This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To report an observational investigation of small high attenuated foci in computed tomography (CT) scan followed by brain parenchymal catheterization.
Methods
From January 2011 to March 2015, we retrospectively reviewed the 381 patients who had undergone brain catheterization in our clinic and enrolled the patients who had newly developed high attenuation foci in the postoperative CT scans. The brain CT scans were reviewed about the lesion location, Hounsfield Unit (HU) and the time of appearance.
Results
Twenty seven of 381 patients had high attenuation foci in CT scans after the procedure. The location of high density lesions was as follows: parenchyma in 9 (33.3%) cases, ventricle in 5 (18.5%), combined in parenchyma and ventricle in 13 (48.1%). The lesions were identified in the catheter tract in parenchymal type, and catheter-lodged frontal horn or choroid plexus in ventricular type. We could not find the calcific foci before the catheter removal, and those were found after removal in all cases. The time of appearance after the removal was variable from 0 to 14 days (mean 4.2, median 3). The regular rules of HU change in CT scans were not found as times go on.
Conclusion
The high attenuation foci in CT scans were bone dust originated from skull during operation. Although these lesions did not make troubles, we should clean the operation field before the insertion of brain catheter and we may use another material, like Surgicel to seal up the burr hole instead of bone dust in the end of operation.
Go to :

Keywords: Brain, Calcinosis, Catheterization, Bone transplantation
Introduction
Brain parenchymal puncture by catheter is thought to be the most commonly used procedure in the neurosurgical field. This procedure is performed for external ventricular drainage (EVD), free-hand aspiration or stereotactic aspiration for the removal of intracerebral hemorrhage, ventriculo-peritoneal (V-P) shunt, monitoring of intracranial pressure. The main complications of these procedures are hemorrhage and infection. But the intracranial calcification is extremely rare condition as a postoperative complication and the reports about this are sparse.
124) Since some time ago we could find high-density intracranial lesions after these operations, and these high-density lesions changed in size and density with time. We analyzed the cases of high density foci in the tract of catheter or in the ventricles, which supposed the bone dust deposit after drilling of skull. And we tried to investigate the etiology and possible pathogenesis of calcification.
Go to :

Materials and Methods
From January 2011 to March 2015, we retrospectively reviewed the medical records of 381 patients who had undergone brain parenchymal catheterization in our neurosurgical clinic. All pre- and post-procedural computed tomography (CT) scans were reviewed and we enrolled 27 of 381 patients (7.1%). The enrollment criteria were the patients who had newly developed high attenuation foci in axial CT scans (5 mm slice interval) within 14 days after the removal of catheters. We examined the CT immediately after the insertion of catheter in all patients, also checked after the removal of that and reviewed the lesion location, density with Hounsfield Unit (HU) and the time of appearance. The duration of CT follow-up period was from one month to 3 years 3 months (mean 11.7 months).
All patients had the same operation room setting to diminish confounded factors, and performed burr-hole trephination rather than twist drill craniotomy in all cases. The used catheters were made by Korean Sewoon Medical (10.5 Fr, 12 Fr), Korean Yushin Medical (10.5 Fr) and Aesculap in USA (7.5 Fr). We used Aesculap's product in the V-P shunt procedure only.
We excluded patients who could have potential of calcifications (meningitis, ventriculitis) and the possibility of confusion with hemorrhage in CT exam (coagulopathic disorders, traumatic brain injury).
