1. Balasubramanian K, Kalsi P, Greenough CG, Kuskoor Seetharam MP. Reliability of clinical assessment in diagnosing cauda equina syndrome. Br J Neurosurg. 2010; 24:383–386. PMID:
20726746.

2. Bell DA, Collie D, Statham PF. Cauda equina syndrome: what is the correlation between clinical assessment and MRI scanning? Br J Neurosurg. 2007; 21:201–203. PMID:
17453789.
3. Bradford DS, McBride GG. Surgical management of thoracolumbar spine fractures with incomplete neurologic deficits. Clin Orthop Relat Res. 1987; (218):201–216. PMID:
3568482.

4. Caputo LA, Cusimano MD. Atypical presentation of cauda equina syndrome. J Can Chiropr Assoc. 2002; 46:31–38.
5. Celik EC, Kabatas S, Karatas M. Atypical presentation of cauda equina syndrome secondary to lumbar disc herniation. J Back Musculoskelet Rehabil. 2012; 25:1–3. PMID:
22398260.

6. Dai LY, Wang XY, Jiang LS. Neurologic recovery from thoracolumbar burst fractures: is it predicted by the amount of initial canal encroachment and kyphotic deformity? Surg Neurol. 2007; 67:232–237. discussion 238PMID:
17320624.

7. Domen PM, Hofman PA, van Santbrink H, Weber WE. Predictive value of clinical characteristics in patients with suspected cauda equina syndrome. Eur J Neurol. 2009; 16:416–419. PMID:
19490073.

8. Fairbank J, Hashimoto R, Dailey A, Patel AA, Dettori JR. Does patient history and physical examination predict MRI proven cauda equina syndrome? Evid Based Spine Care J. 2011; 2:27–33. PMID:
23230403.

9. Fraser S, Roberts L, Murphy E. Cauda equina syndrome: a literature review of its definition and clinical presentation. Arch Phys Med Rehabil. 2009; 90:1964–1968. PMID:
19887225.

10. Gitelman A, Hishmeh S, Morelli BN, Joseph SA Jr, Casden A, Kuflik P, et al. Cauda equina syndrome: a comprehensive review. Am J Orthop (Belle Mead NJ). 2008; 37:556–562. PMID:
19104682.
11. Gooding BW, Higgins MA, Calthorpe DA. Does rectal examination have any value in the clinical diagnosis of cauda equina syndrome? Br J Neurosurg. 2013; 27:156–159. PMID:
23113877.

12. Harrop JS, Hunt GE Jr, Vaccaro AR. Conus medullaris and cauda equina syndrome as a result of traumatic injuries: management principles. Neurosurg Focus. 2004; 16:e4. PMID:
15202874.

13. Herndon WA, Galloway D. Neurologic return versus cross-sectional canal area in incomplete thoracolumbar spinal cord injuries. J Trauma. 1988; 28:680–683. PMID:
3367414.
14. Hu SS, Capen DA, Rimoldi RL, Zigler JE. The effect of surgical decompression on neurologic outcome after lumbar fractures. Clin Orthop Relat Res. 1993; (288):166–173. PMID:
8458130.

15. Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997; 79:69–83. PMID:
9010188.
16. Kim NH, Lee HM, Chun IM. Neurologic injury and recovery in patients with burst fracture of the thoracolumbar spine. Spine (Phila Pa 1976). 1999; 24:290–293. discussion 294PMID:
10025025.

17. Kim TW, Yoon JW, Heo W, Park HS, Rhee DY. Lumbar Disc Herniation Presenting Cauda Equina Syndrome. J Korean Neurosurg Soc. 2006; 39:40–45.
18. Kingwell SP, Curt A, Dvorak MF. Factors affecting neurological outcome in traumatic conus medullaris and cauda equina injuries. Neurosurg Focus. 2008; 25:E7. PMID:
18980481.

19. Kostuik JP, Harrington I, Alexander D, Rand W, Evans D. Cauda equina syndrome and lumbar disc herniation. J Bone Joint Surg Am. 1986; 68:386–391. PMID:
2936744.

20. Meves R, Avanzi O. Correlation between neurological deficit and spinal canal compromise in 198 patients with thoracolumbar and lumbar fractures. Spine (Phila Pa 1976). 2005; 30:787–791. PMID:
15803082.

21. Mohanty SP, Venkatram N. Does neurological recovery in thoracolumbar and lumbar burst fractures depend on the extent of canal compromise? Spinal Cord. 2002; 40:295–299. PMID:
12037711.

22. O'Laoire SA, Crockard HA, Thomas DG. Prognosis for sphincter recovery after operation for cauda equina compression owing to lumbar disc prolapse. Br Med J (Clin Res Ed). 1981; 282:1852–1854.
23. Orendácová J, Cízková D, Kafka J, Lukácová N, Marsala M, Sulla I, et al. Cauda equina syndrome. Prog Neurobiol. 2001; 64:613–637. PMID:
11311464.
24. Sylvester PA, McLoughlin J, Sibley GN, Dorman PJ, Kabala J, Ormerod IE. Neuropathic urinary retention in the absence of neurological signs. Postgrad Med J. 1995; 71:747–748. PMID:
8552542.

25. Thongtrangan I, Le H, Park J, Kim DH. Cauda equina syndrome in patients with low lumbar fractures. Neurosurg Focus. 2004; 16:e6. PMID:
15202876.
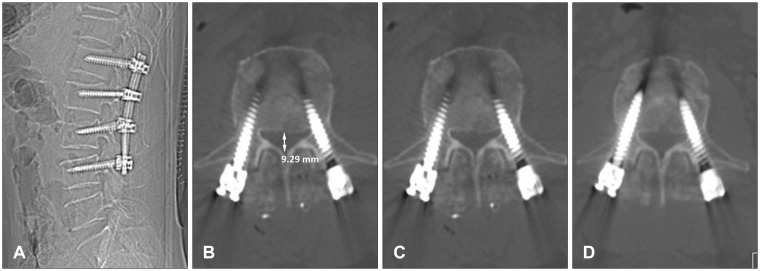
26. Wang US, Ju CI, Kim SW, Wang HS, Lee SM. Short Segment Screw Fixation without Fusion for Low Lumbar Burst Fracture: Severe Canal Compromise but Neurologically Intact Cases. Korean J Neurotrauma. 2013; 9:101–105.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download