1. Aarabi B. Surgical outcome in 435 patients who sustained missile head wounds during the Iran-Iraq War. Neurosurgery. 1990; 27:692–695. discussion 695PMID:
2259397.

2. Alvis Miranda H, Castellar-Leones SM, Moscote-Salazar LR. Decompressive craniectomy and traumatic brain injury: a review. Bull Emerg Trauma. 2013; 1:60–68.
3. Ambrosi PB, Valença MM, Azevedo-Filho H. Prognostic factors in civilian gunshot wounds to the head: a series of 110 surgical patients and brief literature review. Neurosurg Rev. 2012; 35:429–435. discussion 435-436PMID:
22415660.

4. Arendall RE, Meirowsky AM. Air sinus wounds: an analysis of 163 consecutive cases incurred in the Korean War, 1950-1952. Neurosurgery. 1983; 13:377–380. PMID:
6633830.

5. Bakay L. Missile injuries of brain. N Y State J Med. 1982; 82:313–319. PMID:
6953335.
6. Barach E, Tomlanovich M, Nowak R. Ballistics: a pathophysiologic examination of the wounding mechanisms of firearms: Part I. J Trauma. 1986; 26:225–235. PMID:
3951001.

7. Bayston R, de Louvois J, Brown EM, Johnston RA, Lees P, Pople IK. Use of antibiotics in penetrating craniocerebral injuries. "Infection in Neurosurgery" Working Party of British Society for Antimicrobial Chemotherapy. Lancet. 2000; 355:1813–1817. PMID:
10832851.
8. Becker DP, Miller JD, Ward JD, Greenberg RP, Young HF, Sakalas R. The outcome from severe head injury with early diagnosis and intensive management. J Neurosurg. 1977; 47:491–502. PMID:
903803.

9. Carey ME. Experimental missile wounding of the brain. Neurosurg Clin N Am. 1995; 6:629–642. PMID:
8527907.

10. Carey ME, Young H, Mathis JL, Forsythe J. A bacteriological study of craniocerebral missile wounds from Vietnam. J Neurosurg. 1971; 34:145–154. PMID:
14768680.

11. Cavaliere R, Cavenago L, Siccardi D, Viale GL. Gunshot wounds of the brain in civilians. Acta Neurochir (Wien). 1988; 94:133–136. PMID:
3213631.

12. Clark WC, Muhlbauer MS, Watridge CB, Ray MW. Analysis of 76 civilian craniocerebral gunshot wounds. J Neurosurg. 1986; 65:9–14. PMID:
3712033.

13. Coşar A, Gönül E, Kurt E, Gönül M, Taşar M, Yetişer S. Craniocerebral gunshot wounds: results of less aggressive surgery and complications. Minim Invasive Neurosurg. 2005; 48:113–118. PMID:
15906207.

14. Cushing H. Notes on penetrating wounds of the brain. Br Med J. 1918; 1:221–226. PMID:
20768944.

15. Diaz-Daza O, Arraiza FJ, Barkley JM, Whigham CJ. Endovascular therapy of traumatic vascular lesions of the head and neck. Cardiovasc Intervent Radiol. 2003; 26:213–221. PMID:
14562967.

16. Ecklund JM, Sioutos P. Prognosis for gunshot wounds to the head. World Neurosurg. 2014; 82:27–29. PMID:
23924962.

17. Esposito DP, Walker JB. Contemporary management of penetrating brain injury. Neurosurg Q. 2009; 19:249–254.

18. Fackler ML, Malinowski JA. The wound profile: a visual method for quantifying gunshot wound components. J Trauma. 1985; 25:522–529. PMID:
4009751.
19. George ED, Dagi TF. Military penetrating craniocerebral injuries. Applications to civilian triage and management. Neurosurg Clin N Am. 1995; 6:753–759. PMID:
8527916.

20. Gervaise A, Foscolo S, Rivierre A, Derelle A, Schmitt E, Braun M, et al. [Imaging of cranial gunshot traumas]. J Radiol. 2010; 91:1113–1120. PMID:
21178874.
21. Gönül E, Baysefer A, Kahraman S, Ciklatekerlioğlu O, Gezen F, Yayla O, et al. Causes of infections and management results in penetrating craniocerebral injuries. Neurosurg Rev. 1997; 20:177–181. PMID:
9297719.