Go to :

Results
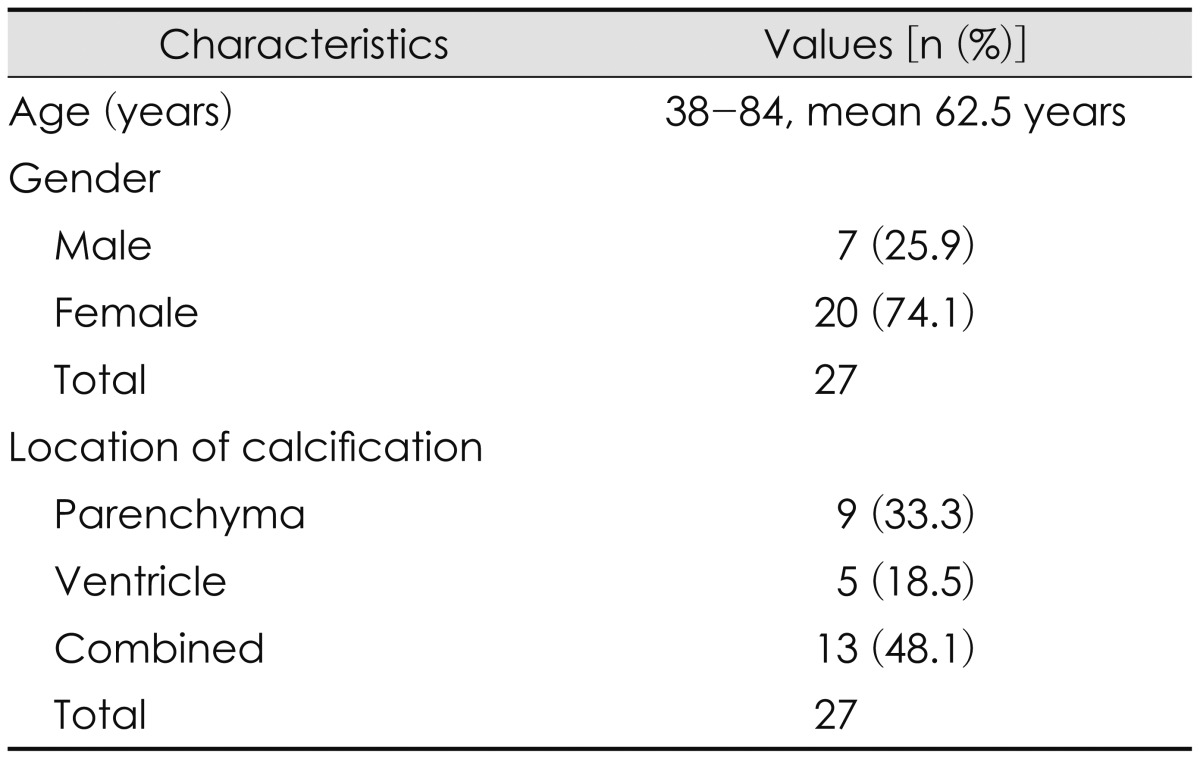
We found that 27 of 381 patients (7.1%) were shown to have high density foci in brain parenchyma and/or ventricle. The range of age distribution was from 38 to 84 (mead 62.5) years old. Among the 27 cases, 7 (25.9%) were males and 20 (74.1%) were females (
Table 1).
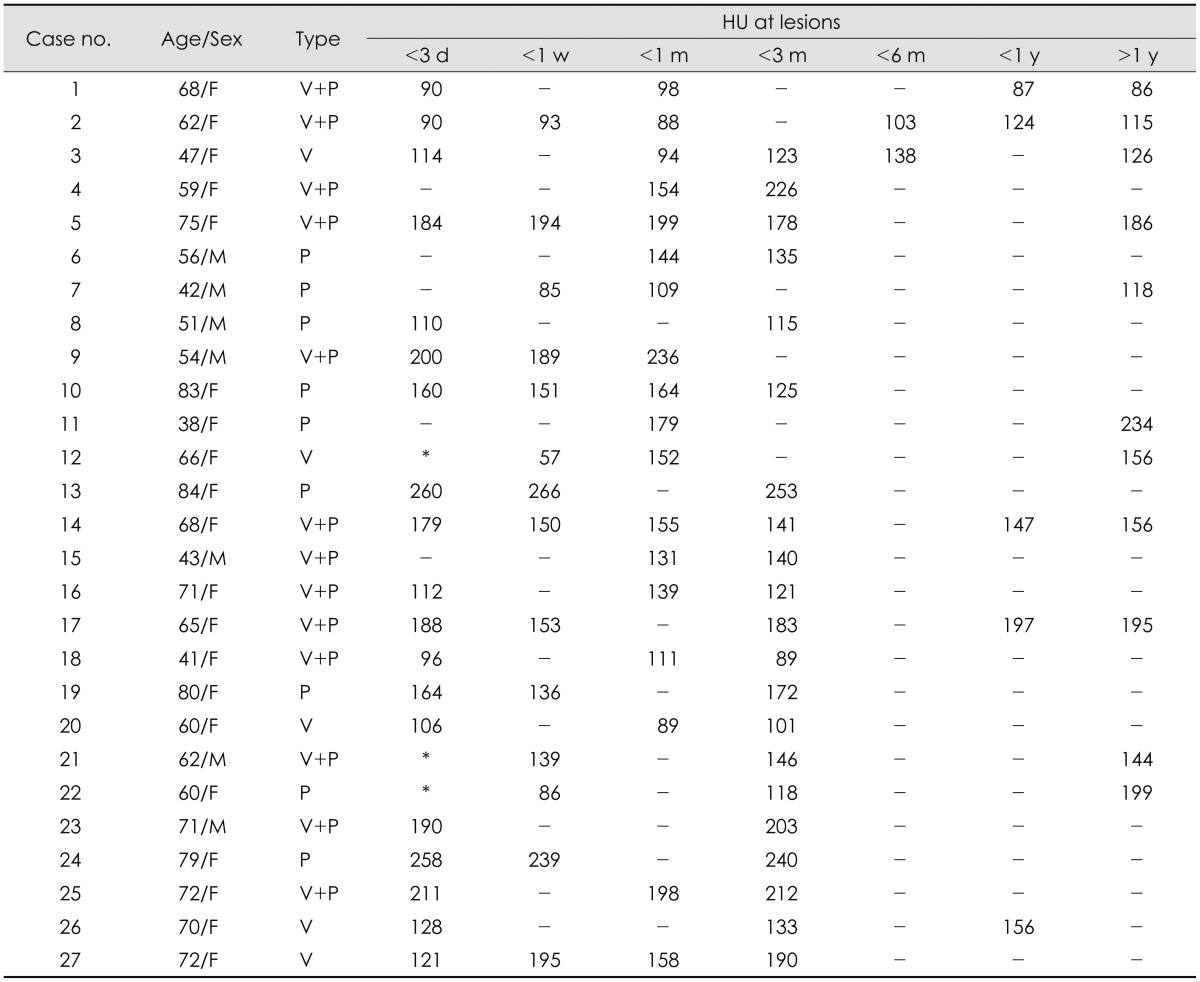
TABLE 1
