This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
This study was aimed at finding out the changes in cognitive dysfunction in patients with traumatic brain injury (TBI) and investigating the factors limiting their cognitive improvement.
Methods
Between January 2010 and March 2014, 33 patients with TBI participated in serial mini-mental status examination (MMSE). Their cognitive functions were statistically analyzed to clarify their relationship with different TBI status. Patients who developed hydrocephalus were separately analyzed in regards to their cognitive function depending on the placement of ventriculoperitoneal shunt (VPS).
Results
Bi-frontal lobe injury (β=-10.441, p<0.001), contre-coup injury (β=-6.592, p=0.007), severe parenchymal injury (β=-7.210, p=0.012), temporal lobe injury (β=-5.524, p=0.027), and dominant hemisphere injury (β=-5.388, p=0.037) significantly lowered the final MMSE scores. The risk of down-grade in the prognosis was higher in severe parenchymal injury [odds ratio (OR)=13.41, 95% confidence interval (CI)=1.31-136.78], temporal lobe injury (OR=12.3, 95% CI=2.07-73.08), dominant hemisphere injury (OR=8.19, 95% CI=1.43-46.78), and bi-frontal lobe injury (OR=7.52, 95% CI=1.31-43.11). In the 11 post-traumatic hydrocephalus patients who underwent VPS, the final MMSE scores (17.7±6.8) substantially increased from the initial MMSE scores (11.2±8.6).
Conclusion
Presence of bi-frontal lobe injury, temporal lobe injury, dominant hemisphere injury, and contre-coup injury and severe parenchymal injury adversely influenced the final MMSE scores. They can be concluded to be poor prognostic factors in terms of cognitive function in TBI patients. Development of hydrocephalus aggravates cognitive impairment with unpredictable time of onset. Thus, close observation and routine image follow-up are mandatory for early detection and surgical intervention for hydrocephalus.
Go to :

Keywords: Brain injuries, Cognition disorders, Mini-mental status examination, Neuropsychological tests
Introduction
With constant increment in the geriatric population, efforts in preserving cognitive function after head trauma have been an issue in the neurosurgical field. Compared with foreign countries, studies on the trend of the neurocognitive function in patients with traumatic brain injury (TBI) and appropriate means of evaluating cognitive functions in these patients have been limited in Korea. The mini-mental status examination (MMSE) was originally developed to evaluate patients with mild cognitive impairment, especially in the elderly patients as a screening study for Alzheimer's dementia.
1) In the present study, the authors have applied the Korean version of the MMSE questionnaire as a measuring instrument of cognitive function in patients with TBI. Serial tests were repeated over given time, and the data was generated to find out the relationship between various forms of TBI and the severity of cognitive impairment.
Go to :

Materials and Methods
Patient population
During January 2010 and March 2014, 218 TBI patients admitted in Konkuk University Medical Center with various vectors and severity were requested to participate in serial MMSE tests. Selection criteria included ages 18 years and older, medically able to participate in cognitive testing, participation in serial tests of twice or more, and patients without prior disease or injury of the brain that may have influenced the test results. One hundred and fifty-two patients who did not participate in serial MMSE and 18 patients whose Glasgow Coma Scale never scored above 12 for at least once during admission were excluded from the study group. One patient whose cognitive function and mental status deteriorated due to fulminant infection, one with re-bleeding after surgery for a traumatic intracerebral hematoma, and another who was re-admitted due to repeated trauma were also omitted. Eight patients with history of cerebral infarction, one patient with history of hypertensive intracerebral hematoma, and another with history of Alzheimer's dementia were also excluded. In addition, two patients whose initial and final MMSE intervals were less than a month were excluded from the study group. In total, 33 patients were enrolled in this study.
Clinico-radiologic data
The clinico-radiologic data of all patients were retrospectively reviewed to gather information on the patients' age, sex, radiologic findings, neurological status, location, type and extent of brain injury, development of hydrocephalus and placement of ventriculoperitoneal shunt (VPS), and their serial MMSE scores. Initial and following computed tomography (CT) scan results were referred to in determining the brain injury status. The brain injury status was categorized as followed: parenchymal injury; parenchymal injury extent (number of lobes involved); posterior fossa injury; brain-stem injury; contre-coup injury; contre-coup injury extent (number of lobes involved); temporal lobe injury; dominant hemisphere injury; bi-frontal lobe injury. Changes in MMSE scores in these patients were recorded and statistically analyzed to find out the effect of these factors on the MMSE scores.
