Abstract
Intracranial wooden foreign bodies are rare. In addition, such objects are difficult to identify with conventional radiographic techniques, such as X-ray radiography or brain computed tomography. A 48-year-old man presented to our emergency room with a headache. Even though he had a history of trauma, he had no external wounds and showed no neurological deficits at the initial examination. He was initially diagnosed with trauma-related pneumocephalus. He developed a delayed intracranial infection and underwent surgery to remove the wooden foreign body. The present case illustrates the necessity for special attention to patients suspected of having pneumocephalus with a rare presentation during the initial examination. Early surgical removal of the intracranial foreign body is necessary to prevent complications.
Intracranial foreign bodies frequently result from trauma, including penetrating injury, and rarely involve wooden materials compared with metallic materials. When intracranial penetrations of wooden objects occur through the transnasal or transorbital route, physical examinations may reveal no abnormalities, and the objects may be difficult to visualize with conventional radiography. We present a case involving the transnasal intracranial penetration of a wooden branch that resulted in a delayed intracranial infection due to initial misdiagnosis.
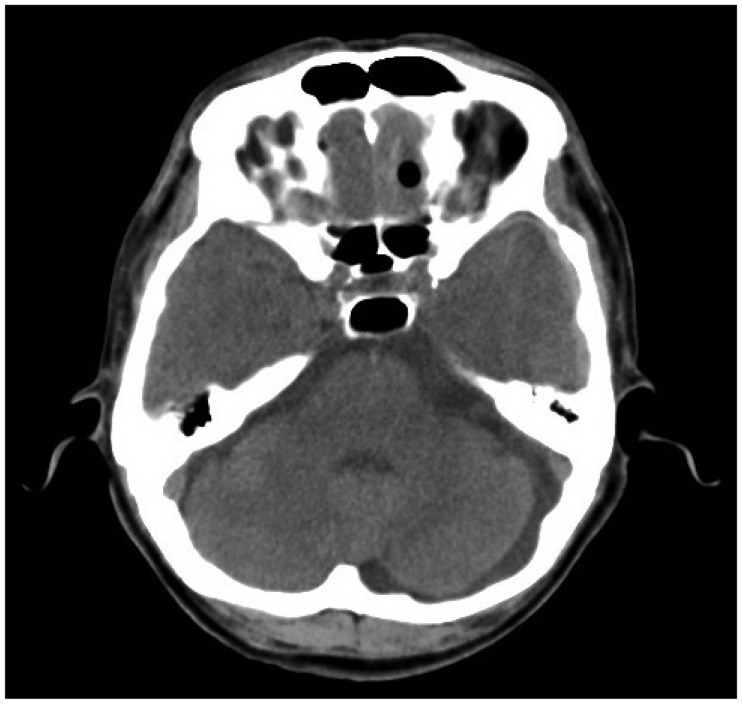
A 48-year-old man presented to the emergency department with complaints of headache the day before. Two days earlier, he fell to the ground in a drunken state, and he could not clearly remember the incident. At the emergency department, no neurological or physical abnormalities, such as external contusions or cerebrospinal fluid rhinorrhea, were observed. A routine simple radiograph revealed no skull fracture (Figure 1). Computed tomography (CT) that was performed upon admission showed a round hypodense signal in the left frontal area, which suggested pneumocephalus, and a small amount acute subdural hematoma in the left frontotemporoparietal area (Figure 2 and 3).
The patient was admitted to the neurosurgical department for close observation, and prophylactic antibiotics were administered for the pneumocephalus. Several days after admission, the patient developed a generalized tonic-clonic seizure. Brain magnetic resonance imaging (MRI) revealed a fistula from the left nasal cavity to the frontal lobe with enhancement along the tract and ventricular lining (Figure 4). He underwent a transnasal endoscopic operation performed by the otorhinolaryngologic team. The foreign body was a wooden branch (11 cm long and 0.7 cm wide) covered with brain tissue (Figure 5).
After the operation, the patient received intravenous antibiotics (ceftriaxone plus vancomycin) for over 2 months. A microbiologic culture study on the foreign body showed gram-positive cocci (S. aureus). The postoperative course was uneventful, and he was discharged without neurological deficits.
Intracranial penetrating injuries by foreign bodies represent only 0.4% of all head injuries and usually occur in children because of falls.17) Intracranial foreign bodies that cause severe intracranial infections can be fatal.8) Miller et al.7) reviewed 42 cases with intracranial penetrating injuries and found that 64% developed central nervous system infections, 45% had additional brain abscesses, and the death rate was 25%. Generally, the time from the injury to the clinical intracranial infection presentation is long, but it can vary from a few days to several years.5) Therefore, careful history taking and thorough physical and radiologic examinations are essential.
However, intracranial wooden foreign bodies are difficult to detect with plain radiographic techniques and distinguish from periorbital fat and air in the nasal cavity on CT images.48) The CT attenuation values of wooden foreign bodies vary depending on their water content. Freshly cut wood has a relatively high physical density because of its high water content; therefore, it is difficult to distinguish it from soft tissues, such as muscle and vitreous.3) Conversely, when wood dries, the water is gradually replaced by gas, and its density is difficult to distinguish from that of fat or air.3) Consequently, intracranial wooden foreign bodies have variable densities over time and are difficult to distinguish from the surrounding structures. However, an interesting study was conducted on CT images of wooden foreign bodies. Tasneem et al.11) described a case involving a radiolucent intracranial wooden foreign body and the usefulness of the lung window setting for detecting wooden foreign bodies on CT images. Careful review of CT images with the lung window setting can be helpful for detecting a wooden foreign body. Unlike CT images, MRI is more useful for detecting wooden foreign bodies that appear hypointense on T1- and T2-weighted MRI scans and that can be distinguished from air or fat.69) In addition, infected lesions exhibit Gadolinium enhancement.
The initial CT image of the patient showed a single area of air in the frontal lobe. A pneumocephalus with this location and pattern is very rare. Steudel and Hacker10) reviewed 508 cases with acute head injuries and found that 49 (9.7%) had a pneumocephalus on brain CT scans, with 5 (1%) showing a single air bubble and 6 (1.1%) having an intracerebral or intraventricular location. However, they did not experience a case involving a single air bubble with an intracerebral or intraventricular location. These findings suggest that patients with a pneumocephalus with a rare presentation need to be examined more carefully.
Patients with retained intracranial wooden foreign bodies frequently develop delayed infectious complications, and surgical removal is necessary, even in the absence of symptoms.178) Our patient experienced late-onset seizures, which could have been secondary to gradual gliosis, progressive granulomatous changes, or delayed abscess formation, as has been noted in cases with retained foreign bodies.2) Therefore, if intracranial injury from a wooden foreign body is suspected, careful history taking and imaging are very important. Once the diagnosis of an intracranial foreign body is confirmed, surgical removal of the foreign body is required.
References
1. Arifin MZ, Gill AS, Faried A. Penetrating skull fracture by a wooden object: Management dilemmas and literature review. Asian J Neurosurg. 2012; 7:131–134. PMID: 23293668.

