Abstract
Traumatic basal ganglia hemorrhage (TBGH) is a rare presentation of head injuries. Bilateral lesions are extremely rare. The pathophysiologic mechanism of bilateral TBGH seems to be the same as diffuse axonal injury. However, limited information about childhood bilateral TBGH is available in the literature. We report the case of a child with bilateral TBGH treated with stereotactic aspiration of hemorrhage and periodic urokinase irrigation.
Traumatic basal ganglia hemorrhage (TBGH) is uncommon in head injuries and is reported in about 3% of patients.3) TBGH is associated with poor prognosis than other types of posttraumatic intracranial hemorrhages. Bilateral TBGH is even rarer and is extremely rare in children. We report a case of a child with bilateral TBGH and discuss our experience concerning treatment and hospital course.
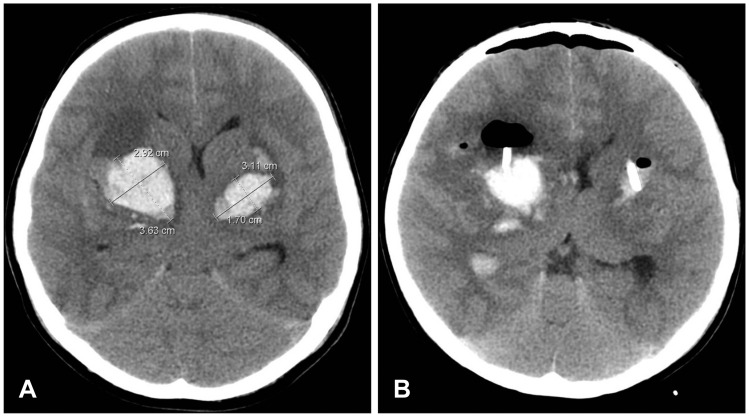
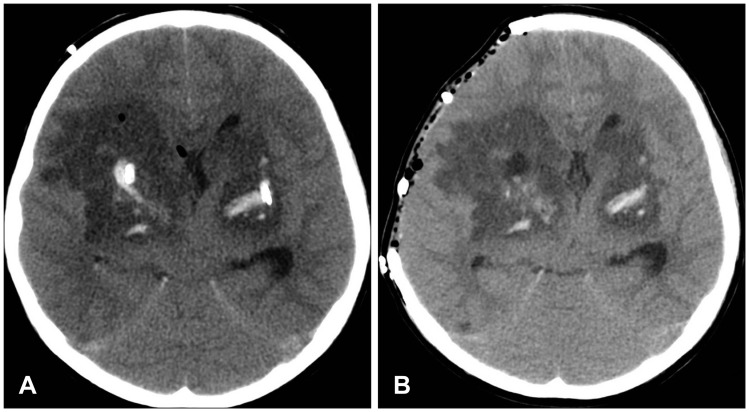
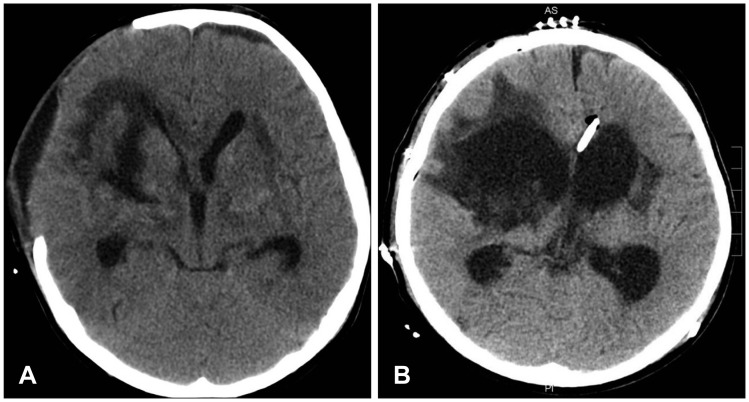
A six-year-old boy was referred to our hospital after a traffic accident. He presented with decreased mentality (Glasgow Coma Scale score of 6), with an endotracheal tube and mechanical ventilation. Pupils were isocoric but sluggish to light. Computed tomography (CT) scans showed bilateral TBGH, about 30 cc in the right side and 20 cc in the left side (Figure 1A). Intraventricular hemorrhage (IVH) was present. We decided to remove bilateral TBGH to reduce increased intracranial pressure (ICP); this was done by bilateral stereotactic hemorrhage aspiration (Figure 1B). Surgery lasted 6 hours and draining catheters were inserted in both operation sites. Postoperatively, he was transferred to the intensive care unit where he was sedated and ventilated. Immediate postoperative brain CT confirmed the appropriate location of both draining catheters and the persistence of hemorrhage, with more hemorrhage on the right side (Figure 1B). We started irrigation via a draining catheter with 8,000 IU of urokinase dissolved in normal saline every 8 hours over 2 days on the right side. After the administration of urokinase, 3 cc normal saline was injected into the clot. At total of 5 cc of diluted urokinase and normal saline were administered. The catheter was then clamped for 30 minutes. The amount of drain was about 110 cc dark-colored blood mixed with cerebrospinal fluid on the right side and less than 5 cc on the left side during the first 24 hours postoperatively. On the second day after operation, brain CT follow-up demonstrated diffuse low density around the previous hemorrhage and severe brain swelling (Figure 2A). Shortly after brain CT, the patient's right pupil size suddenly became dilated and unresponsive to light. Decompressive huge craniectomy and duroplasty were performed (Figure 2B). At postoperative day (POD) 11, brain CT showed further reduction in bilateral TBGH and IVH and enlargement of ventricle size associated with scalp bulging at the operation site (Figure 3A). At POD 39, ventriculoperitoneal shunting and cranioplasty using autologous bone were done (Figure 3B). Currently, he remains in a chronic vegetative condition.
TBGH is uncommon and bilateral TBGH is extremely rare.36) We were unable to find any case of bilateral TBGH in a child in the literature and could not obtain any information about the hospital course and treatment. The child's brain is resilient and able to compensate for acutely increased ICP due to intracerebral hematoma because the skull has expansibility.2) Anatomical aspects of younger child to head injuries are large head to body ratio, relatively weak neck, thinner skull, and larger subarachnoid space in which the brain can move freely.13) For this reason, a child's brain has the ability to expand and buffer against impact but vulnerable to damages.
