Abstract
The aim of this paper was to report the effect of temporary and chronic spinal cord stimulation for refractory neuropathic pain in neuralgic amyotrophy (NA). A 35-year-old female presented with two-months history of a severe, relentless neuropathic pain of the left shoulder, forearm, palm, and fingers. The neuropathic pain was refractory to various medical treatments, including nonsteroidal anti-inflammatory drugs, opiates, epidural and stellate ganglion blocks, and typically unrelenting. The diagnosis of NA was made with the characteristic clinical history and magnetic resonance imaging. The patient underwent a temporary spinal cord stimulation to achieve an adequate pain relief because her pain was notoriously difficult to control and lasted longer than the average duration (about 4 weeks on average) of a painful phase of NA. Permanent stimulation was given with paddle lead. The neuropathic pain in her NA persisted and she continued using the spinal cord stimulation with 12 months after development of NA. The temporary spinal cord stimulation was effective in a patient with an extraordinary prolonged, acute painful phase of NA attack, and the subsequent chronic stimulation was also useful in achieving an adequate analgesia during the chronic phase of NA.
Neuralgic amyotrophy (NA)-also known as Parsonage-Turner syndrome or brachial plexus neuritis-is an under-recognized but distinct clinical syndrome, with a characteristic clinical presentation of an acute, severe neurogenic pain in the shoulder or arm lasting for several days or weeks, followed by muscle weakness, atrophy, and sensory loss as the pain diminishes.13171920212223) The pain is a hallmark of NA and typically relentless and severe [numerical rating scale (NRS)>7].1721) There is no successful treatment of NA yet and the initial pain at the onset of an attack is only partly relieved by traditional analgesics.1721)
Although spinal cord stimulation (SCS) has been known as an accepted, effective therapy for patients with chronic neuropathic pain such as complex regional pain syndrome (CRPS) type I as well as in a variety of other neuropathic conditions,127121524) its effectiveness against the neuropathic pain of NA was not reported. Herein we describe a 35-year-old woman with intractable neuropathic pain from NA who responded to SCS.61524)
A 35-year-old female presented with an eight-week history of a severe, unrelenting pain in the left palm and radial four fingers, medial forearm, and in the shoulder pain waking her from sleep. The pain was described as dull, crushing, and deep pressure-like and of an extreme severity (8-9/10 on NRS). The pain made the patient sit on the table constantly holding her arm close to her body, keeping it immobile.
Eight weeks ago, she woke up in the morning with a severe pain in her left shoulder and hand and this pain was unlikely any pain she experienced before. The pain worsened at this day and become constant and unrelenting since then and it was heavier at night. A weakness in her left hand progressively developed 2 weeks after the onset of pain. The pain did not respond to medications and physical therapy. A magnetic resonance imaging (MRI) of the cervical spine showed no abnormalities. The electromyography study suggested an incomplete brachial plexopathy.
On examination, a moderate tenderness in the left shoulder with a moderate weakness [manual muscle testing (MMT) grade 3] of the left hand grasping and finger movement was observed. The sensory examination showed patch areas of hypesthesia, paresthesia, and mechanical allodynia to light touch and pressure in her left shoulder, medial forearm, thenar side of the palm and in four fingers which corresponded to the pain sites (Figure 1A). Her NRS at examination was (8/10, NRS) and the pain was more severe at night (9/10, NRS). The MRI of the left brachial plexus showed a diffuse swelling, increased signal intensity, and an enhancement of whole trunks of the left brachial plexus and its divisions suggesting a brachial plexopathy (Figure 1B and C). There was a marked asymmetrical uptake in the blood pool phase of the three-phase bone scintigraphy (Figure 1D) and skin temperature asymmetry on digital infrared thermal imaging (Figure 1E).
After admission for pain control, the amount of daily medication was increased to gabapentin 2,400 mg, IR-codon 40 mg, oxycodone 40 mg, amitriptyline 20 mg, and 50 mcg/hr transdermal fentanyl. However, the pain relief was not satisfactory and the patient got an injection of fentanyl 10 mg five times a day as needed. A stellate ganglion block was effective only for several hours.
