This article has been
cited by other articles in ScienceCentral.
Abstract
The authors present a case of rapidly progressing eosinophilic granuloma (EG) of the skull without hemorrhage after minor trauma. A 6-year-old boy presented with a soft mass on the midline of his forehead. He had a surgery for EG 19 months ago. One month earlier, computed tomography (CT) and bone scans were performed to evaluate the possible recurrence of EG, and there was no evidence of recurrence in CT. However, a slightly increased uptake in the bone scan was noted on the midline of the forehead. A rapid growing mass developed in a new spot after a minor trauma 7 days before the patient arrived at the clinic. His physical examination was unremarkable, except for a non-tender, soft, and immobile mass. A plain skull X-ray and CT showed a lytic bony defect on the midline of the frontal bone. Magnetic resonance imaging showed a 1.4 cm sized enhancing mass. Surgical resection and cranioplasty were done. The role of trauma in the development of EG is unclear. However, our case suggests that minor trauma is an aggravating factor for EG formation. Careful observation with regular follow-up is necessary in patients with EG after minor trauma.
Go to :

Keywords: Eosinophilic granuloma, Craniocerebral trauma, Child, Rapid progression
Introduction
Eosinophilic granuloma (EG), a benign local bone disease, is classified as the mildest form of Langerhans' cell histiocytosis (LCH). EG predominantly affects children, adolescents, and young adults, and the skull is the most common site of involvement.