A small amount of TBGH (<2 cm in diameter) can be considered as a hemorrhagic contusion.4) It can be related to diffuse axonal injury when it is associated with contusions and/or small hemorrhage in the corpus callosum, basal ganglia, tegmentum of pons, IVH, and acute brain swelling.11) The pathophysiologic mechanism of unilateral TBGH is unclear, but is believed to occur from shear strain in ganglionic lesion.12) Mosberg and Lindenberg4) demonstrated a traumatic tear of a pallidal branch of anterior choroidal artery as the origin of pallidal hematoma in an autopsy case. Head injuries including traffic accidents associated with acceleration and deceleration forces with rotational movement traumatic dissection of perforating arteries, mainly the anterior choroidal artery or lenticulostriate artery, can cause basal ganglia hemorrhage.61012) Still, the exact explanation for bilateral TBGH is elusive in the literature. We think this phenomenon could develop by similar mechanism, but do not know whether the hemorrhage developed simultaneously in both sides or separately over time.
In this case, initial CT scans showed a difference in hemorrhage volume on both sides of the brain, with the larger diameter of 3.6 cm on the right side and 3.1 cm on the left side. This finding did not provide any clues about the mechanism of bilateral hemorrhage development, especially the time sequence.
Whether to treat this patient or not depended on his clinical condition. Our patient showed poor neurological condition at admission and we decided to remove both hemorrhage areas using stereotactic aspiration and periodic urokinase irrigation. Six hours after admission the operation was performed and urokinase irrigation was done every 8 hours. No literature references concerning urokinase irrigation for children are available; we decided to use 8,000 IU of urokinase, which is the amount that we usually use to treat adult patients. Initially, 5 cc of regimen would be tolerable for a child. During the first 24 hours postoperatively, 110 cc was drained from the right side indicating cerebrospinal fluid mixture, with <5 cc drained from the left side. Routine brain CT at POD2 demonstrated markedly decreased hemorrhage at both basal ganglia but diffuse low density lesions around the previous hemorrhage. These findings are not typical in adult basal ganglia hemorrhage and we presumed the cause of this finding the possibility of the urokinase overdosage and toxicity. Brain edema caused by thrombin might be greatly amplified by the presence of plasminogen activators, perhaps because the latter compete for naturally occurring thrombin inhibitors.1) The authors concluded that in the context of intracerebral hemorrhage the use of tissue plasminogen activator or urokinase (uPA) to lyse clotted blood in brain parenchyma may promote edema formation in surrounding tissue.7) A case featuring protracted perihematomal edema after hematoma evacuation and fibrinolysis therapy with uPA was reported.8) Recent studies indicate that no differences in permeability could be detected between newborn and adult blood-brain barrier (BBB) capillaries and the newborn BBB has restrictive properties similar to that of the adult. In our case under the condition of BBB disruption due to initial hemorrhage injection of adult dose of urokinase into the hemorrhage site may aggravate cerebral edema around cerebral tissue.579) Also, the total of 110 cc drainage through the right draining catheter may have masked this edema formation during the first postoperative 24 hours. Thus we presumed his neurological condition was poor and that a second operation was needed.
References
1. Figueroa BE, Keep RF, Betz AL, Hoff JT. Plasminogen activators potentiate thrombin-induced brain injury. Stroke. 1998; 29:1202–1207. discussion 1208. PMID: 9626295.