Demographic and clinical characteristics of patients
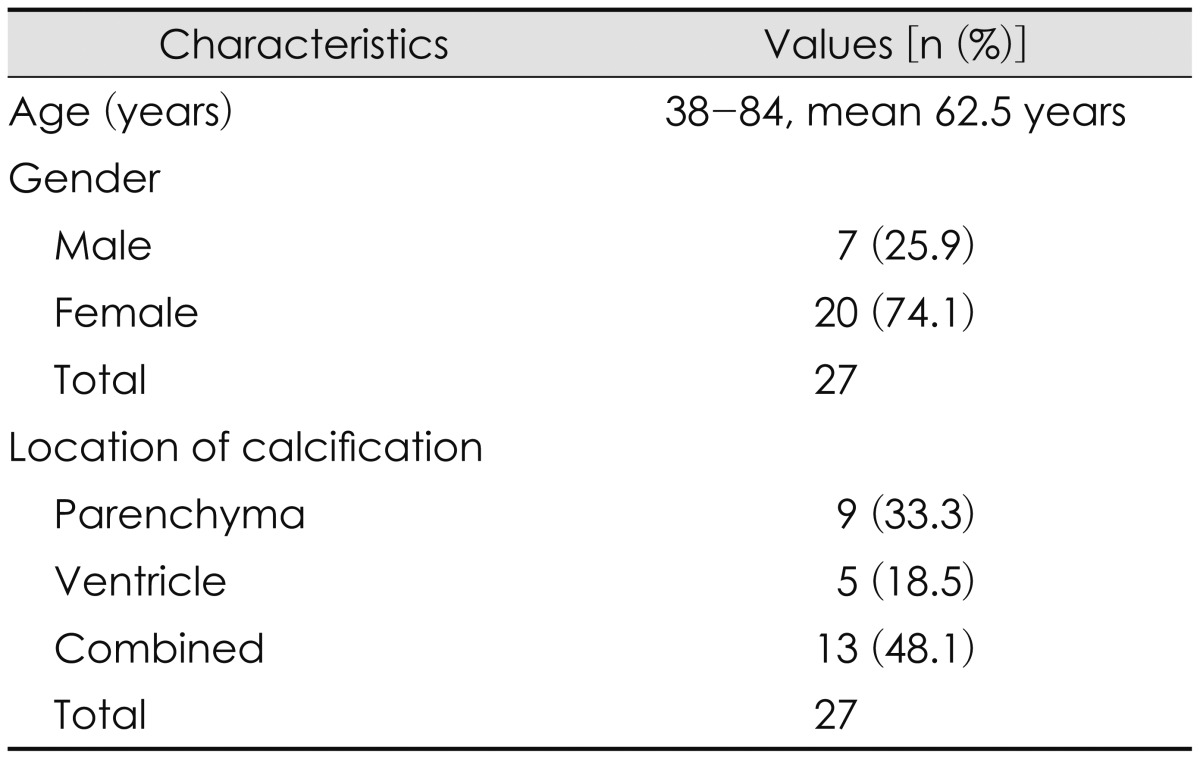

The location of calcification was as follows; parenchyma in 9 (33.3%) cases, ventricle in 5 (18.5%), combined in parenchyma and ventricle in 13 (48.1%) (
Table 1). The lesions were identified in the catheter tract in the parenchymal type, and mainly catheter-lodged frontal horn or choroid plexus in ventricular type.