2. Aulino JM, Gyure KA, Morton A, Cole JW. Temporal lobe intraparenchymal retained foreign body from remote orbital trauma. AJNR Am J Neuroradiol. 2005; 26:1855–1857. PMID: 16091543.
3. Dalley RW. Intraorbital wood foreign bodies on CT: use of wide bone window settings to distinguish wood from air. AJR Am J Roentgenol. 1995; 164:434–435. PMID: 7839984.

4. Hansen JE, Gudeman SK, Holgate RC, Saunders RA. Penetrating intracranial wood wounds: clinical limitations of computerized tomography. J Neurosurg. 1988; 68:752–756. PMID: 3357035.

5. Horner FA, Berry RG, Frantz M. Broken pencil points as a cause of brain abscess. N Engl J Med. 1964; 271:342–345. PMID: 14171802.

6. Krimmel M, Cornelius CP, Stojadinovic S, Hoffmann J, Reinert S. Wooden foreign bodies in facial injury: a radiological pitfall. Int J Oral Maxillofac Surg. 2001; 30:445–447. PMID: 11720049.

7. Miller CF, Brodkey JS, Colombi BJ. The danger of intracranial wood. Surg Neurol. 1977; 7:95–103. PMID: 835079.
8. Nishio Y, Hayashi N, Hamada H, Hirashima Y, Endo S. A case of delayed brain abscess due to a retained intracranial wooden foreign body: a case report and review of the last 20 years. Acta Neurochir (Wien). 2004; 146:847–850. PMID: 15254807.

9. Specht CS, Varga JH, Jalali MM, Edelstein JP. Orbitocranial wooden foreign body diagnosed by magnetic resonance imaging. Dry wood can be isodense with air and orbital fat by computed tomography. Surv Ophthalmol. 1992; 36:341–344. PMID: 1566235.

10. Steudel WI, Hacker H. Prognosis, incidence and management of acute traumatic intracranial pneumocephalus. A retrospective analysis of 49 cases. Acta Neurochir (Wien). 1986; 80:93–99. PMID: 3716896.
11. Tasneem K, Concannon ES, Abulkhir A, Ryan RS, Barry K. Radiolucent wooden foreign body masquerading as a depressed skull fracture. BMJ Case Rep. 2011; 12. 20. epub ahead of print. DOI: 10.1136/bcr.10.2011.4964.

FIGURE 2
A brain computed tomography scan with an axial view demonstrating air density in the left frontal lobe and subdural hematoma on the left convexity.

FIGURE 3
A brain computed tomography scan with an axial view demonstrating air density of nasal cavity.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download