Abstract
Spine surgery has been increased as the population ages, but the occurrence of unusual complication such as remote cerebellar hemorrhage (RCH) is not well understood. We recently experienced a case of RCH in a 60-year-old woman showed neurologic dysfunction after degenerative lumbar spine surgery. There was no definite dural tearing and cerebrospinal fluid (CSF) loss during operation. Brain magnetic resonance imaging showed cerebellar hemorrhage. The patient received conservative management and rehabilitation program. Most other reports have been suggested that RCH after spinal surgery might be related with excessive CSF drainage perioperatively. Minimizing of CSF loss during operation would be helpful to reduce the risk of RCH. If large volume of CSF has been lost accompanied by neurologic deterioration, brain imaging is necessary simultaneously.
The incidence of a remote cerebellar hemorrhage (RCH) after spinal surgery has rarely been reported,123456789101112131415) although an RCH after spinal surgery was first reported in 1981 by Chadduck.7) The pathophysiology of RCHs has not been clearly explained.7) Many of the reported cases of RCH presented with intraoperative dural tearing and an extensiveloss of cerebrospinal fluid (CSF). We reported a case of an RCH that occurred after spinal surgery and reviewedthe literature related to this phenomenon.
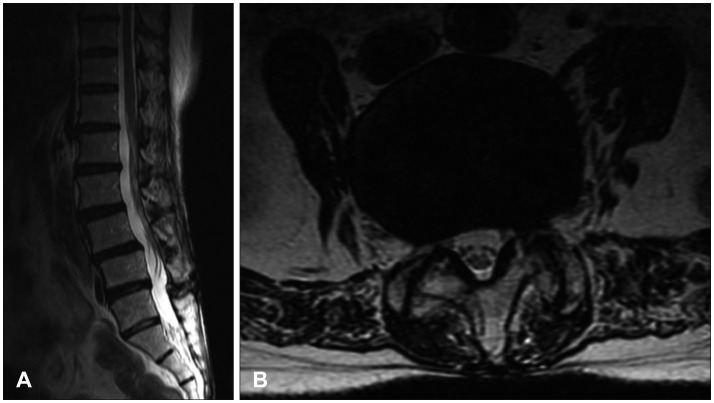
A 60-year-old woman visited the hospital with pain in her back and both legs, which she had experienced for one year. The initial visual analog scale score for the back pain was 7, and the initial blood pressure was normotensive at 120/80 mm Hg. The patient's body mass index was 21.3. Neurologically, her consciousness and orientation were clear. Thoracolumbar kyphosis was revealedon the radiological examination. The Cobb's angle was between T12, and the S1 was 6.5 degrees. The T score ofthe lumbar spine on dual energy X-ray absorptiometry was -1.1, as in osteopenia. The lumbar spine magnetic resonance imaging (MRI) revealed lumbarization of the S1 vertebra, degenerative spondylolisthesis at L4/5 and retrolisthesis at L5/S1 (Figure 1).
A complete laminectomy with a Smith-Petersen osteotomy at L4 and L5, a discectomy at L4-5 and L5S1, and L3-4-5-S1 pedicle-screw fixation were performed (Figure 2). There were no accidents perioperatively. The intraoperative motor evoked potentials and the somatosensory evoked potential monitoring of the lower extremities did not show any changes during the surgery. Anti-adhesive agent of Sodium hyaluronate was applied on dura mater. Ten French hemovac drains (Zimmer, Dover, OH, USA) were placed in the sub-muscular space, and the deep fascia, subcutaneous tissue and skin were closed layer by layer with a watertight procedure. Postoperative pain was controlled routinely with an opioid-filled patient controlled analgesia (PCA) pump.
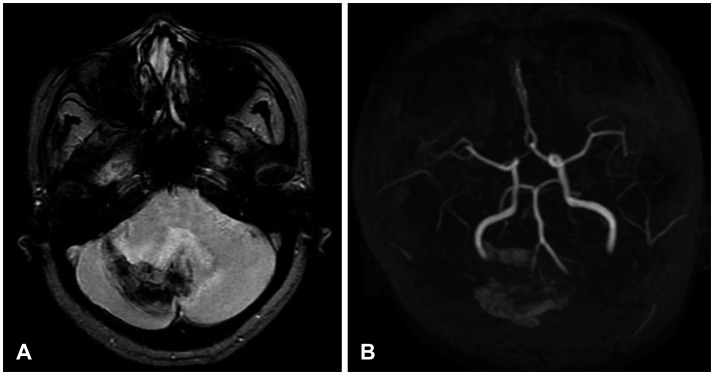
The drains were connected with negative pressure chambers. On postoperative day 1, the patient was comfortable and asymptomatic. However, 530 mL of serosanguinous fluid was present in the surgical drain, and 305 mL and 315 mL were present on the 2nd and 3rd postoperative day, respectively. The patient complained of dizziness and a mild headache on the 3rd postoperative day, and the intravenous PCA was stopped and the hemovac drains were removed. Eight days after surgery, the patient was less responsive as well as diplopic, and she presented with dysarthria and difficulty in maintaining her equilibrium. An urgent MRI revealed a cerebellar hemorrhage in the right cerebellar hemisphere and vermis (Figure 3). The patient underwent bed rest, therapy with fluids, blood pressure control, and close radiological monitoring as well as a thorough rehabilitation program during her hospitalization. A month after the original fusion operation, the hemorrhage was completely resolved, and the patient returned home and was able to walk by herself without support. Her symptoms improved, and finally, she has become neurologically symptom-free.
During brain surgery, decreased intracranial pressure followed by a loss of CSF might lead to a caudal shift of the brain and rupture of the venous cortical blood vessel.2) This sequence is hypothesized to be a pathomechanism of postoperative removal of an intracranial hemorrhage. A postoperative RCH is rare, particularly after spinal surgery, since first reported by Chadduck.7) No reports have explained the exact RCH pathomechanism, although several cases of RCH have been reported.
An RCH is characteristically located in the upper vermis and cerebellar sulci, in which the cerebellar draining veins are located. RCH computed tomography findings are typically linear with alternating hyperdensity of blood and hypodensity of cerebellum because the blood collects in the folial subarachnoid spaces and between the folia and the tentorium. This finding was described as the 'zebra sign'.3)
Most authors suggest that the RCH pathomechanism is related to the venous system and perioperative CSF loss. A hemorrhagic transformation of an arterial ischemic stroke or active arterial bleeding causes more profuse hemorrhaging than a RCH and tends to be unilateral, whereas an RCH is nearly bilateral.1234510) Some authors suggest that the pathomechanism is a hemorrhagic transformation of a venous infarction. In this case, evidence of an infarction could be found on the brain imaging. A loss of CSF causes a caudal descent of the cerebellum, following stretching and tearing of adjacent venous structures; CSF loss leads to hemorrhaging. This hypothetical progression is known as 'cerebellar sag'.89101112131415) This condition makes tearing of the microcirculation vessels, which is unlikely to produce clinical symptoms and diagnostic imaging signs typical of a stroke. An RCH involves an area larger than that of a single vein and typically does not demonstrate edema or cerebellar swelling; this finding does not conform exactly to the cerebellar sag theory.4)
An RCH is treated surgically or conservatively according to the state of patient. A small RCH could be managed without surgery, with medical treatment including bed rest, therapy with fluids and blood pressure control, which is based on the hemorrhage itself and its complications, not on the occurrence on an infarction.
The prognosis for a patient with an RCH is generally favorable, with transient or mild neurological deficits.26) Brain imaging is not performed routinely during spinal surgery, andan RCH with mild symptoms such as headache, nausea or dizziness after surgery might be missed. The incidence of an RCH after spinal surgery is difficult to assess, and the occurrence might be higher than reported.
In this case, the patient did not experience definite dural tearing during the surgery. However, a large amount of drainage was found postoperatively. Extensive drainage might be evidence of limited dural tearing that could not be detected during the surgery. Because dural micro-tears could deteriorate fromthe negative pressure of drainage after surgery, sudden increase of drainage volume should be managed carefully including brain investigation.
References
1. Adam R, Priglinger M, Harrington T, Gottlieb D, Krause M. An unusual cause of cerebellar hemorrhage in a young patient: essential thrombocythemia. J Stroke Cerebrovasc Dis. 2014; 23:e373–e374. PMID: 24582788.