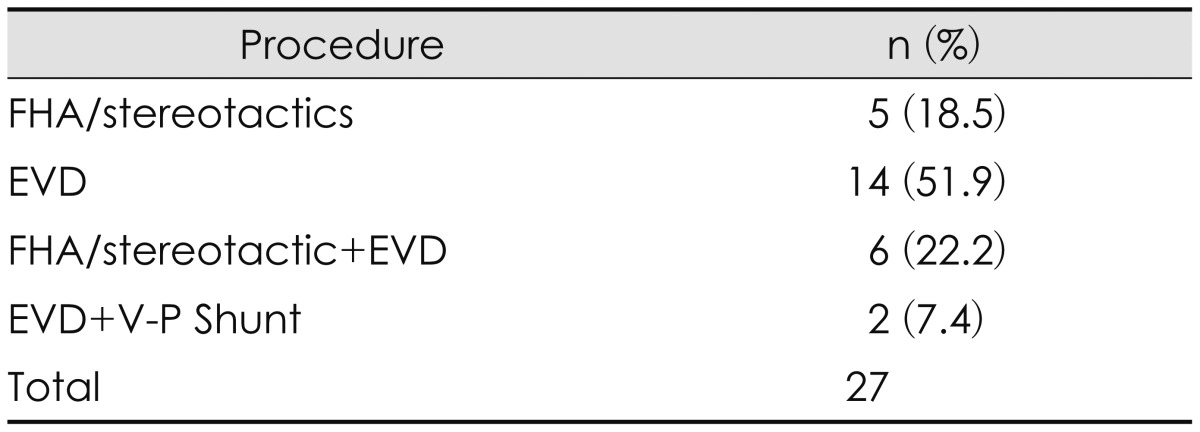
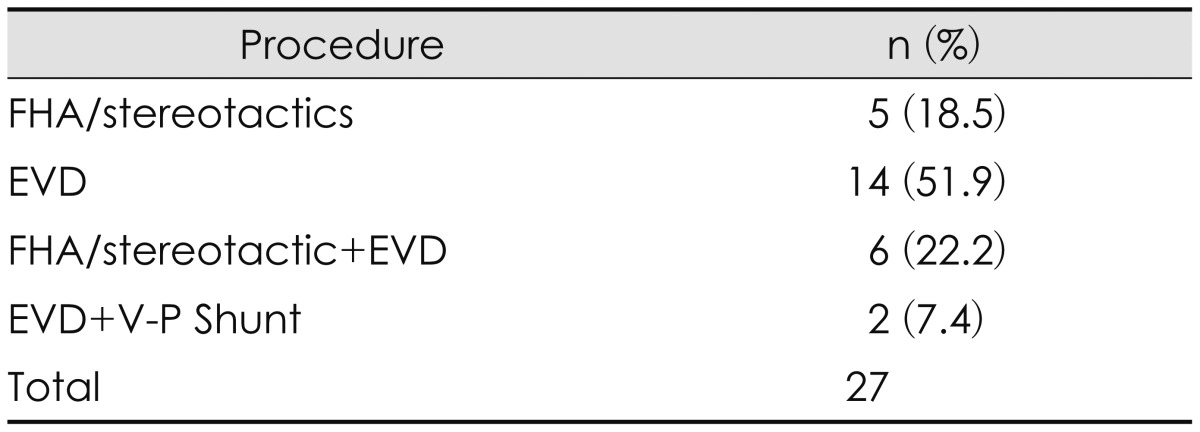
And we classified the occurrence of the lesion by operative method, i.e., free hand aspiration (FHA) or stereotactic removal of hematoma in 5 (18.5%) cases, EVD 14 (51.9%), FHA or stereotactic removal with EVD 6 (22.2%), EVD with V-P shunt 2 (7.4%) (
Table 2).
