Abstract
Objective
Bisphosphonate, a typical bone resorption inhibitor, is an important first-line drug for treating osteoporosis. Recent studies show a novel paradigm in stimulating bone formation. Teriparatide, which is composed of recombinant human parathyroid hormone, stimulates osteoblasts and induces bone regeneration. Bone mineral density (BMD) that was used before and after the treatment with anti-osteoporosis drug was compared for the effectiveness in therapy between a combination of teriparatide and selective estrogen receptor modulator (SERM), and bisphosphonate.
Methods
We retrospectively reviewed the outcomes of 85 postmenopausal women who were concurrently diagnosed with osteoporosis and spinal compression fracture between November 2008 and January 2015. The targeted group were treated with teriparatide and SERM (TS group, n=26) and bisphosphonate (B group, n=59).
Results
In both groups, BMD of femur neck was not improved after the medication. In the TS group, on the other hand the BMD and T-score of lumbar spine has significantly improved. BMD ratio of lumbar spine was prominently higher than those of TS group.
Conclusion
The combination therapy of teriparatide and SERM was very effective in treating the lumbar spine, compared to that of bisphosphonate. Although the period of teriparatide treatment has been relatively short, the preventive effects of compression fracture were considerable. Thus, combination therapy of teriparatide and SERM is highly recommended for patients who are concerned with spinal compression fracture from osteoporosis.
Despite various studies, osteoporosis is one of the most major health problems, especially among elderly women. There are two major categories in managing osteoporosis: bone resorption inhibition and bone formation stimulation. Recently, more attention has been focused on teriparatide as a stimulator of bone formation. Teriparatide is a genetically engineered recombinant human parathyroid hormone (PTH) which acts as a bone anabolic drug in treating osteoporosis. The mechanism of this drug is similar to that of endogenous human PTH.168) Human PTH and teriparatide binds to the same receptor on osteoblasts and stimulates osteoblastic effects on bone.4) Daily injection of teriparatide stimulates osteoblast activity improving bone architecture. This drug is approved by the United States Food and Drug Administration as a treatment for osteoporosis.3)
Bisphosphonate, estrogen, selective estrogen receptor modulators (SERM), calcitonin and calcitriol are representative bone resorption inhibitors. Of these, bisphosphonate is the first line treatment and is among the most popular and cost-effective for osteoporosis. Bisphosphonate acts by inhibiting the digestion of bone encouraging osteoclasts to undergo apoptosis. Regulating calcium and bone metabolism, SERM assumes the role of estrogen in postmenopausal women. Unlike SERM, other therapies utilize the human monoclonal antibody denosumab and, in hypogonadal men, testosterone.
We compared the combination of teriparatide and SERM with bisphosphonate to treat osteoporosis for menopausal women and its effect on bone mineral density (BMD) in lumbar spine and femur neck.
