This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
Injuries of upper cervical spine are potentially fatal. Thus, appropriate diagnosis and treatment is essential. In our institute, preoperative computed tomography angiography (CTA) has been performed for evaluation of injuries of bony and vascular structure. The authors confirmed the engorged venous plexus within injured posterior neck muscle. We have this research to clarify the relationship between the engorged venous plexus and engorged vein.
Methods
A retrospective review identified 23 adult patients who underwent 23 posterior cervical spine surgeries for treatment of upper cervical injury between 2013 and 2015. Preoperative CTA was used to identify of venous engorgement within posterior neck muscle. The male to female ratio was 18:5 and the mean age was 53.5 years (range, 25-78 years). Presence of venous engorgement and estimated blood loss (EBL) were analyzed retrospectively.
Results
The EBL of group with venous engorgement was 454.55 mL. The EBL of group without venous engorgement was 291.67 mL. The EBL of group with venous engorgement was larger than control group in significant.
Conclusion
The presence of engorged venous plexus is important factor of intraoperative bleeding. Preoperative CTA for identifying of presence of engorged venous plexus and fine operative techniques is important to decrease of blood loss during posterior cervical spine surgery.
Go to :

Keywords: Surgical blood loss, Spinal injury, Venous engorgement
Introduction
Upper cervical injuries (UCI) consist of a various type of injuries that affect the skull base, the atlas, and the axis.
1214) Around this bony structure, important organs such as, brain stem, cranial nerve, vertebral artery, muscle and ligaments exist. Moreover, craniocervical junction and atlantoaxial complex made motion including axial rotation, flexion and extension. Therefore, after injured to this articular structure, neurologic deficit and instability is able to result.
91214) To maintain stability, prevent deformity, and protect neurological function, UCI need a proper treatment. When our institute evaluate patients with UCI in emergency rooms, computed tomography angiography (CTA) of cervical spines was performed routinely for confirmation of vascular structure injuries. On CTA, we can found that abnormal vascular structure with contrast enhancement and dilatation within paraspinal back muscle. This abnormal vascular structure is considered as engorged venous plexus. We assumed that venous engorgement induced massive bleeding during muscle dissection. In this study, we evaluated the relation of venous engorgement and blood loss for adult patients with UCI.
Go to :

Materials and Methods
Baseline characteristics and inclusion criteria
Between 2013 and 2015, total 23 patients with posterior fusion operations for UCI were enrolled. Medical data were collected according to our protocol and reviewed retrospectively under approval of the institutional review board. The inclusion criteria were as follows: 1) patients with upper cervical blunt trauma treated by only emergency posterior fusion surgery, aged ≥20 years; 2) diagnosed of UCI via X-ray, computed tomography (CT) and magnetic resonance (MR); 3) performed CTA for evaluation of vascular structure injury; 4) had no past medical history and took any medication. Patients with spinal cord compression who needed laminectomies for minimizing the addition of the bone bleeding, and diagnosed as vascular diseases such as arteriovenous fistula were excluded. Initial prothrombin time (PT) international normalized ratio (INR), activated partial thromboplastin time (aPTT) and platelet count were checked as laboratory findings related to bleeding factors.
Venous engorgement evaluation and estimated blood loss (EBL)
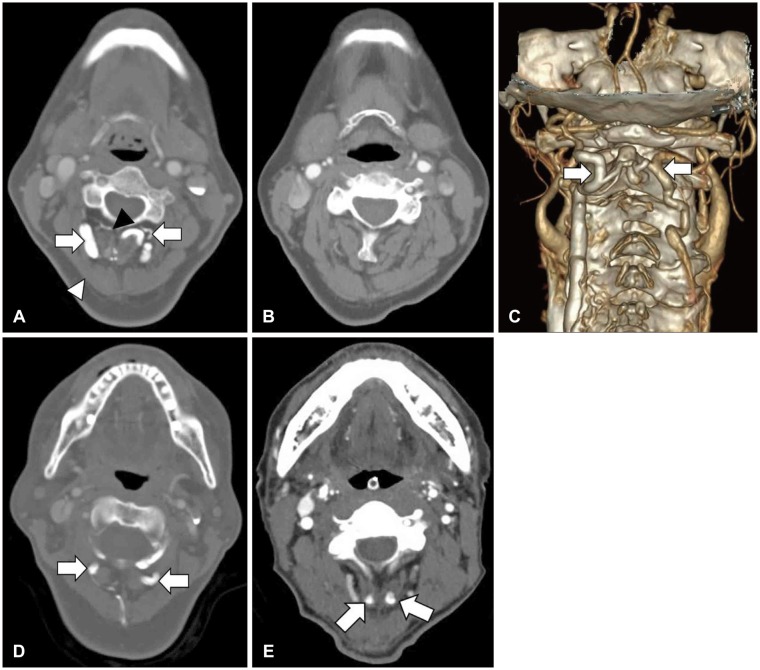
We confirmed the venous engorgement in posterior neck muscle as CTA. The venous engorgement was defined as unusual venous structure over 3 mm with enhancement and dilatation within paraspinal neck muscle by CTA (
Figure 1). Radiologic findings were confirmed by two neurosurgeon and neuroradiologist. Patients were divided into two groups based on engorged vein size of 3 mm. Previous studies found the diameter of vertebral artery at levels of C1 and C2 to be about 3 mm.