TABLE 2
Classification of procedure

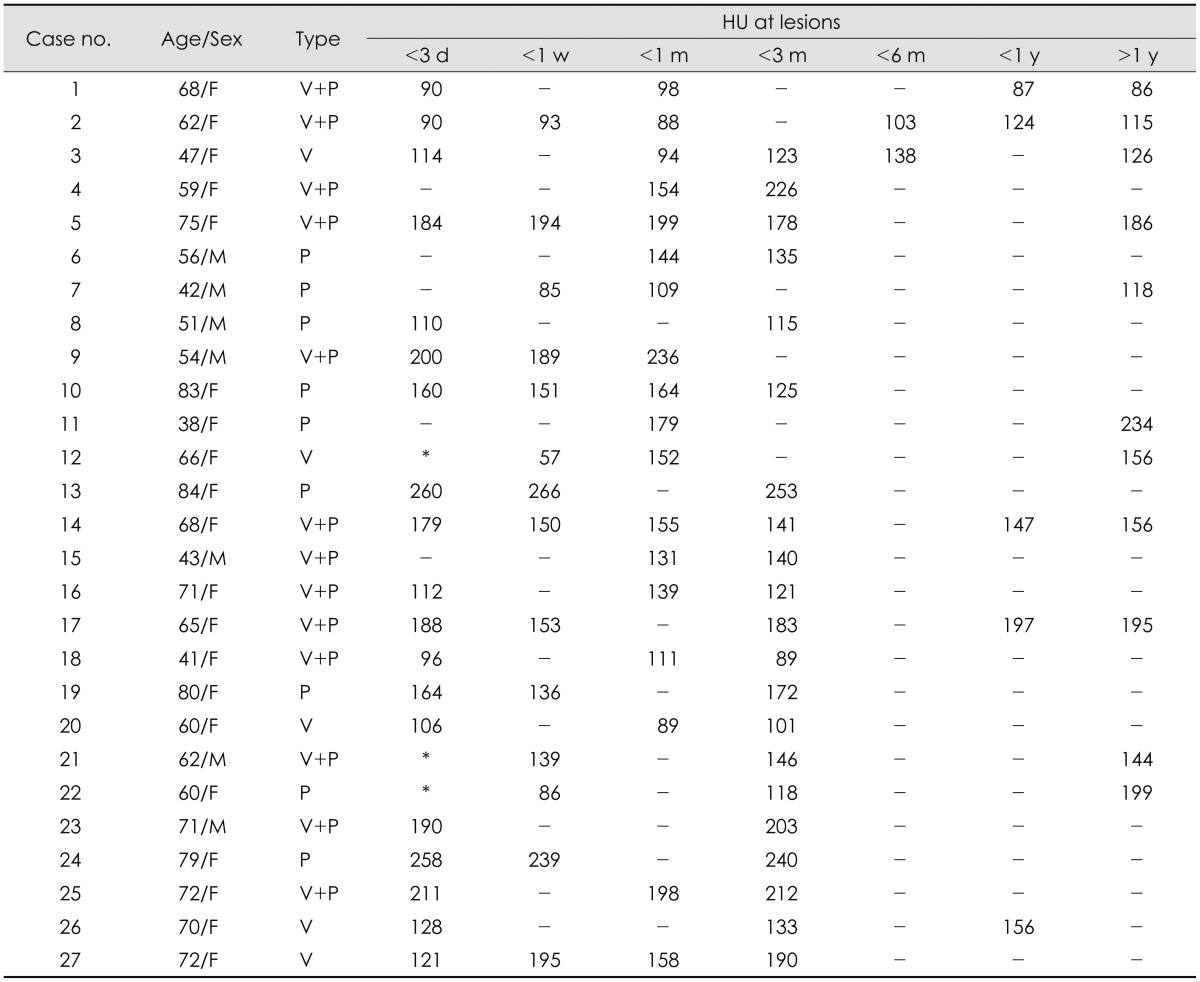
Among 27 cases there were no high-density lesions before catheter removal in serial CT scans, those were found in all cases after removal of it. The time of appearance after removal was variable from 0 to 14 days (mean 4.2, median 3). We checked chronological change pattern of HU in lesions after removal of the catheters (
Table 3). However there were not specific regular rules in the data as time flows. In some cases the increase of HU was seen within one month but not in all the cases. The size of calcification was slightly enlarged also at the early stage in a few cases only, and it maintained until the late stage without further enlargement. The patients who checked serial CT scan over one year after operation were eleven. Of these 11 patients there aren't the patients who had the increase of lesions. The ventricular high attenuation foci were identified on CT exams obtained 3 days after removal of the catheter, and maintained the same size and density on the 30 months follow-up examination (Case 3) (
Figure 1,
2,
