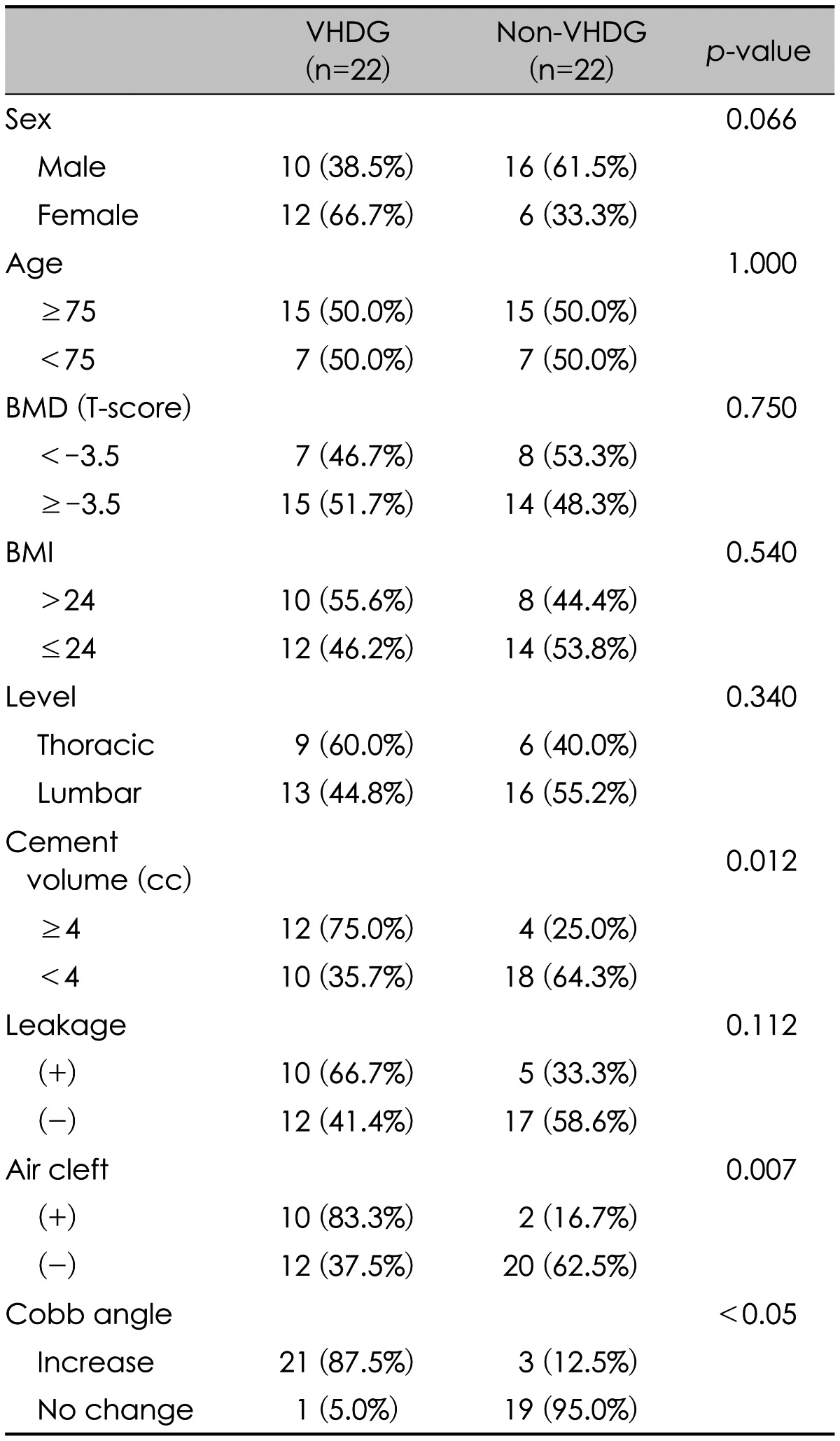
Height decrease of augmented vertebrae occurred in 10 of 26 men (38.5%) and 12 of 18 women (66.7%). The height decrease was more common in women, but the difference was not statistically significant (p=0.066). Patients were divided into two groups. Fourteen were in a group aged less than 75 years, and 30 were aged 75 years or over (average age, 76.1 years). They height decrease of augmented vertebrae occurred at the same rate in the two groups (50.0%). We defined severe osteoporosis as a T-score less than -3.5, which was seen in 29 patients. Height decrease was less common in the severe osteoporosis group (46.7% vs. 51.7%, p=0.750). BMI over 24 was defined as over-weight. Height decrease occurred more commonly (55.6% vs. 46.2%, p=0.540) in this group. Height decrease of augmented vertebrae was more common in the thoracic spine than in the lumbar spine (p=0.340). When cement leaked into the disc space, height decrease was more common (66.7% vs. 41.4%,p=0.112).
When the volume of injected cement was greater than 4cc, height decrease was more common (75.0% vs. 35.7%). The difference was statistically significant (p=0.012). Air clefts within the vertebral body on admission were visualized by plain radiography or computed tomography. When an air cleft was present, height decrease wa more common (83.3% vs. 37.5%, p=0.007). The gradual height decrease of augmented vertebrae increased the sagittal Cobb angle during follow-up with statistical significance (Table 2).
Go to : 
Vertebral body height often increases during vertebroplasty, although the clinical significance of restoring height is unknown.7) Kyphoplasty and vertebroplasty showed similar reduction in pain and disability, with similar safety and complication rates.4)
Vertebroplasty was not associated with increased refracture rates in different vertebrae.2123) However, other report showed refracture of different vertebrae in the vertebroplasty group occurred much sooner than that in a conservative treatment group.21) Recollapse of augmented vertebrae is not relatively common. In our study, vertebral body height gradually decreased during the follow-up period in about half of the patients, without reappearance of severe back pain. Air clefts and greater height restoration of fractured vertebrae were risk factors for recollapse.610) Air clefts within the vertebrae were also prone to vertebral height decrease in our study. Non-cemented-endplate-contact was another important predisposing factor for recollapse.10) Preoperative kyphotic change also influenced recollapse of cemented vertebrae.8)