The MMSE scores were classified into three groups to describe the severity of cognitive impairment as proposed by Lopez et al.;
5) any score greater than or equal to 24 were presumed to be normal in cognition, between 18 and 23 to be mildly impaired, and less than 18 to be severely impaired. Changes in these groups based on the initial and final MMSE scores were noted, and they were categorized under "Normal", "Improved", "Worsened", and "No change" groups. The patients who had no cognitive impairment throughout the study period were grouped as "Normal". Those who showed any degree of improvement in the final MMSE results were grouped as "Improved". Those who ended up with deteriorated cognitive function were grouped as "Worsened". Finally, those who remained stationary as mild or severe impairment throughout the study period were grouped as "No change".
The prognoses in cognitive function were decided according to these four groups; the "Normal" and "Improved" groups were said to have a good prognosis, and the "Worsened" and the "No change" groups were said to have a poor prognosis. Their associations in regards to each TBI state were statically analyzed to investigate the poor prognostic factors of cognitive function in patients with TBI.
Delayed hydrocephalus after TBI and the placement of VPS were also examined for significance as predictors of cognitive outcome.
Statistical analysis
For determining possible factors in association with cognitive function in the patients with TBI, repeated measure analyses were used to investigate the association between each injury status and change in MMSE score (linear mixed model analysis). Multivariate logistic regression was also used to find any significant relationship between the each injury status and prognosis of cognitive function. Age, sex, time since symptom onset (in days), and time at which MMSE tests were taken (initial/final) were