5) The pathologic diagnosis of EG can be confirmed by positive stains of CD1a antigen and protein S-100 or when intracytoplasmic organelles (Birbeck granules) are detected using electron microscopy.
11)
The most common symptom of EG is a tender, growing scalp mass, but it can be asymptomatic and incidentally found on skull X-rays. The clinical course is benign with a tendency to spontaneous regress; however, EG may also recur.
It is common to prove the antecedent of a mild head trauma preceding clinical symptoms. There have been several reported cases of EG associated with epidural hematoma. In fact, the etiology of EG is unknown. Here, we report a case of EG with rapid progression after minor trauma.
Go to :

Case Report
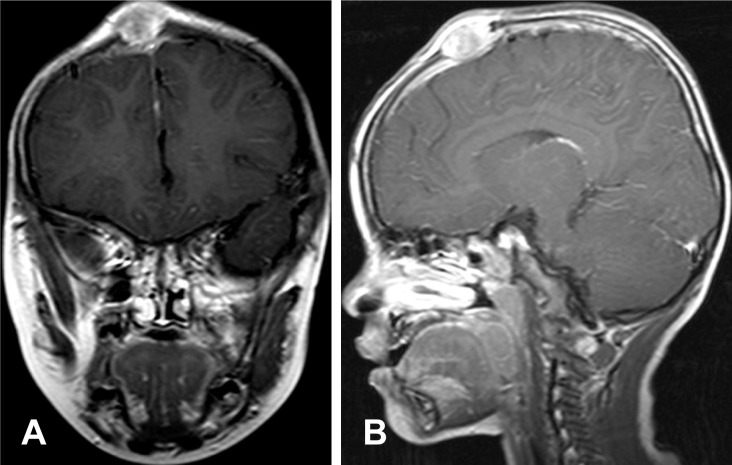
A-6-year-old boy was referred to our hospital with a soft mass on the midline of his forehead. He had undergone surgery for EG in the vertex 19 months ago (
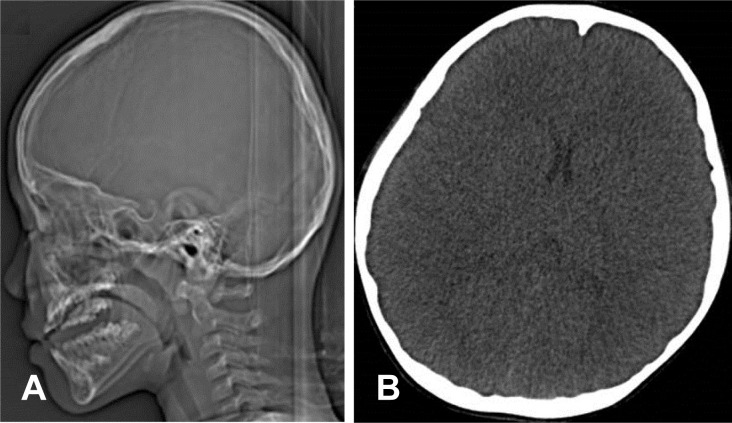
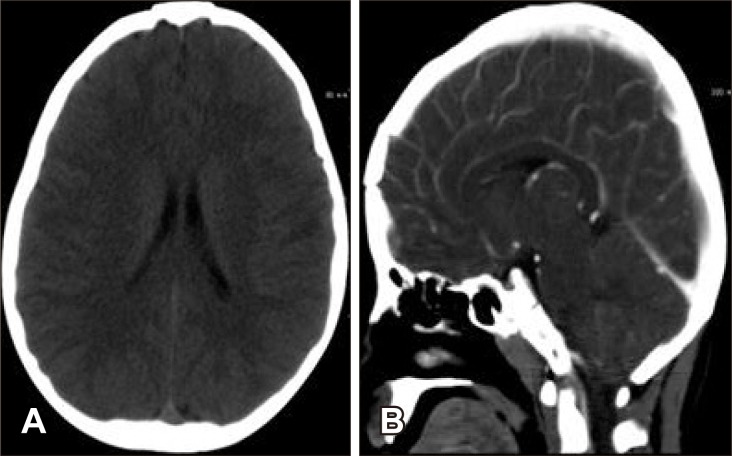
Figure 1). One month prior to minor head trauma, a follow-up computed tomography (CT) (
Figure 2) was performed to check for recurrence, and none was found. One week before his arrival at the hospital, he had hit his head, and the resulting mass grew rapidly after the trauma. The findings of the neurological examination were unremarkable, except for a non-tender, soft, and immobile mass.
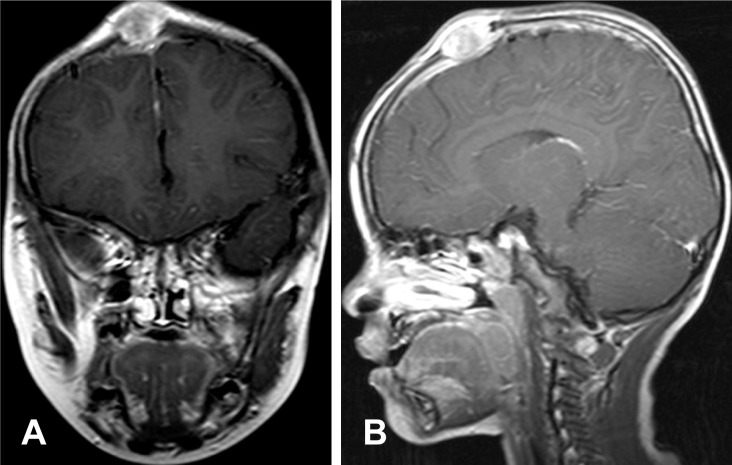 | FIGURE 1T1 enhanced images (A: coronal, B: sagittal) showing a 2.3 cm-sized enhancing mass in the mid vertex 19 months ago.