Cement augmentation restores the strength of treated vertebrae, but leads to an increased endplate bulge and altered load transfer in adjacent vertebrae.16) Cemented vertebrae had a lower elastic modulus, but there was no significant effect on the frequency or severity of an induced fracture within the vertebrae.15) Pneumaticos et al.18) reported that there is no difference in the compressive load of failure between augmented and non-augmented fractured vertebrae. These mechanisms may induce recollapse of augmented vertebrae as well as non-augmented fractured vertebrae. Recollapse was more common with use of calcium phosphate.17) The mechanism of recollapse after vertebroplasty may be thermal necrosis19) and mismatch of elastic modulus, stiffness, and strength at the cement-bone interface.11)
The optimal volume of cement to inject into fractured vertebrae remains controversial. Vertebral augmentation with appropriate amounts of bone cement does not lead to stress peaks under the endplate.1) Bone cement increases subsidence in the posterior regions of the treated endplate and the anterior region of the superior caudal endplate.14) Greater height restoration and solid lump filling cement are risk factors for refracture of cemented vertebrae.313) Greater volume of injected cement contributed to frequent subsequent fracture.12) Cement volume was related to recollapse of fractured vertebrae as well as subsequent fracture.9) But, other studies showed that there was no correlation between injected cement volume and subsequent fracture.520) Our study suggested that more than 4 cc of injected cement may induce a gradual vertebral height decrease after vertebroplasty. Larger cement volume may induce more thermal necrosis and mismatch at cement-bone interface.
A limitation of our study is that follow-up periods were relatively short and did not define the relationship between gradual vertebral height decrease and the clinical significance. So, further studies will be needed about clinical significance of gradual vertebral height decrease.
Go to : 
References
1. Aquarius R, van der Zijden AM, Homminga J, Verdonschot N, Tanck E. Does bone cement in percutaneous vertebroplasty act as a stress riser? Spine (Phila Pa 1976). 2013; 38:2092–2097. PMID: 24026155.