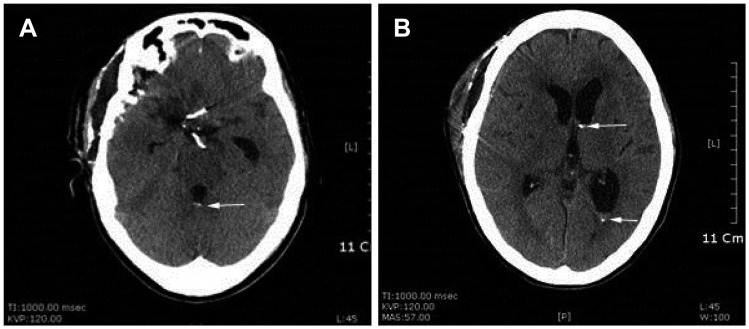
3). The patient had no clinical problems at follow-up periods. The parenchymal high-density lesions at left frontal lobe were found after removal of 2 catheters for EVD and FHA of hematoma (Case 22) (
Figure 3 and
4). The lesions were not found 3 days after catheter removal in CT scan, but 6 days after they were seen and lasted. The reason of dissimilar densities in two figures (
Figure 5) is a little different angle of orbitomeatal line of CT scout scan.
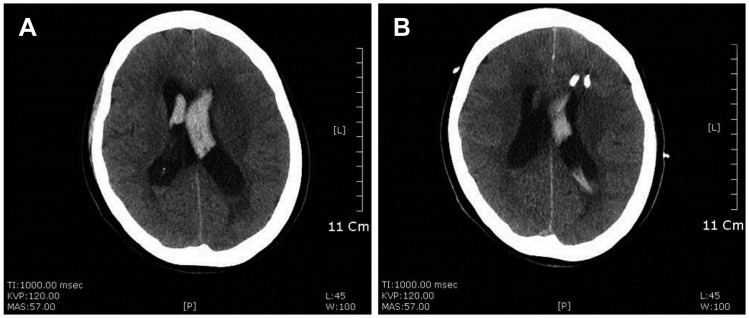
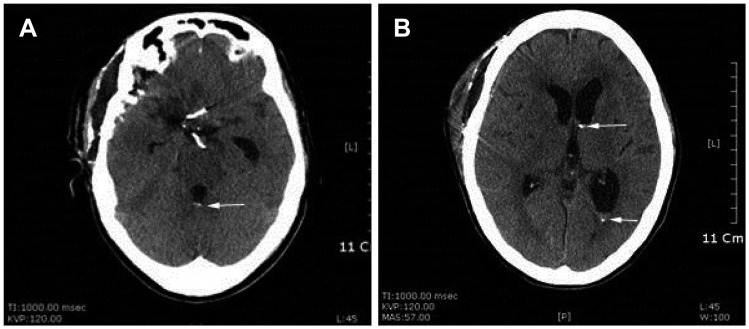
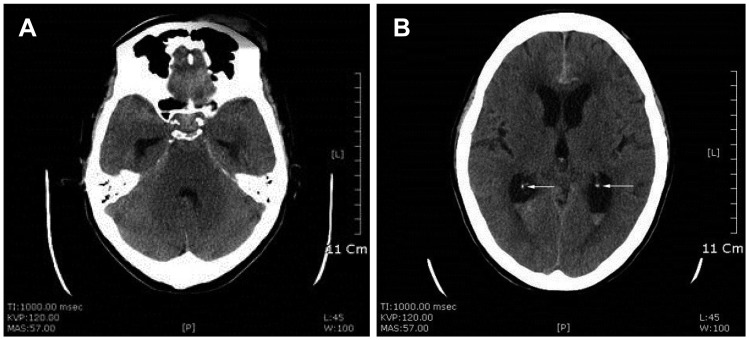 | FIGURE 1Ventricular type: (A) preoperative brain computed tomography shows aneurysmal subarachnoid hemorrhage (B) with normal calcification (white arrows) of both choroid plexus of lateral ventricle.
|
 | FIGURE 2(A) unenhanced brain computed tomography on 3 days after removal of brain catheter reveals the development of hyperdense lesions (white arrows) in the 4th ventricle and (B) the left frontal and occipital horn of the lateral ventricle. (A) two aneurysmal clips are seen at Willis' circle.