613) Based on this, the authors judged the vein of more than 3 mm thick as venous engorgement.
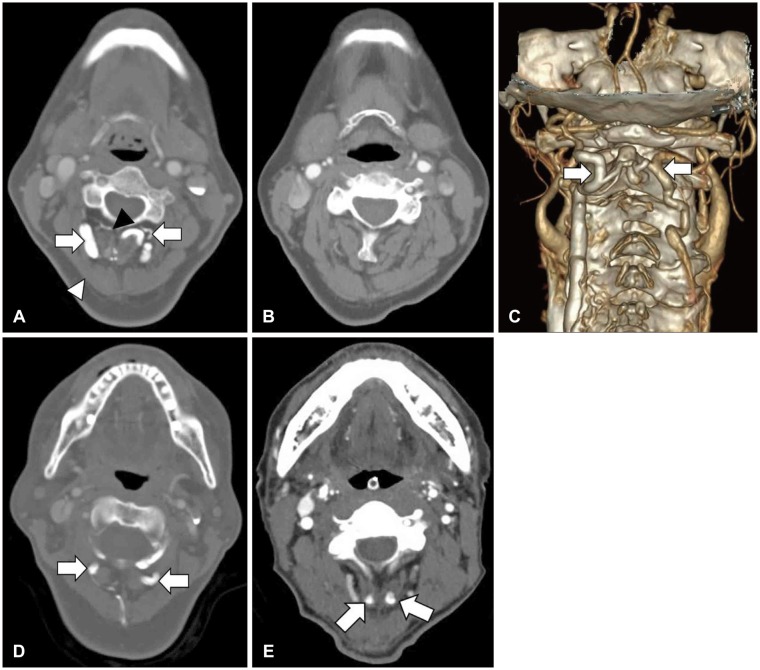 | FIGURE 1Preoperative computed tomography angiography (CTA). Three traumatic patients were performed the CTA examination preoperatively. (A) Engorged venous structures are showed. Semispinaliscapitus muscles (white arrowhead), multifidus muscles (black arrowhead) and engorged venous plexus (white arrows) are indicated. (B) On CTA, engorged venous plexus disappear after one month. (C) Three dimensions reconstructive image shows dilatated venous structures (white arrows). (D, E) Engorged venous plexus (white arrows) were showed.
|
The EBL was confirmed in anesthesia records. Anesthesiologist was determined the EBL on the basis of blood soaking gauzes, fluid volume of suction bottles, transfusion volume.
CTA protocol
The patients were laid supine on the table with neutral position. CTA was performed (General electric Discovery CT 750HD; GE Healthcare, Milwaukee, WI, USA) after injecting 80 mL of nonionic iodinated contrast material (iodine concentration, 755 mg/mL) through a 20 gauge intravenous cannula at a rate of 4 mL/s. After 20 seconds from the contrast material injection, enhanced images were obtained. The final image is reconstructed by the software (AW Volume Share 5; GE Healthcare, Milwaukee, WI, USA).
Analysis
The relation of EBL and venous engorgement were analyzed. Independent-Samples t-test was used to assess the difference between group with venous engorgement and control group. Also, We analyzed the relationship between EBL and other variables. Statistical methods were noted in the following tables. All p-values of less than 0.05 were considered to indicate statistical significance. All statistical analyses were conducted with the use of statistical software package SPSS (Version 24.0; SPSS Inc., Chicago, IL, USA).