|
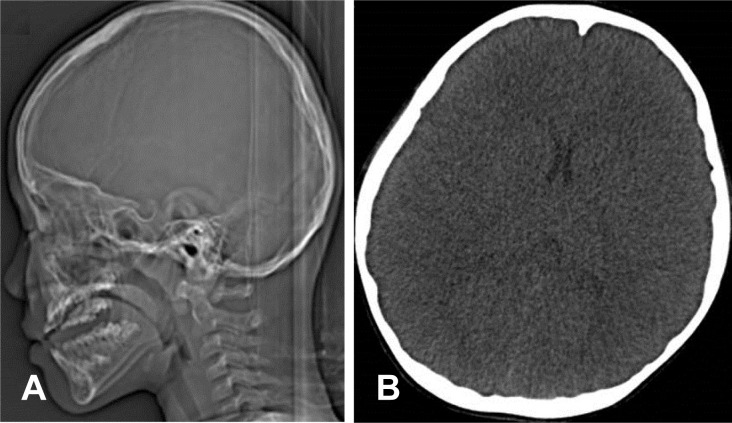 | FIGURE 2A: Skull lateral image taken one month prior to trauma showed no evidence of recurrence. B: Non-contrast axial computed tomography image.
|
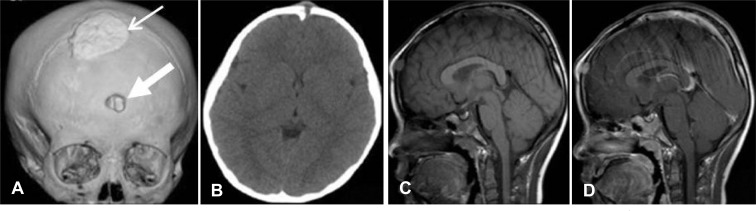
The three-dimensional (3D) CT showed a lytic bony defect on the frontal bone without hemorrhage (
Figure 3A and B) and the enhanced magnetic resonance imaging (MRI) revealed a 1.4 cm-sized growing mass on the midline of the forehead (
Figure 3C and D). The results of the blood tests were normal except for eosinophilia. The level of erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) was within normal limits.
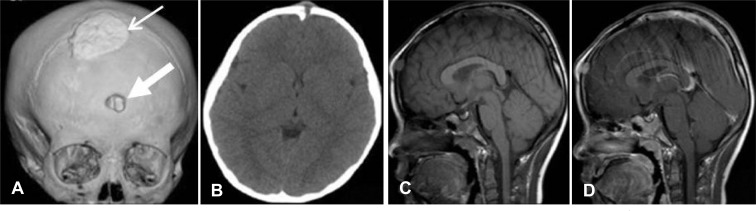 | FIGURE 3A, B: Three-dimensional computed tomography showing lytic bony defect in the frontal region (small arrow: previous operation lesion, large arrow: new developed lesion). C, D: Sagital magnetic resonance imaging showing a 1.4 cm-sized enhnacing mass (C: non-contrast, D: contrast).
|
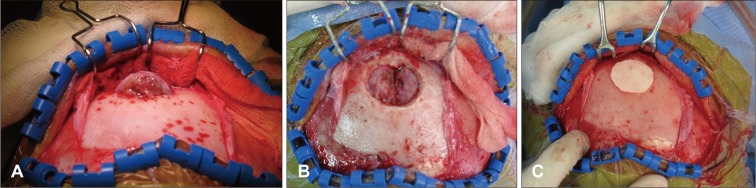
The patient was operated on the day following his admission. The protruding mass extended from the scalp through the defect in the frontal bone, and was visualized when the scalp flap was reflected (
Figure 4A). After removal of the bone flap and tumor, it was noted that there was no hematoma and the dura mater was intact without invasion (
Figure 4B). The tumor was removed completely and the bony defect was replaced with bone cement (
Figure 4C). The postoperative course was uneventful.