|
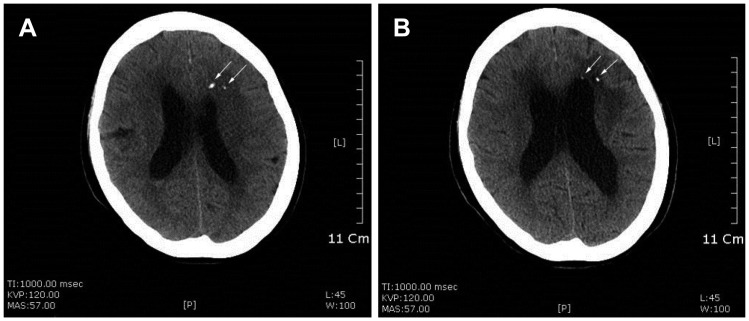
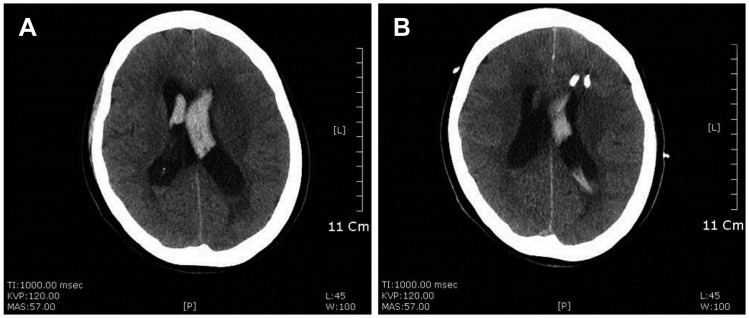
 | FIGURE 3Follow up computed tomography obtained 30 months after removal of catheter demonstrates that the calcific lesions are same in size and density (white arrows). (A) The two aneurysmal clips and (B) proximal catheter of ventriculo-peritoneal shunt are seen.
|
 | FIGURE 4Parenchymal type: (A) preoperative unenhanced brain computed tomography (CT) shows hemorrhage in both lateral ventricles, and (B) brain CT after insertion of 2 catheters.
|
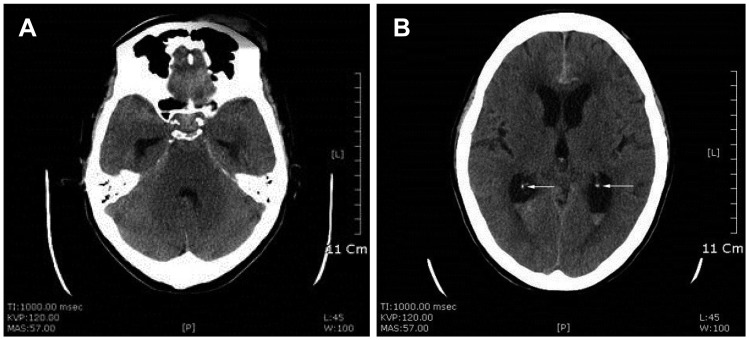
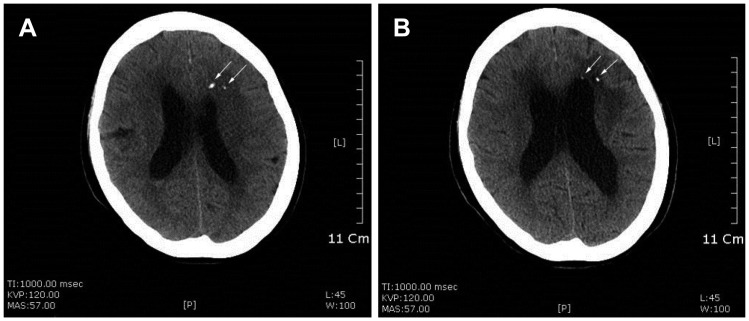
 | FIGURE 5(A) unenhanced brain computed tomography on 6 days, (B) 6 months after removal of brain catheters reveal the development of hyperdense lesions (white arrows) in the left frontal lobe.
|
TABLE 3
Chronological change pattern of the Hounsfield Units in computed tomography scan in lesions of all patients

Go to :

Discussion
The common complications of brain catheterization include hemorrhage, infection.
2) We occasionally had experienced the high density foci in CT scans after operation in few days to weeks, so we tried to observe and analyzed the brain lesion in those patients. We postulated 3 hypotheses as causes of high density lesion after the procedure.