Go to :

Results
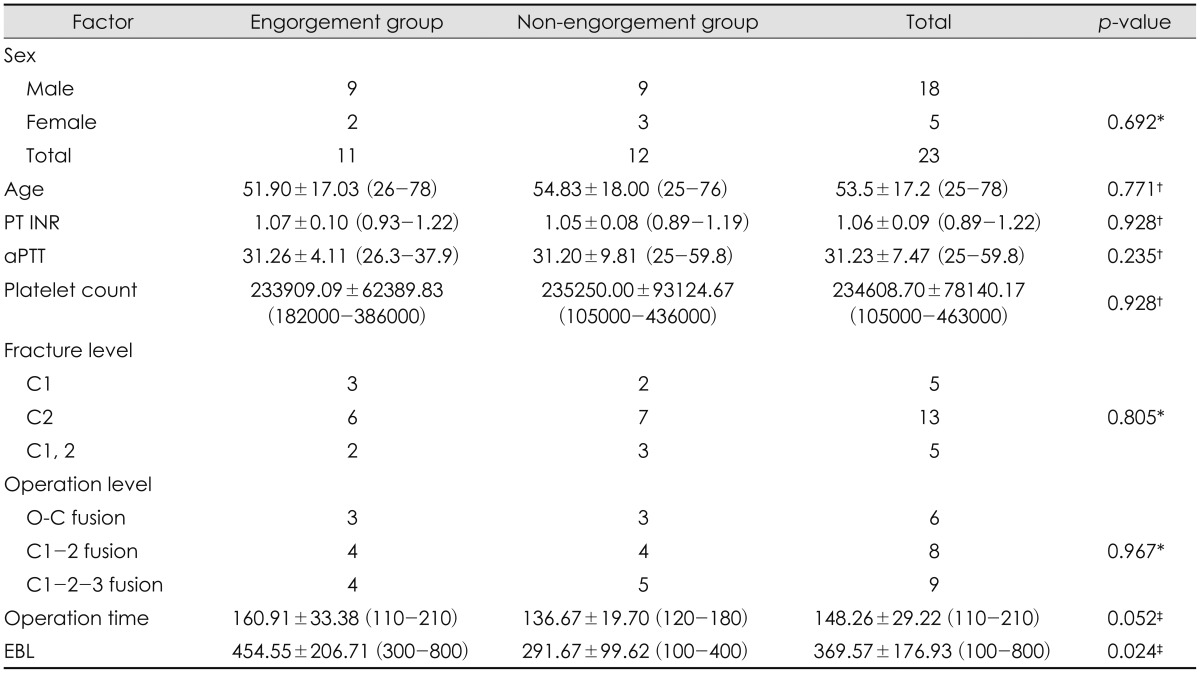
All patients underwent surgery, the postoperative management was terminated without any problems. Patient's characteristics are shown in
Table 1. The male to female ratio was 18:5 and the mean age was 53.5 years (range, 25-78 years). Of 23 patients, 11 patients had venous engorgement in posterior neck muscle. EBL of total enrolled patients was 369.57 mL (range, 100-800). The EBL of group with venous engorgement was larger than that of control group as 454.55±206.71 in significant (
p<0.05) (
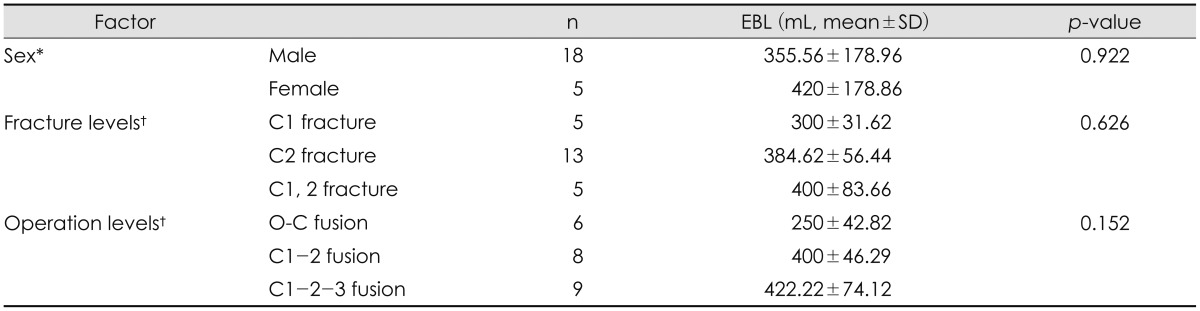
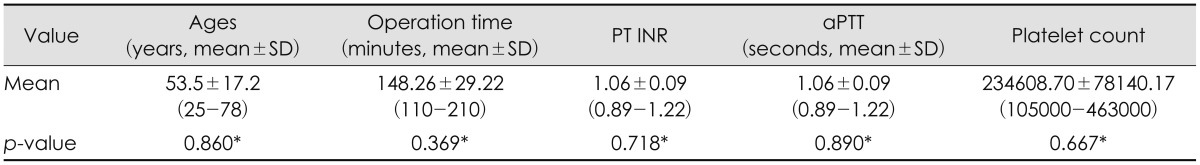
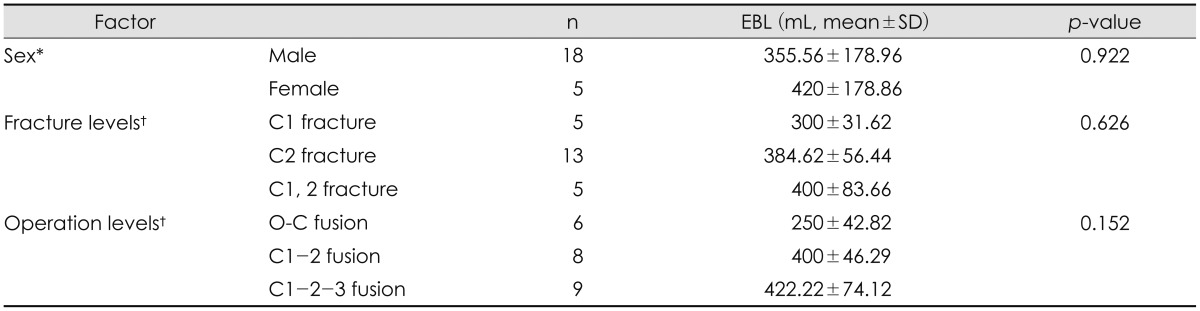
Table 1). However, the other variants did not have statistical significance (
Table 2 and
3).
TABLE 1
Baseline characteristics
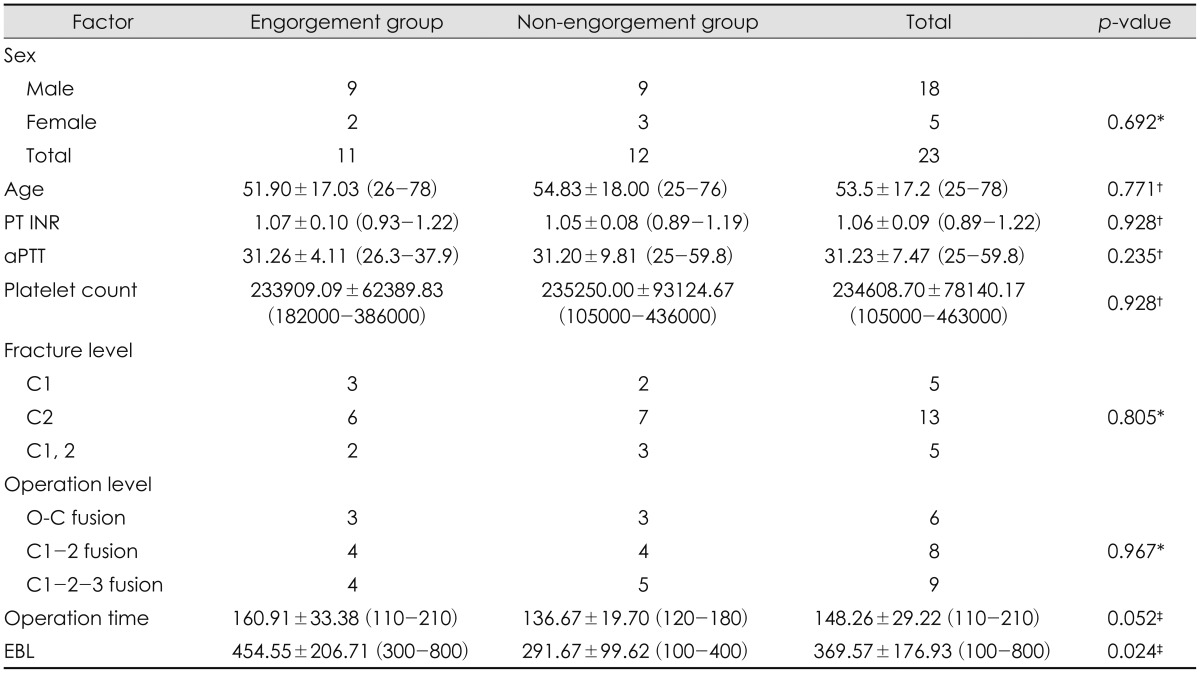

TABLE 2
The relation of estimated blood loss and other variants
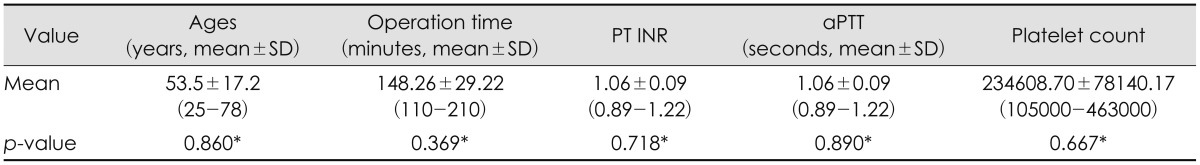

TABLE 3
The relation of estimated blood loss and other variants

Go to :

Discussion
The present study compared EBL between groups with/without post-traumatic muscular venous engorgement during upper cervical spinal fusion operations. Both groups in the present study had significant difference in EBL. Current surgical approaches for treating UCI have developed through the continuous innovations in surgical technique, since in 1891 Hadra first introduced spinous process wiring in Pott's disease and in 1942
4) Rogers
16) described the interspinous wiring method used for trauma-induced cervical instability. Recently, several surgery approaches have been attempted to treat UCI, including wiring technique, interlaminar clamps, and screw insertion.
25810151719) Especially, the C1 lateral mass and C2 pedicle screws are biomechanically considered more rigid and got a higher fusion rate than other techniques.