2. Kang JK, Park CK, Kim MC, Kim DS, Song JU. Traumatic isolated intracerebral hemorrhage in children. Childs Nerv Syst. 1989; 5:303–306. PMID: 2805000.

3. Katz DI, Alexander MP, Seliger GM, Bellas DN. Traumatic basal ganglia hemorrhage: clinicopathologic features and outcome. Neurology. 1989; 39:897–904. PMID: 2739917.

4. Mosberg WH, Lindenberg R. Traumatic hemorrhage from the anterior choroidal artery. J Neurosurg. 1959; 16:209–221. PMID: 13642112.

5. Narayan RK, Narayan TM, Katz DA, Kornblith PL, Murano G. Lysis of intracranial hematomas with urokinase in a rabbit model. J Neurosurg. 1985; 62:580–586. PMID: 3973729.

6. Öğrenci A, Ekşi MŞ, Gün B, Koban O. Traumatic basal ganglia hematoma following closed head injuries in children. Childs Nerv Syst. 2016; 32:1237–1243. PMID: 26994013.

7. Rohde V, Rohde I, Thiex R, Ince A, Jung A, Dückers G, et al. Fibrinolysis therapy achieved with tissue plasminogen activator and aspiration of the liquefied clot after experimental intracerebral hemorrhage: rapid reduction in hematoma volume but intensification of delayed edema formation. J Neurosurg. 2002; 97:954–962. PMID: 12405387.

8. Seo DH. Protracted perihematomal edema after fibrinolysis therapy with urokinase. Korean J Cerebrovasc Surg. 2003; 5:153–157.
9. Sharma GV, Cella G, Parisi AF, Sasahara AA. Thrombolytic therapy. N Engl J Med. 1982; 306:1268–1276. PMID: 7040966.

10. Sobani ZA, Ali A. Pediatric traumatic putamenal strokes: Mechanisms and prognosis. Surg Neurol Int. 2011; 2:51. PMID: 21697966.

11. Vega MB, Hamamoto Filho PT, Machado Cde J, Zanini MA. Traumatic brain injury presenting with bilateral basal ganglia hemorrhage. Neurol Neurochir Pol. 2015; 49:456–459. PMID: 26652883.

12. Zimmerman RA, Bilaniuk LT, Genneralli T. Computed tomography of shearing injuries of the cerebral white matter. Radiology. 1978; 127:393–396. PMID: 644064.

13. Zuckerman GB, Conway EE Jr. Accidental head injury. Pediatr Ann. 1997; 26:621–632. PMID: 9339463.

FIGURE 1
Initial preoperative and postoperative non-contrast computed tomography (CT) scans of a 6-year-old boy. (A) Preoperative brain CT scan showing traumatic bilateral hemorrhage of the basal ganglia. (B) Postoperative brain CT scan. He underwent bilateral stereotactic aspiration.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download