2. Brockmann MA, Groden C. Remote cerebellar hemorrhage: a review. Cerebellum. 2006; 5:64–68. PMID: 16527766.

3. Brockmann MA, Nowak G, Reusche E, Russlies M, Petersen D. Zebra sign: cerebellar bleeding pattern characteristic of cerebrospinal fluid loss. Case report. J Neurosurg. 2005; 102:1159–1162. PMID: 16028781.
4. Calisaneller T, Yilmaz C, Ozger O, Caner H, Altinors N. Remote cerebellar haemorrhage after spinal surgery. Can J Neurol Sci. 2007; 34:483–484. PMID: 18062460.

5. Cavanilles-Walker JM, Tomasi SO, Sgier F, Kröber M. Remote cerebellar haemorrhage after lumbar spine surgery: case report. Arch Orthop Trauma Surg. 2013; 133:1645–1648. PMID: 24121622.

6. Cevik B, Kirbas I, Cakir B, Akin K, Teksam M. Remote cerebellar hemorrhage after lumbar spinal surgery. Eur J Radiol. 2009; 70:7–9. PMID: 18294795.

7. Chadduck WM. Cerebellar hemorrhage complicating cervical laminectomy. Neurosurgery. 1981; 9:185–189. PMID: 7266820.

8. Farag E, Abdou A, Riad I, Borsellino SR, Schubert A. Cerebellar hemorrhage caused by cerebrospinal fluid leak after spine surgery. Anesth Analg. 2005; 100:545–546. PMID: 15673890.

9. Friedman JA, Ecker RD, Piepgras DG, Duke DA. Cerebellar hemorrhage after spinal surgery: report of two cases and literature review. Neurosurgery. 2002; 50:1361–1363. discussion 1363-1364PMID: 12015857.

10. Honegger J, Zentner J, Spreer J, Carmona H, Schulze-Bonhage A. Cerebellar hemorrhage arising postoperatively as a complication of supratentorial surgery: a retrospective study. J Neurosurg. 2002; 96:248–254. PMID: 11838798.
11. Khalatbari MR, Khalatbari I, Moharamzad Y. Intracranial hemorrhage following lumbar spine surgery. Eur Spine J. 2012; 21:2091–2096. PMID: 22349967.

12. Khong P, Jerry Day M. Spontaneous cerebellar haemorrhage following lumbar fusion. J Clin Neurosci. 2009; 16:1673–1675. PMID: 19793659.

13. Konya D, Ozgen S, Pamir MN. Cerebellar hemorrhage after spinal surgery: case report and review of the literature. Eur Spine J. 2006; 15:95–99. PMID: 16007466.

14. Mallio CA, Sarà M, Pistoia ML, Occhicone F, Errante Y, Giona A, et al. Bilateral remote cerebellar haemorrhage after spinal surgery: a case study and review of the literature. Brain Inj. 2014; 28:1216–1222. PMID: 24865277.

15. Nam TK, Park SW, Min BK, Hwang SN. Remote cerebellar hemorrhage after lumbar spinal surgery. J Korean Neurosurg Soc. 2009; 46:501–504. PMID: 20041065.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download