adjusted for repeated analyses, while age and sex were adjusted for logistic regression. All analyses were tested at the p<0.05 level of significance, and PROC MIXED and PROC LOGISTIC statements from SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA) were used for the association analyses.
Go to :

Results
The study population was composed of 33 subjects and the median age was 65 years (range, 18 to 92). The median interval from the trauma to the initial MMSE was 45 days (range, 0 to 419) and the median interval from the trauma to the final MMSE was 177 days (range, 37 to 1027). In overall, the mean initial and final MMSE scores were 12.0±9.9 and 16.4±9.4, respectively.
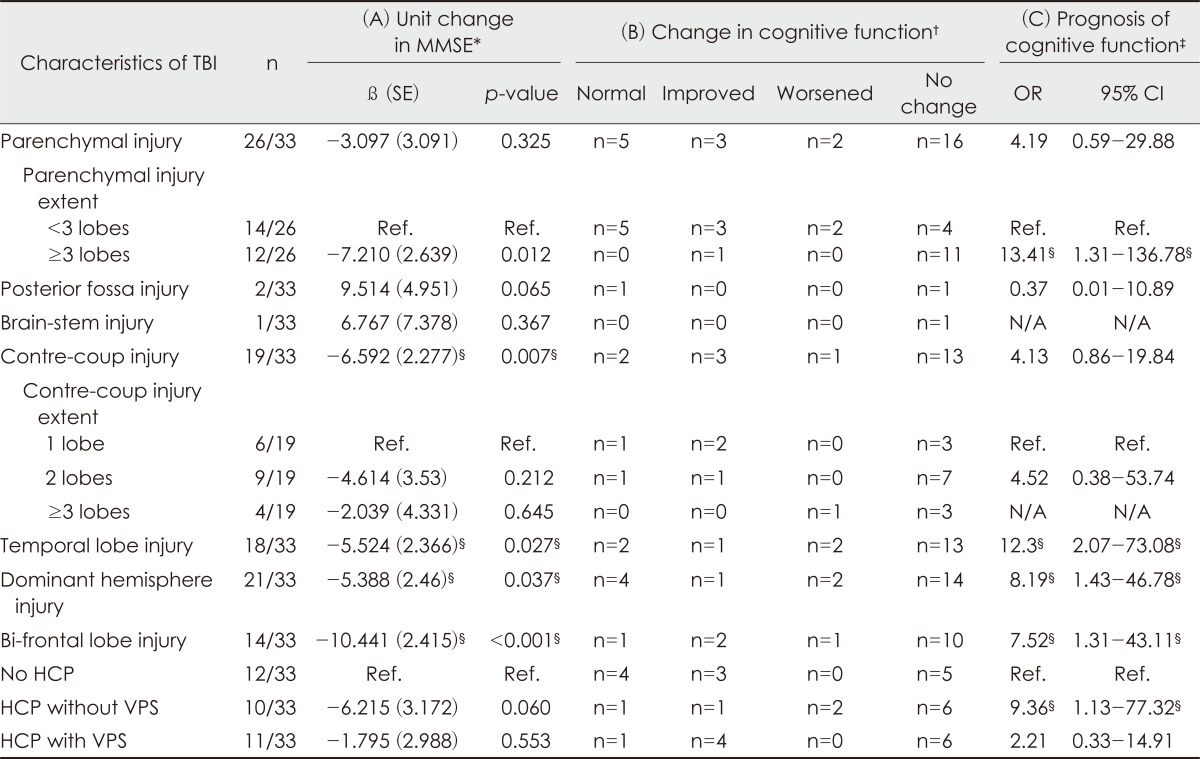
The TBI status and their relationship with the cognitive function are shown in
Table 1. Presence of bi-frontal lobe injury (β=-10.441,
p<0.001), contre-coup injury (β=-6.592,
p=0.007), dominant hemisphere injury (β=-5.388,
p=0.037) and temporal lobe injury (β=-5.524,
p=0.027) significantly lowered average MMSE scores compared to those without such lesions. Presence of parenchymal injury itself did not have a significant relationship but severe parenchymal injury (defined by ≥3 injured lobes) significantly lowered MMSE scores (β=-7.210,
p=0.012). On the other hand, the extent of contre-coup injury did not have any significant relationship with the MMSE scores.
TABLE 1
Relationship between characteristics of traumatic brain injury and mini-mental status examination results
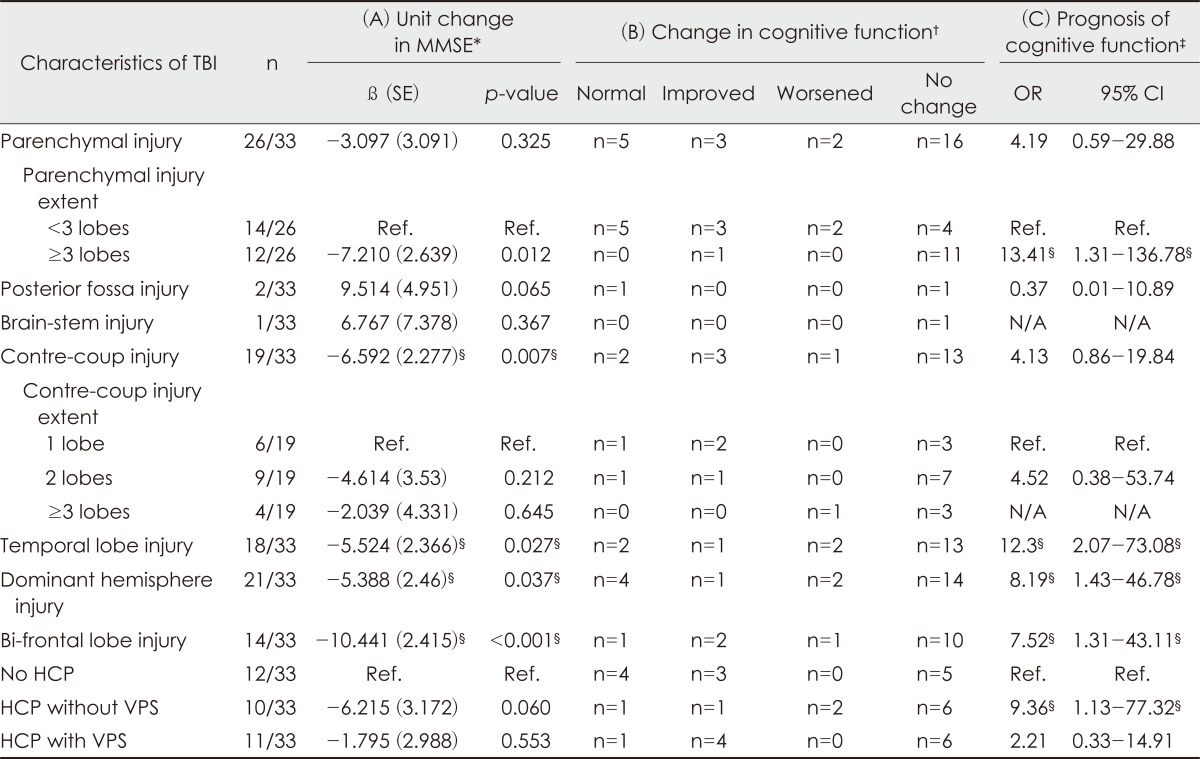

In regards to the prognosis in cognitive function, severe parenchymal injury [odds ratio (OR)=13.41, 95% confidence interval (CI)=1.31 to 136.78], temporal lobe injury (OR=12.3, 95% CI=2.07 to 73.08), dominant hemisphere injury (OR=8.19, 95% CI=1.43 to 46.78), and bi-frontal lobe injury (OR=7.52, 95% CI=1.31 to 43.11) had higher risk of down-grade in cognitive function.