22. Grahm TW, Williams FC Jr, Harrington T, Spetzler RF. Civilian gunshot wounds to the head: a prospective study. Neurosurgery. 1990; 27:696–700. discussion 700PMID:
2259398.

23. Hachemi M, Jourdan C, Di Roio C, Turjman F, Ricci-Franchi A, Mottolese C, et al. Delayed rupture of traumatic aneurysm after civilian craniocerebral gunshot injury in children. Childs Nerv Syst. 2007; 23:283–287. PMID:
17119977.

24. Hadas N, Schiffer J, Rogev M, Shperber Y. Tangential low-velocity missile wound of the head with acute subdural hematoma: case report. J Trauma. 1990; 30:358–359. PMID:
2313761.

25. Hagan RE. Early complications following penetrating wounds of the brain. J Neurosurg. 1971; 34:132–141. PMID:
14768678.

26. Hammon WM, Kempe LG. Methyl methacrylate cranioplasty. 13 years experience with 417 patients. Acta Neurochir (Wien). 1971; 25:69–77. PMID:
5135756.
27. Harvey EN, McMillen JH. An Experimental Study of Shock Waves Resulting from the Impact of High Velocity Missiles on Animal Tissues. J Exp Med. 1947; 85:321–328. PMID:
19871617.

28. Hofbauer M, Kdolsky R, Figl M, Grünauer J, Aldrian S, Ostermann RC, et al. Predictive factors influencing the outcome after gunshot injuries to the head-a retrospective cohort study. J Trauma. 2010; 69:770–775. PMID:
20173654.

29. Hollerman JJ, Fackler ML, Coldwell DM, Ben-Menachem Y. Gunshot wounds: 2. Radiology. AJR Am J Roentgenol. 1990; 155:691–702. PMID:
2119096.

30. Horowitz MB, Kopitnik TA, Landreneau F, Ramnani DM, Rushing EJ, George E, et al. Multidisciplinary approach to traumatic intracranial aneurysms secondary to shotgun and handgun wounds. Surg Neurol. 1999; 51:31–41. discussion 41-42PMID:
9952121.

31. Jimenez CM, Polo J, España JA. Risk factors for intracranial infection secondary to penetrating craniocerebral gunshot wounds in civilian practice. World Neurosurg. 2013; 79:749–755. PMID:
22722035.

32. Joseph B, Aziz H, Pandit V, Kulvatunyou N, O'Keeffe T, Wynne J, et al. Improving survival rates after civilian gunshot wounds to the brain. J Am Coll Surg. 2014; 218:58–65. PMID:
24055384.

33. Joseph B, Aziz H, Sadoun M, Kulvatunyou N, Pandit V, Tang A, et al. Fatal gunshot wound to the head: the impact of aggressive management. Am J Surg. 2014; 207:89–94. PMID:
24119889.

34. Kaufman HH. Civilian gunshot wounds to the head. Neurosurgery. 1993; 32:962–964. discussion 964PMID:
8327099.

35. Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011; 4:395–402. PMID:
21887033.

36. Khan MB, Kumar R, Irfan FB, Irfan AB, Bari ME. Civilian craniocerebral gunshot injuries in a developing country: presentation, injury characteristics, prognostic indicators, and complications. World Neurosurg. 2014; 82:14–19. PMID:
23313238.

37. Kim TW, Lee JK, Moon KS, Kwak HJ, Joo SP, Kim JH, et al. Penetrating gunshot injuries to the brain. J Trauma. 2007; 62:1446–1451. PMID:
17563664.

38. Knightly JJ, Pulliam MW. Military head injuries. In : Narayan RK, Wilberger JE, Povlishock JT, editors. Neurotrauma. New York: McGraw-Hill;1996. p. 891–902.
39. Kubal WS. Updated imaging of traumatic brain injury. Radiol Clin North Am. 2012; 50:15–41. PMID:
22099485.

40. Levy ML, Masri LS, Lavine S, Apuzzo ML. Outcome prediction after penetrating craniocerebral injury in a civilian population: aggressive surgical management in patients with admission Glasgow Coma Scale scores of 3, 4, or 5. Neurosurgery. 1994; 35:77–84. discussion 84-85PMID:
7936156.
41. Liebenberg WA, Demetriades AK, Hankins M, Hardwidge C, Hartzenberg BH. Penetrating civilian craniocerebral gunshot wounds: a protocol of delayed surgery. Neurosurgery. 2005; 57:293–299. discussion 293-299PMID:
16094158.