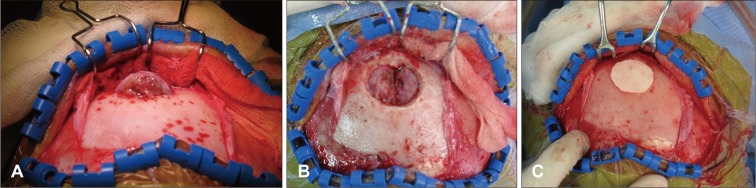 | FIGURE 4A: After the scalp flap was reflected, a protruding mass was found. (B) The mass was completely removed, and (C) a cranioplasty was performed with bone cement.
|
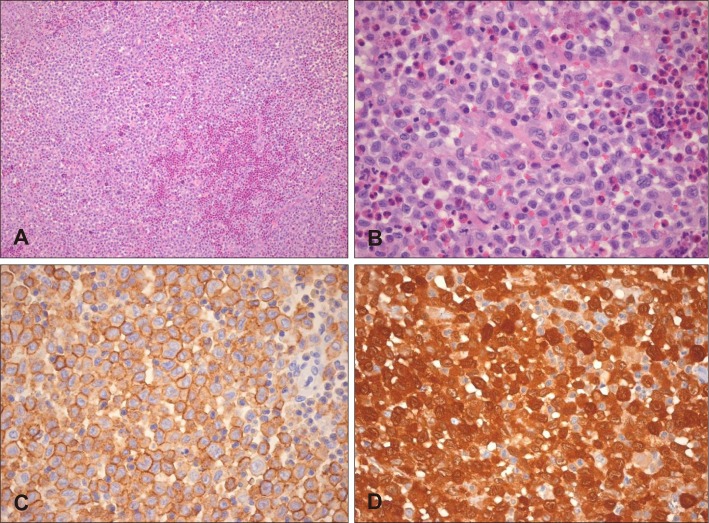
The histopathological examination revealed numerous oval Langerhans' cells and eosinophils (
Figure 5A and B). The Langerhans' cells were stained for CD1a and S-100 (
Figure 5C and D). These findings were consistent with LCH. The patient was followed-up six months after the operation and had a normal neurologic examination at that point. The 3D CT showed no recurrence (
Figure 6).
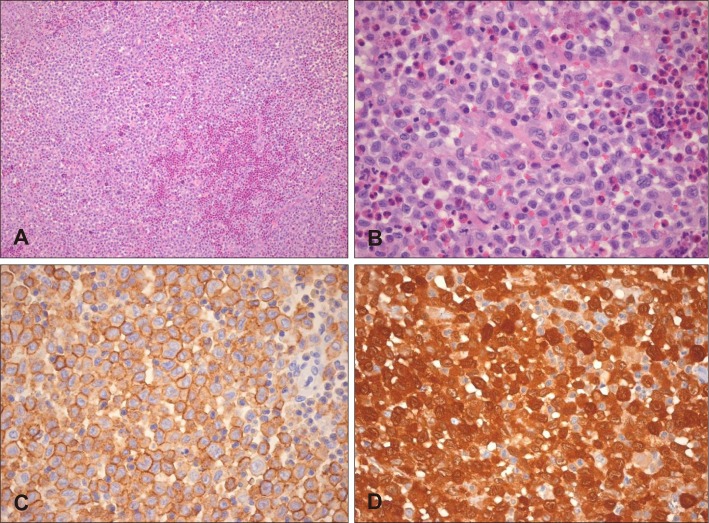 | FIGURE 5A, B: There are numerous oval Langerhans cells with many nuclei containing linear grooves (H-E, ×100). Eosinophilic microabscesses are noted (H-E, ×400). C: The surfaces of the Langerhans cells are uniformly positive for CD1a staining (×400). D: Strong positive staining is both nuclear and cytoplasmic with S-100 (×400).