Hydrocephalus
In our study population, hydrocephalus developed in 21 patients (63.6%), and 11 of these patients (33.3%) underwent VPS. Among the other ten patients without VPS, eight patients had ventriculomegaly without definite symptoms of hydrocephalus. One patient showed no definite improvement in symptom after diagnostic cerebrospinal fluid drainage. In one patient, VPS was recommended but the patient was reluctant to surgery.
Hydrocephalus without VPS resulted in decreased MMSE scores with borderline significance (β=-6.215,
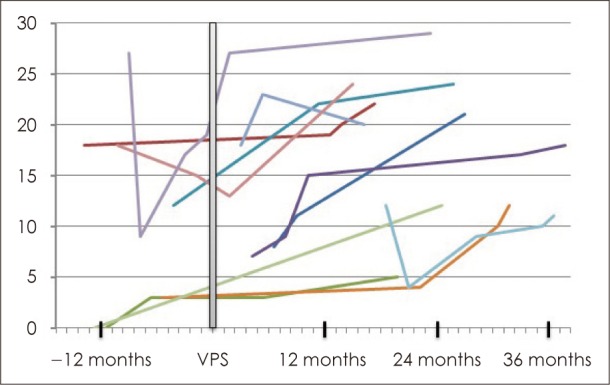
p=0.060) and increased risk of down-grade in the prognosis (OR=9.36, 95% CI=1.13 to 77.32). In the patients who underwent VPS, mean MMSE score before VPS was 11.2±8.6, whereas mean final MMSE score after VPS was 17.7±6.8. However, no statistical significance could be seen in this group of patients. The association analyses of the hydrocephalus patients are summarized in
Table 1, and the trend in their MMSE scores associated with VPS is depicted in
Figure 1.
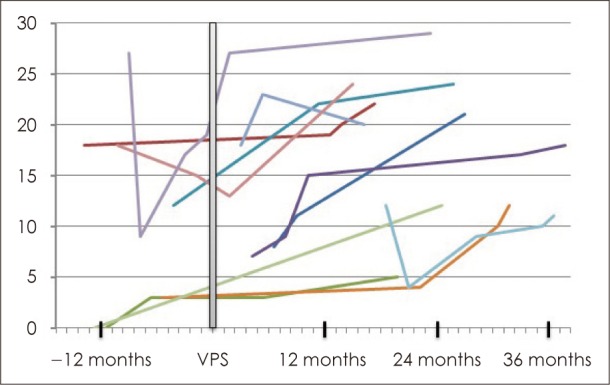 | FIGURE 1Trend in mini-mental status examination (MMSE) before and after ventriculoperitoneal shunt (VPS) in patients with post-traumatic hydrocephalus. Graph shows serial MMSE scores of 11 patients with post-traumatic hydrocephalus who underwent VPS. The average initial score was 11.2±8.6, and the average final score was 17.7±6.8. x-axis: time in regards to VPS, y-axis: MMSE score.
|
Go to :

Discussion
The objective of this study was to validate the trends in cognitive function in regards to different brain injury status in patients with TBI, and hence to determine the predictors of cognitive outcome in these patients.
The main finding of this study is that the presence of bi-frontal lobe injury, severe parenchymal injury, contre-coup injury, temporal lobe injury, and dominant hemisphere injury had negative effects in the cognitive outcome in patients with TBI.
Damage to prefrontal cortex disrupts a variety of cognitive functions, including planning, problem solving, and temporal organization. Although patients with frontal lobe injury are not amnesic, impairment on certain tests of memory have been perceived.