42. Liker MA, Aarabi B, Levy ML. Missile wounds to the head: ballistics and forensics. In : Aarabi B, Kaufman HH, editors. Missile wounds of the head and neck. Park Ridge: Thieme;1999. Vol 2:p. 35–56.
43. Meirowsky AM, Caveness WF, Dillon JD, Rish BL, Mohr JP, Kistler JP, et al. Cerebrospinal fluid fistulas complicating missile wounds of the brain. J Neurosurg. 1981; 54:44–48. PMID:
7463119.

44. Melada A, Marcikić M, Mrak G, Stimac D, Sćap M. Cerebrospinal fluid fistula as a consequence of war head injury. Mil Med. 2002; 167:666–670. PMID:
12188239.

45. Moscote-Salazar LR, Alvis-Miranda HR, Palencia C, Rubiano AM. Emergent decompressive craniectomy in patients with fixed dilated pupils; a single center experience. Bull Emerg Trauma. 2013; 1:175–178.
46. Murano T, Mohr AM, Lavery RF, Lynch C, Homnick AT, Livingston DH. Civilian craniocerebral gunshot wounds: an update in predicting outcomes. Am Surg. 2005; 71:1009–1014. PMID:
16447469.

47. Nagib MG, Rockswold GL, Sherman RS, Lagaard MW. Civilian gunshot wounds to the brain: prognosis and management. Neurosurgery. 1986; 18:533–537. PMID:
3714000.

48. Neuroimaging in the management of penetrating brain injury. J Trauma. 2001; 51:S7–S11. PMID:
11505193.
49. Offiah C, Twigg S. Imaging assessment of penetrating craniocerebral and spinal trauma. Clin Radiol. 2009; 64:1146–1157. PMID:
19913123.

50. Ordog GJ, Wasserberger J, Balasubramanium S. Wound ballistics: theory and practice. Ann Emerg Med. 1984; 13:1113–1122. PMID:
6507972.

51. Ozkan U, Kemaloğlu S, Ozateş M, Aydin MD. Analysis of 107 civilian craniocerebral gunshot wounds. Neurosurg Rev. 2002; 25:231–236. PMID:
12172731.

52. Part 1: Guidelines for the management of penetrating brain injury. Introduction and methodology. J Trauma. 2001; 51:S3–S6. PMID:
11505192.
53. Part 2: Prognosis in penetrating brain injury. J Trauma. 2001; 51:S44–S86. PMID:
11505200.
54. Raimondi AJ, Samuelson GH. Craniocerebral gunshot wounds in civilian practice. J Neurosurg. 1970; 32:647–653. PMID:
5442590.

55. Rish BL, Caveness WF, Dillon JD, Kistler JP, Mohr JP, Weiss GH. Analysis of brain abscess after penetrating craniocerebral injuries in Vietnam. Neurosurgery. 1981; 9:535–541. PMID:
7322316.

56. Rish BL, Dillon JD, Caveness WF, Mohr JP, Kistler JP, Weiss GH. Evolution of craniotomy as a debridement technique for penetrating craniocerebral injuries. J Neurosurg. 1980; 53:772–775. PMID:
7441337.

57. Rish BL, Dillon JD, Meirowsky AM, Caveness WF, Mohr JP, Kistler JP, et al. Cranioplasty: a review of 1030 cases of penetrating head injury. Neurosurgery. 1979; 4:381–385. PMID:
111153.
58. Robles LA. High-velocity gunshot to the head presenting as initial minor head injury: things are not what they seem. Am J Emerg Med. 2012; 30:2089.e5–2089.e7. PMID:
22386344.

59. Rosenfeld JV. Gunshot injury to the head and spine. J Clin Neurosci. 2002; 9:9–16. PMID:
11749010.

60. Saito N, Hito R, Burke PA, Sakai O. Imaging of penetrating injuries of the head and neck: current practice at a level I trauma center in the United States. Keio J Med. 2014; 63:23–33. PMID:
24965876.
61. Selden BS, Goodman JM, Cordell W, Rodman GH Jr, Schnitzer PG. Outcome of self-inflicted gunshot wounds of the brain. Ann Emerg Med. 1988; 17:247–253. PMID:
3345018.