Between November 2008 and January 2015, we retrospectively reviewed postmenopausal female patients at 52-88 years of age (mean 70.25±9.03 years) diagnosed with compression fracture diagnosed by spine X-ray and spine magnetic resonance imaging. Osteoporotic patients were divided into two groups based upon treatment: teriparatide (Forsteo®) plus SERM (Evista®) (TS group, n=26) and bisphosphonate (Alend®; B group, n=59). Patients who agreed to use teriparatide, were indicated TS group, and B group patients refused to inject teriparatide. After the discontinuation teriparatide treatment, 26 patients were treated via continuous oral SERM drug. The teriparatide therapy was discontinued mainly due to its expensive cost compared to those of other osteoporotic drugs. The Institutional Review Board of our hospital approved the study protocol. The informed consents were waived by the board.
Patients in the TS group used teriparatide during 3.23±1.63 months, before the change to SERM. The longer use of teriparatide was encouraged. However, patients requested to stop drug injection for financial reasons.
We evaluated the therapeutic outcome of patients for BMD indirectly by measuring bone strength and fracture risk. BMD was measured twice (at the start of medication therapy and following therapy) in the femur and lumbar spine region via dual X-ray absorptiometry using a Hologic discovery-Wi model. Compression fracture level was excluded to avoid masking BMD increase. Outcome was evaluated by comparing BMD changes and calculating the BMD ratio as follows:
Numerical data were presented in terms of the mean range, and tested for statistical significance using the Student t-test. Categorical data were indicated as frequencies and percentages, and then compared using the Pearson chi-square test, or Fisher's exact test. The difference was considered to be statistically significant when the p value was less than 0.05. All statistical analyses were conducted using IBM SPSS Statistics version 22 (SPSS Inc., Chicago, IL, USA).
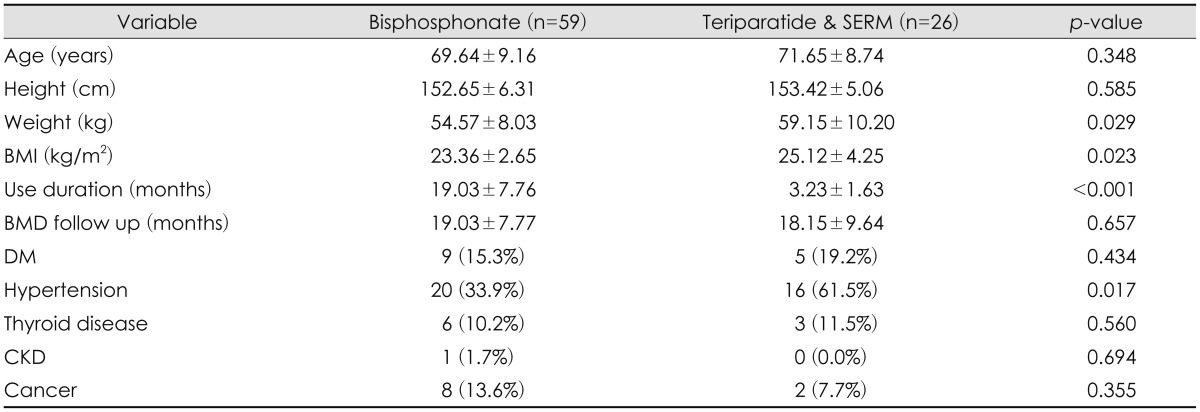
The demographics of the 85 patients are summarized in Table 1. Mean age was 70.25±9.03 years, mean body mass index was 23.90±3.30 kg/m2. The TS group was treated during 3.23±1.63 months and then with teriparatide, and the B group was treated for 19.03±7.76 months.
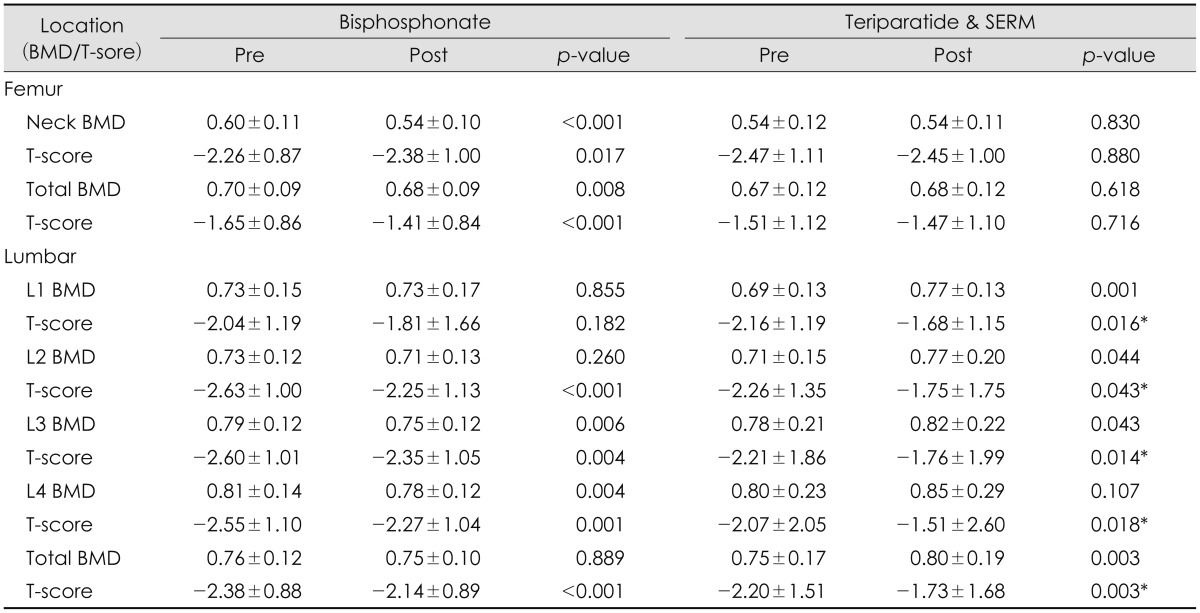
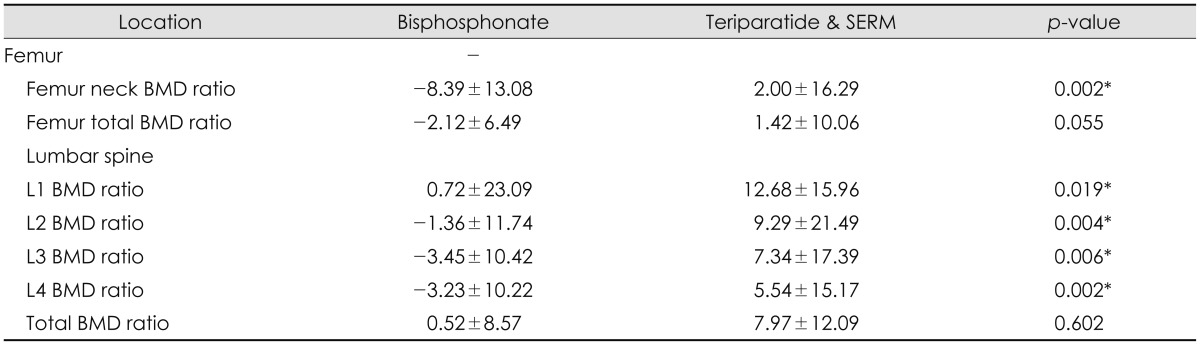
In the TS group, there was no change BMD of femur neck (0.54±0.12 vs. 0.54±0.11), but the T-score was marginally increased from -2.47±1.11 to -2.45±1.00. In contrast, in the B group, BMD of femur neck and T-score decreased from 0.60±0.11 to 0.54±0.10, and from -2.26±0.87 to -2.38±1.00, respectively. BMD and T-score of the lumbar spine increased in the TS group, whereas the B group displayed a decrease L1 BMD and total BMD in B group (Table 2). Especially, in the TS group, all of lumbar spine T-score was increased significantly. BMD ratio of femur neck increased in the TS group (2.00±16.29) but decreased in the bisphosphonate group (-8.39±13.08) (p=0.002). In lumbar spine, the BMD ratio of the TS group was statistically higher than those of B group except lumbar total BMD significantly (Table 3).
We studied the outcomes of osteoporosis treatment among postmenopausal females with compression fracture using teriparatide and SERM treatments comparison with bisphosphonate using BMD. The World Health Organization 1994 recommendation for measuring BMD is via dual-energy X-ray absorptiometry, which is a gold standard for diagnosing osteoporosis and monitoring treatment results in bone strength and a determinant in fracture risk.10) Today, the treatment outcome has been measured by BMD and T-score of femur and lumbar spine, since it is supposed that BMD reflects both bone strength and fracture risk.