|
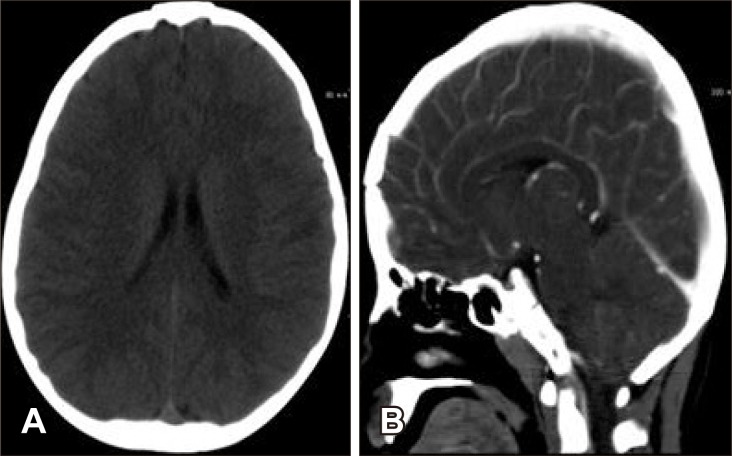 | FIGURE 6Computed tomography six months after the operation showing no recurrence. A: Axial noncontrast image. B: Sagittal contrast image.
|
Go to :

Discussion
LCH is a unifocal or multifocal disorder of the bone or soft tissue, most often appearing as a lytic lesion of the skull. EG is the mildest form of LCH.
5) The exact incidence of EG is not well known but Vandenberg and Coley
12) found that it accounted for only 2.4% of benign skull tumors. In the series of cases studied by Jelsma and Ross,
4) the incidence of EG was found to be 12% of skull bone tumors.
The most common symptom of EG is a tender, enlarged scalp mass on the parietal and frontal bones. EG may be asymptomatic and only discovered on a skull X-ray by chance. The X-ray radiologic findings consist of a punched-out, skull lesion with sharply defined margins. The CT scan usually shows soft tissue within the area of bony destruction. As the clinical and radiologic findings are not specific enough to determine the diagnosis, cytology is very helpful in diagnosing EG. The key feature is the identification of characteristic Langerhans cells in a background of eosinophils and red blood cells.
5)
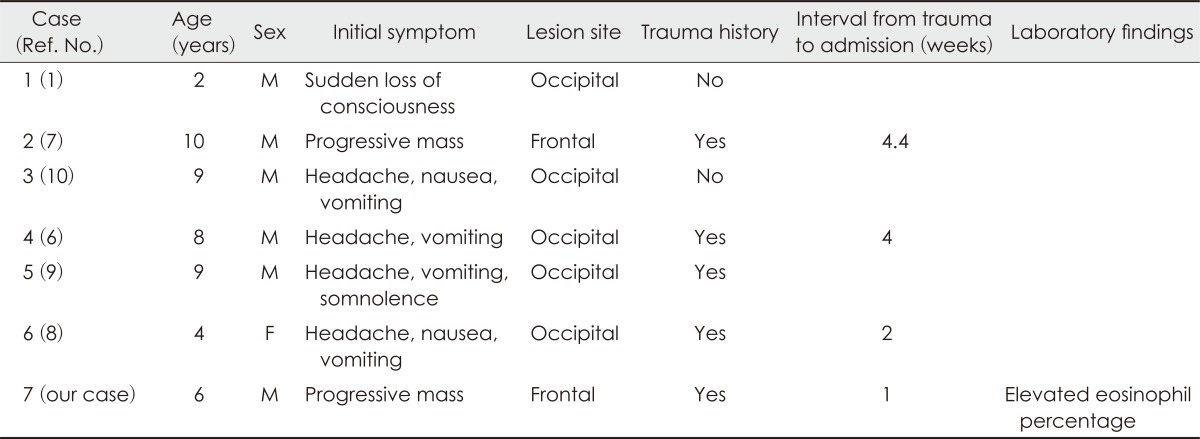
There is no definite disease etiology for EG. However, autoimmune diseases, inflammatory processes, and uncontrolled Langerhans cell replication can be considered to be etiological factors.