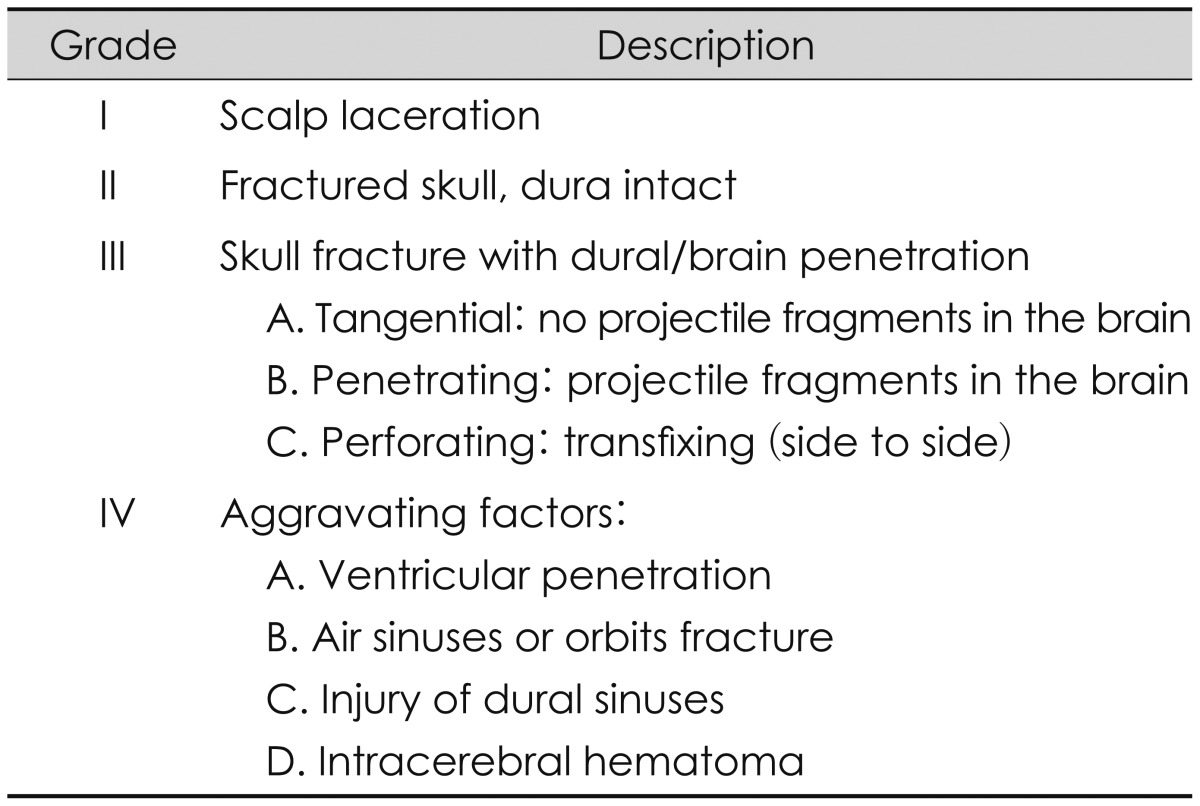
62. Shaffrey ME, Polin RS, Phillips CD, Germanson T, Shaffrey CI, Jane JA. Classification of civilian craniocerebral gunshot wounds: a multivariate analysis predictive of mortality. J Neurotrauma. 1992; 1:S279–S285. PMID:
1588617.
63. Slemon HV. Forward neurosurgery in Italy. J Neurosurg. 1945; 2:332–339.

64. Tsuei YS, Sun MH, Lee HD, Chiang MZ, Leu CH, Cheng WY, et al. Civilian gunshot wounds to the brain. J Chin Med Assoc. 2005; 68:126–130. PMID:
15813246.

65. Vascular complications of penetrating brain injury. J Trauma. 2001; 51:S26–S28. PMID:
11505196.
66. Whitaker R. Gunshot wounds of the cranium: with special reference to those of the brain. Br J Surg. 1915; 3:708–735.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download