3) Studies have shown strong evidence that frontal damage disrupts performance on the test of recognition, cued recall, and free recall.
6,
9) In our study, patients with extensive bi-frontal lobe injury have displayed the highest risk of cognitive impairment with the greatest fall in the MMSE score, thereby verifying the role of frontal lobes in cognitive function.
There is little doubt that the temporal lobe plays a significant role in both retrograde and anterograde memory as it is well-known for its function in memory storage, language recognition and processing of audiovisual sensory input. The role of medial temporal lobes and hippocampus as memory center has been widely described, and researches have shown that focal lesions in the hippocampus result in limited impairment of memory function, whereas extensive lesions that include the hippocampus and the medial temporal cortex result in severe impairment.
47)
Presence of contre-coup injury may be described in correlation with the above two factors. Due to the rough internal surface of the anterior and middle cranial fossa, frontal and temporal lobes are the sites most prone to contre-coup injuries.
2) In fact, 15 out of 18 temporal lobe injury patients (83.3%) and 13 out of 14 bi-frontal lobe injury patients (92.9%) had contre-coup injury in our study. Moreover, the presence of contre-coup injury may implicate a high inertial force. The larger average number of lobes involved (n=3.2) and the higher proportion of initial decompressive surgery in patients with contre-coup injury (14/19=73.7%) compared to that of patients without contre-coup injury (n=0.9, 5/14=35.7%) in our study support this presumption. In addition, our study showed that patients with contre-coup injury had a worse prognosis in cognitive outcome than patients without contre-coup injury (
p=0.007). Contre-coup injuries which are closely related with severity and fronto-temporal location of TBI seem to be a major prognostic factor in the cognitive function.
The incidence of post-traumatic hydrocephalus varies widely in the literature from 30% to 86% of patients examined within one year after moderate to severe head trauma.
8) Due to a wide range in the timing of occurrence, development of the pathognomonic symptoms such as memory impairment, gait disturbance and urinary incontinence has to be closely monitored for early diagnosis and appropriate treatment. Unfortunately, as much of the patients with TBI eventually transfer out to rehabilitation department or local rehabilitation centers for chronic phase management, development of these symptoms and radiologic work-up could often be missed out. Although improvement of cognitive function following VPS could not be statistically validated in this study due to limited sample size, substantial increment in the mean final MMSE score after VPS (from 11.2±8.6 to 17.7±6.8) implies that there have been improvements in the cognitive function in these patients to some extent. Moreover, the role of VPS in reversal of neurologic deterioration caused by hydrocephalus has been well-documented and there seems to be no question against it unless when contraindicated. Therefore, close monitoring of symptoms, routine screening image studies, and appropriate surgical management such as VPS are essential in the TBI patients prone to post-traumatic hydrocephalus.
The results of this study seem to be unique and meaningful. Firstly, we determined some radiologic risk factors affecting cognitive outcome using the MMSE which is a reliable and standardized tool in evaluation for cognitive functions. Secondly, our study showed dynamic changes of cognitive function according to delayed hydrocephalus after TBI and the placement of VPS. Lastly, our study involved consecutive patients with TBI of variable severity to minimize selection bias. Most of previous articles about cognitive dysfunction after TBI had limited study group to patients with mild to moderate TBI. But our study enrolled all patients who could conduct the MMSE and analyzed the recovery of cognition over time according to different traumatic modes. However, the inclusion of patients with severe TBI inevitably led to a timing discrepancy in terms of time interval from the trauma to the MMSE, because comatose or medically ill patients conducted the MMSE after the recovery of consciousness or medical condition. Our study had additional limitations such as a small sample size, a lack of consideration for surgical decompression, and no consideration for learning effect from repeated MMSE.
Despite aforementioned limitations, we believe that this study could be used as preliminary data for future prospective studies about cognitive outcome in patients with TBI.
Go to :

Conclusion
Bi-frontal lobe injury, temporal lobe injury, dominant hemisphere injury, and contre-coup injury significantly lowered the MMSE scores. The extent of parenchymal injury also had an indirect relationship with the MMSE scores. Moreover, these injuries also displayed higher risks of down-grade in the prognoses of cognitive function. Because development of hydrocephalus adds to cognitive impairment with unpredictable time of onset, close monitoring and routine image studies are needed for early detection and surgical intervention.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download