11)
However, intraoperative bleeding has been recognized as a common complication during posterior spine fixation surgery. As previous study, there are known various risk factors associated with bleeding in spine surgery such as patient position, past medical history, operation technique and levels.
718) The major causes of intraoperative bleeding were muscular and bony bleeding and injured of vascular structure. Arnautović et al.
1) reviewed and revealed the venous anatomy at the craniocervical junction.
3) The authors emphasized the importance of suboccipital cavernous sinus, they proposed to describe the venous compartment surrounding the vertebral artery at the skull base. They described it have many communication vessel, that anastomotic vein, which connects to the suboccipital venous plexus, placed between the deep and intermediate muscle layers. We reviewed the medical records, laboratory examinations, and radiologic findings of patients who had massive bleeding during surgery. Authors were able to observe some patients with engorged venous structures.
Figure 1 shows that engorged venous plexus located between the semispinalis capitus and multifidus muscle. In patients with blunt cervical trauma, we suppose that contusion and swelling of deep muscle may exist and affect the progression of venous congestion. In some patients who did not receive surgical treatment, we observed that the engorged venous plexus disappeared later (
Figure 1C). Between engorged vein and EBL, there was statistically relevant. According to our research, engorged venous structures are considered as a new risk factor. We presumed two reasons for the difference of EBL according to venous engorgement. First, intraoperative injuries of engorged venous plexus might cause much bleeding. Second, venous engorgement leads to congestion of blood, which is the major reason for increased EBL. Therefore, this hypothesis results in more bleeding as muscular layer dissection in patients with engorged venous plexus.
We propose the following method for reducing the EBL during surgery. 1) Confirmation of presence of the engorged venous plexus via preoperative CTA; 2) decrease of muscular damage by midline approach and fine dissection. The more muscle damage leads massive oozing bleeding due to engorged venous structures. Therefore it is important to midline approach and delicate dissection for avoiding of muscle damage. If massive bleeding occurs, it can be controlled by applying hemostatic materials and manual compression; 3) delayed operation for patients who did not have neurologic symptoms with the engorged venous plexus.
The current study has several limitations. First, this study examined a small number of patients. Second, the other main limitation of this research is the method of EBL calculation. Although identified as anesthesiology records will vary slightly depending on the experience of the anesthesiologist. So, studies are needed to determine the EBL by using the quantitative figures such as pre/postoperative hemoglobin, hematocrit, transfusion, etc. Nonetheless, our findings suggest that the presence of engorged venous plexus results in more bleeding during operation.
Go to :

Conclusion
Intraoperative bleeding is important problems for hemodynamic instability, operative wound and infection. This study confirms that the presence of engorged venous plexus is one of factors, which cause more bleeding after blunt trauma of cervical spine. This problems is solved by preoperative CTA for identifying of presence of engorged venous plexus and fine operative techniques.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download