1) Catheter origin: the catheter is made of silicon, and the inner longitudinal radiopaque band for the radiologic identification contains tungsten material which is instilled in manufacturing process. So we supposed the melt of tungsten and deposition in brain acts as a source of high attenuated foci. We experimented in our lab to investigate this hypothesis. We immersed 2 different catheters (Korean Sewoon Medical 10.5 Fr, Korean Yushin Medical 10.5 Fr) in normal saline bottles, and incubated in 36.5° chamber for 7 days. And then we scanned those bottles with CT scan, but the high density deposit was not found in these bottles. Finally we could reach a conclusion that the catheter is not a cause.
2) Calcification in a blood clot or in a small traumatized and infarcted brain tissue in the tract of the catheter.
1) Infarctions are recognized cause of brain calcification. This calcification in infarction that is recognizable on CT scan usually takes several months to appear in adults.
3) This hypothesis can't explain the finding of our patients because the high attenuation foci were seen on the examinations within 14 days maximum from removal of the catheter. This is obviously not an enough time to develop such calcifications.
3) Bone dust may play a major role in the occurrence of the lesion. This hypothesis is supported by the sudden appearance of high attenuation foci in catheter tract or in cerebrospinal fluid (CSF) path way after removal of that, and these foci were not changed in size and shape on the long-term follow-up examinations.
The neurosurgeon usually perform twist drill craniotomy or formation of burr-hole using electrical perforator for drainage catheter insertion, the authors prefer to make the burr-hole because the direct visualization of dura is good. In the process of craniotomy powdered bone from skull could be produced more in burr hole craniotomy than in twist drill craniotomy. So the bone dust had a more chance to put into the brain through the catheter tract after catheter insertion or removal without perfect irrigation and cleansing in burr hole craniotomy. Some surgeons may fill with bone dust to seal up the burr hole after insertion of catheter in the end of operation.
From the point of a pathogenetic view the bone dust could be pushed deep by the catheter and arrested in the parenchyma or ventricle.
1) And we considered the appearance of high attenuation foci after removal of catheter in 2 points of view. In cases of ventricular puncture, bone dust floating the CSF-filled tract which formed for a while after withdrawal of catheter, and sink slowly in ventricle later. In cases of parenchymal puncture, the powdered bone could deposit immediately in the tract which is filled with little CSF. In our clinic four surgeons were operated and seal the burr hole with bone dust after insertion of catheter case by case according to their preference.
We had followed up the patients with serial CT scans and observed the findings. At the early time after the removal of catheter the density of calcific lesion was not so very high, however as time went on it became gradually strong high with/without enlargement of calcification in a few days. But it was not changed in size and density for a long time follow-up. There were eleven patients who checked follow-up CT scans over one year after operation, no case had developed an enlarged calcification among them. We can explain this phenomenon that floating bone dust sink slowly as time passed. The more an amount of dust is large, the shorter appearance date of calcification may be and the higher enlargement speed also may be in early stage. We observed the chronological change pattern of HU in all cases (
Table 3). In the cases of relatively high HU, the volume of dust was slightly larger than the low HU cases. The HU scale was increased in some cases at the early stage (within 1 month) but it didn't find out at the other cases (case 1, 5, 7, 12, 16, and 18). We couldn't observe the regular rules in those data as time progress. We had several difficulties determining the HU in CT images. First, the HU scale had different values due to the slight differences in the level of axial section images in the follow-up exams. Second, as there were small multiple calcifications in many cases, we calculated them using mean values. Lastly there were differences in the time interval of first CT scan between the patients after the catheter removal. As a result, we had difficulties in analyzing the results.
There are not any complications associated with these calcifications. But there is an article that progressive hypertrophic calcification formed following ventricular endoscopy.
4) Thomson et al.
4) experienced 2 cases of enlargement within 1 year after operation. Bone dust contains viable osteoblasts that when implanted into vascular tissues are capable of dividing and laying down bone, and this is the theoretical basis of sealing burr hole with powdered bone in our operation. They suppose that bone dust got into the highly vascularized choroid plexus, it could form viable, progressive hypertrophic calcification in enlarged cases.
Our study had a limitation that the serial check time of CT scan after removal of catheter r was different from patients to patients because the condition of the patients was variable. So the prospective study can precisely measure the appearance time of calcification in CT scan after procedure.
Go to :

Conclusion
The high attenuation foci in CT scans may be from the bone dust originated during operation. The skill, technique and the habit of surgeon used have a major role to play in forming calcification. Although these lesions did not make troubles, we should clean the operation field before the insertion of brain catheter and we may use another material, like Surgicel to seal up the burr hole instead of bone dust in the end of operation.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download