Several studies demonstrated 20 ug of daily subcutaneous teriparatide injection decreases vertebral fracture risk. In one of study, BMD of the lumbar spine and femur neck was determined 4, 12, and 24 months after using 21 months of teriparatide injection; then compared to those of a control group of patients under placebo.7) Teriparatide decreased the fracture risk compared to those of the placebo group. Teriparatide increased cancellous bone volume and cortical bone thickness, and improved trabecular morphology. In these data, lumbar spine BMD of the TS group was significantly higher than those of the B group.
In another study, 6 months of teriparatide use decreased pain and promoted healing of femoral fractures. In the five patients using teriparatide for 6 months, bone remodeling markers were increased.2) Our study also improved femur neck BMD ratio showing that the value 2.00±16.29 (p=0.002), but that is less than lumbar spine BMD ratio.
Teriparatide is especially effective in the elderly and in those with low initial BMD.9) Our results showed that mean age of TS group and B group was 71.65±8.74 and 69.64±9.16 as old age representative.
Another study showed vertebral fracture reduction effects persisted for at least 18 months after the end of teriparatide treatment.5) But there was no long term follow up BMD after termination of using teriparatide.
Traditionally, bisphosphonate has been the first choice for treating osteoporosis. However, recent trials show teriparatide has been effective for elderly patients with osteoporosis diagnosed compression fracture. Almost articles described that teriparatide was used during at least 6 months. But patients in the TS group used teriparatide for a mean of 3.23±1.63 months, after only oral SERM treatment. In the Korea, osteoporosis patients tend to stop teriparatide medication due to its high cost with regard to medical insurance compensation, and prefer cost effective or generic drugs. Keep this limitation, although not patients used teriparatide for long-term, we got the results that using teriparatide combination with SERM make better BMD compared to those using bisphosphonate. In this retrospective study, the TS group showed improvements in lumbar spine BMD and T-score, and increased width of the BMD ratio, compared to those of B group.
Teriparatide used in combination with SERM can reduce fracture risk, especially in the lumbar spine more so than the femur neck region. Using teriparatide and SERM can be effective in increasing BMD in postmenopausal women with compression fracture within a short time frame of treatment.
It is still important to select osteoporotic drug according to the individual patient. Patients were considered both financial cost and effectiveness to treat osteoporosis. Further long term study is needed for improvement of BMD reflects clinical good outcome included recurrent fracture. Additionally, bone turnover markers are also important evaluation factors and should be evaluated for further studied.
Comparison of TS group and B group was performed in postmenopausal women of compression fracture by BMD and in lumbar spine region, BMD ratio of TS group was comparatively higher than those of B group. In summary, the results are shown to be significantly effective increasing BMD through treatments using SERM after using teriparatide within a short period of time among menopausal women. We recommend using teriparatide combination with SERM was used postmenopausal women of compression fracture.
References
1. Chen P, Satterwhite JH, Licata AA, Lewiecki EM, Sipos AA, Misurski DM, et al. Early changes in biochemical markers of bone formation predict BMD response to teriparatide in postmenopausal women with osteoporosis. J Bone Miner Res. 2005; 20:962–970. PMID: 15883636.