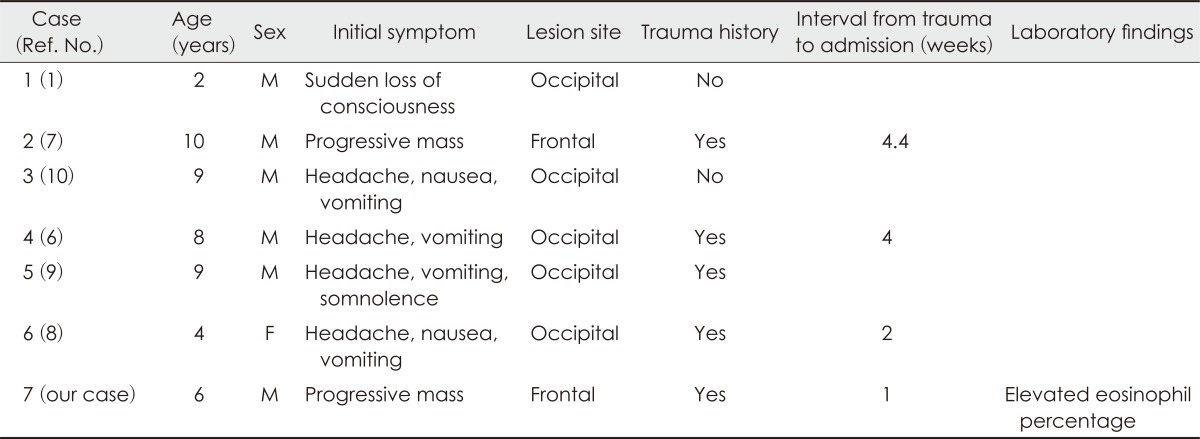
3) Also, minor trauma is considered an etiologic factors. There have been six reported cases of EG associated with epidural hematoma (
Table 1).
1678910) The possible mechanisms of epidural hematomas in the six cases consisted of a rupture of the tumor cyst, communicating with the epidural vein and the sinus pericranii, or a head trauma-related intratumoral hemorrhage, which subsequently penetrated into the epidural space. However, the two theories could not be applied in our case. All six cases were associated with epidural hemorrhages, while our case was not. In our case, no hematoma or hemorrhage was found in the CT/MRI image, or in intraoperative and pathologic findings.
TABLE 1
Summary of previous reports of eosinophilic granuloma associated with epidural hematoma

The patient in our case regularly visited the clinic for follow-up appointments due to his history of EG. The CT scan taken one month prior to the trauma showed no definite recurrence; however, a newly developed EG lesion was found one week after the trauma. This indicates that the development of EG may be associated with trauma.
In this case, it is thought that EG developed through a local inflammatory response due to a minor trauma. Trauma may be a trigger factor of the inflammatory response instead of the etiology of the disease.
The elevated levels of ESR and CRP are found in some, but not all, cases of EG. This is because EG lesions are limited to local level and the time between diagnosis and trauma varies. In the present case, the author finds the period between the trauma and diagnosis to be relatively long.
Factors related to hematoma formation may include the trauma's intensity and the time interval after the trauma. For example, in one case, a patient with an epidural hematoma had a two-week time interval, with a fluid level confirmed four weeks later.
In the management of solitary EG, surgical excision is recommended and radiotherapy can be considered as an adjuvant therapy if necessary. Some authors advocate surgical excision followed by postoperative treatment that includes low-dose radiotherapy, intralesional application of corticosteroids, or a combination of chemotherapy and radiotherapy.
11)
Other studies found that solitary calvarial EG in skeletally immature patients 14 years of age or younger resolved fully without any recurrence.
2) EG is responsive to steroid treatment and this indicates that the etiology of EG is associated with local inflammatory processes. To avoid surgical procedures, a short period of observation may be useful in the initial care of EG.
The prognosis depends on the age of the patient at the time of diagnosis and the number of lesions. The local recurrence rate is 6%, and new lesions appear in about 22% of patients, therefore, long-term follow-up is recommended.
311)
Go to :

Conclusion
The role of trauma in the development of EG is unclear. Our case suggests that minor trauma may be an aggravating factor for the progression of EG, based on the radiological findings before and after the trauma. Thus, careful observation with regular follow-up is needed for patients with EG after trauma.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download