2. Chandra RV, Yoo AJ, Hirsch JA. Vertebral augmentation: update on safety, efficacy, cost effectiveness and increased survival? Pain Physician. 2013; 16:309–320. PMID: 23877447.
3. Chen LH, Hsieh MK, Liao JC, Lai PL, Niu CC, Fu TS, et al. Repeated percutaneous vertebroplasty for refracture of cemented vertebrae. Arch Orthop Trauma Surg. 2011; 131:927–933. PMID: 21191607.

4. Dohm M, Black CM, Dacre A, Tillman JB, Fueredi G. A randomized trial comparing balloon kyphoplasty and vertebroplasty for vertebral compression fractures due to osteoporosis. AJNR Am J Neuroradiol. 2014; 35:2227–2236. PMID: 25300981.

5. Frankel BM, Monroe T, Wang C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007; 7:575–582. PMID: 17905320.

6. Heo DH, Chin DK, Yoon YS, Kuh SU. Recollapse of previous vertebral compression fracture after percutaneous vertebroplasty. Osteoporos Int. 2009; 20:473–480. PMID: 18636218.

7. Hiwatashi A, Moritani T, Numaguchi Y, Westesson PL. Increase in vertebral body height after vertebroplasty. AJNR Am J Neuroradiol. 2003; 24:185–189. PMID: 12591631.
8. Kang SK, Lee CW, Park NK, Kang TW, Lim JW, Cha KY, et al. Predictive risk factors for refracture after percutaneous vertebroplasty. Ann Rehabil Med. 2011; 35:844–851. PMID: 22506213.

9. Kim SG, Yang JC, Kim TW, Park KH. Risk factors for subsequent fracture after osteoporotic vertebral compression fracture. Korean J Neurotrauma. 2013; 9:120–124.

10. Kim YY, Rhyu KW. Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture. Eur Spine J. 2010; 19:1907–1912. PMID: 20559850.

11. Lewis G. Properties of acrylic bone cement: state of the art review. J Biomed Mater Res. 1997; 38:155–182. PMID: 9178743.

12. Li YA, Lin CL, Chang MC, Liu CL, Chen TH, Lai SC. Subsequent vertebral fracture after vertebroplasty: incidence and analysis of risk factors. Spine (Phila Pa 1976). 2012; 37:179–183. PMID: 21240045.
13. Lin WC, Lee YC, Lee CH, Kuo YL, Cheng YF, Lui CC, et al. Refractures in cemented vertebrae after percutaneous vertebroplasty: a retrospective analysis. Eur Spine J. 2008; 17:592–599. PMID: 18204942.

14. Liu WG, He SC, Deng G, Guo JH, Fang W, Zhu GY, et al. Risk factors for new vertebral fractures after percutaneous vertebroplasty in patients with osteoporosis: a prospective study. J Vasc Interv Radiol. 2012; 23:1143–1149. PMID: 22920978.

15. Nagaraja S, Awada HK, Dreher ML, Bouck JT, Gupta S. Effects of vertebroplasty on endplate subsidence in elderly female spines. J Neurosurg Spine. 2015; 22:273–282. PMID: 25525963.

16. Oakland RJ, Furtado NR, Wilcox RK, Timothy J, Hall RM. The biomechanical effectiveness of prophylactic vertebroplasty: a dynamic cadaveric study. J Neurosurg Spine. 2008; 8:442–449. PMID: 18447690.

17. Piazzolla A, De Giorgi G, Solarino G. Vertebral body recollapse without trauma after kyphoplasty with calcium phosphate cement. Musculoskelet Surg. 2011; 95:141–145. PMID: 21468725.

18. Pneumaticos SG, Triantafyllopoulos GK, Evangelopoulos DS, Hipp JA, Heggeness MH. Effect of vertebroplasty on the compressive strength of vertebral bodies. Spine J. 2013; 13:1921–1927. PMID: 23981817.

19. Stańzyk M, van Rietbergen B. Thermal analysis of bone cement polymerisation at the cement-bone interface. J Biomech. 2004; 37:1803–1810. PMID: 15519587.
20. Syed MI, Patel NA, Jan S, Harron MS, Morar K, Shaikh A. Intradiskal extravasation with low-volume cement filling in percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2005; 26:2397–2401. PMID: 16219853.
21. Wagner AL, Baskurt E. Refracture with cement extrusion following percutaneous vertebroplasty of a large interbody cleft. AJNR Am J Neuroradiol. 2006; 27:230–231. PMID: 16418390.
22. Yi X, Lu H, Tian F, Wang Y, Li C, Liu H, et al. Recompression in new levels after percutaneous vertebroplasty and kyphoplasty compared with conservative treatment. Arch Orthop Trauma Surg. 2014; 134:21–30. PMID: 24287674.

23. Yoshii T, Ueki H, Kato T, Tomizawa S, Okawa A. Severe kyphotic deformity resulting from collapses of cemented and adjacent vertebrae following percutaneous vertebroplasty using calcium phosphate cement. A case report. Skeletal Radiol. 2014; 43:1477–1480. PMID: 24880714.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download