2. Chiang CY, Zebaze RM, Ghasem-Zadeh A, Iuliano-Burns S, Hardidge A, Seeman E. Teriparatide improves bone quality and healing of atypical femoral fractures associated with bisphosphonate therapy. Bone. 2013; 52:360–365. PMID: 23072919.

3. Cho PG, Ji GY, Shin DA, Ha Y, Yoon DH, Kim KN. An effect comparison of teriparatide and bisphosphonate on posterior lumbar interbody fusion in patients with osteoporosis: a prospective cohort study and preliminary data. Eur Spine J. [epub ahead of print December 10, 2015]. DOI: 10.1007/s00586-015-4342-y.

4. Collinge C, Favela J. Use of teriparatide in osteoporotic fracture patients. Injury. 2016; 47(Suppl 1):S36–S38.

5. Lindsay R, Scheele WH, Neer R, Pohl G, Adami S, Mautalen C, et al. Sustained vertebral fracture risk reduction after withdrawal of teriparatide in postmenopausal women with osteoporosis. Arch Intern Med. 2004; 164:2024–2030. PMID: 15477438.

6. Marcus R, Wang O, Satterwhite J, Mitlak B. The skeletal response to teriparatide is largely independent of age, initial bone mineral density, and prevalent vertebral fractures in postmenopausal women with osteoporosis. J Bone Miner Res. 2003; 18:18–23. PMID: 12510801.

7. Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001; 344:1434–1441. PMID: 11346808.

8. Niimi R, Kono T, Nishihara A, Hasegawa M, Matsumine A, Kono T, et al. Determinants associated with bone mineral density increase in response to daily teriparatide treatment in patients with osteoporosis. Bone. 2014; 66:26–30. PMID: 24909538.

9. Obermayer-Pietsch BM, Marin F, McCloskey EV, Hadji P, Farrerons J, Boonen S, et al. Effects of two years of daily teriparatide treatment on BMD in postmenopausal women with severe osteoporosis with and without prior antiresorptive treatment. J Bone Miner Res. 2008; 23:1591–1600. PMID: 18505369.

10. Senn C, Günther B, Popp AW, Perrelet R, Hans D, Lippuner K. Comparative effects of teriparatide and ibandronate on spine bone mineral density (BMD) and microarchitecture (TBS) in postmenopausal women with osteoporosis: a 2-year open-label study. Osteoporos Int. 2014; 25:1945–1951. PMID: 24760244.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download