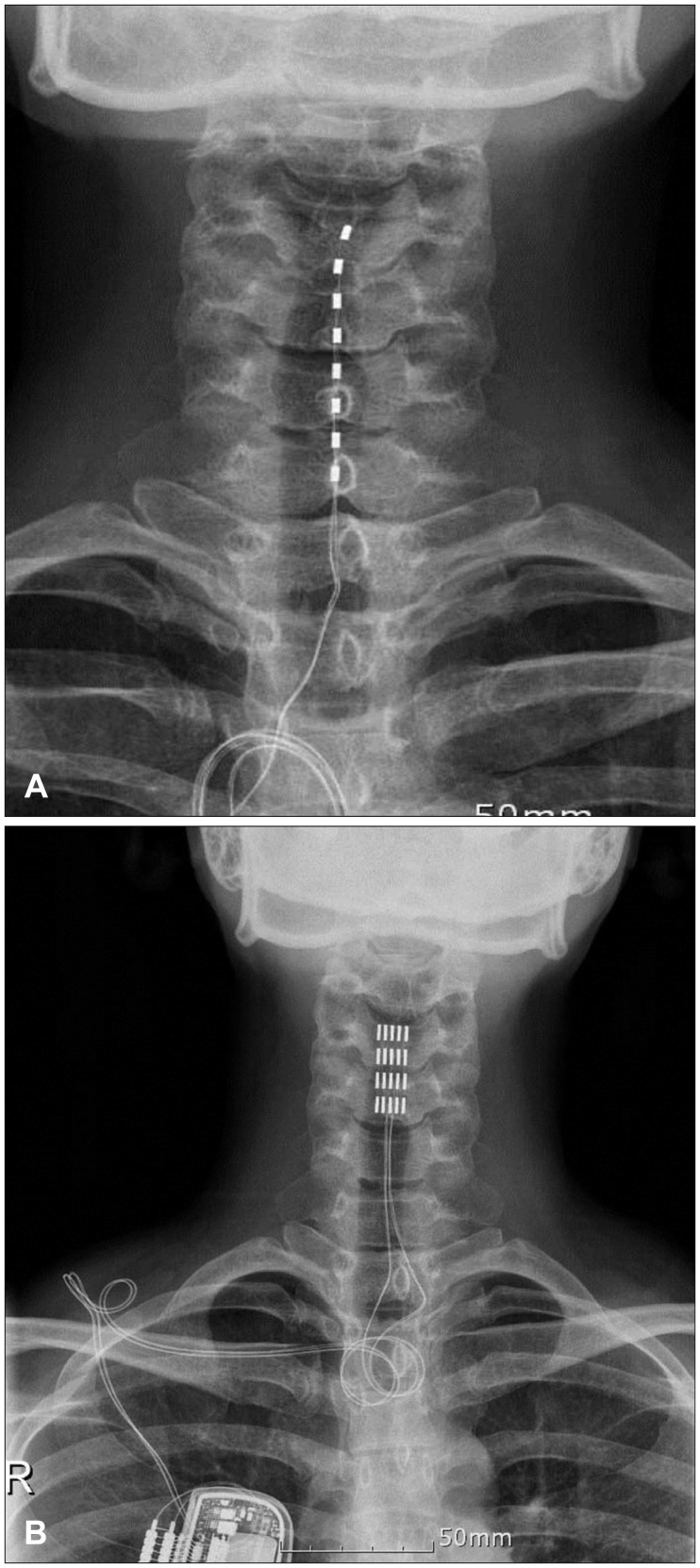
Considering the chronicity and severity of neuropathic pain, a temporary trial of SCS was performed (approximately 10 weeks after onset of pain) with a cylindrical electrode (Octrode®, Plano, TX, USA) at the level of C3-5 (Figure 2A). The severe dull, crushing and deep pressure-like spontaneous pain and the evoked pain (mechanical allodynia) in the arm and hand was alleviated for about 50% (contact polarity 3-4+, 100 usec, 100 Hz, 1.5 mA). She assessed the effect of SCS as fairly successful and expressed the pain intensity (4-5/10, NRS). During the temporary stimulation period of 21 days, she was satisfied with the analgesic efficacy of SCS and wanted to have a chronic stimulation.
Approximately 12 weeks after the onset of severe pain, a chronic SCS system was implanted through a paddle lead SCS (Penta™ and Eon-Mini® rechargeable, St. Jude Medical, Plano, TX, USA) (Figure 2B). After one week of adjustment of the stimulation parameters (1-4+, 400 usec, 90 Hz, 1.4 mA), she finally discontinued a nighttime injection of fentanyl and switched into IR-codon 10 mg as needed. The analgesic efficacy of SCS was more effective in controlling pain and allodynia in the medial forearm, palm and 2nd, 3rd, 4th fingers (more than 60% relief, subjective assessment). The effectiveness of chronic SCS was fairly consistent during the follow-up of 12 months and she evaluated her pain as 4 (daytime)-5 (nighttime) in on an 11 point NRS. At the last follow-up of 12 months after the onset of pain, the patient still suffered a serious, chronic pain (fluctuating 3-6/10, NRS) and grade IV MMT weakness of left hand. Her medication at the last follow-up was gabapentin 1,200 mg, oxycodone 20 mg, amitriptyline 10 mg, and IR-codon 20 mg per day.
NA, which was first described by Dreschfeld4) in 1886 as a distinct clinical syndrome, is characterized by attacks of neuropathic pain and subsequent patch paresis in the upper extremities. The etiology of idiopathic NA remains unknown and an immune-mediated process seems to garner the most support currently.111425) A hallmark of NA is a sudden, severe painful onset and the patch distribution of motor, sensory and autonomic symptoms.1727) Any part of the brachial plexus and the lumbosacral plexus can be involved, with any combination of motor and sensory impairment.1721) A bilateral involvement of the brachial plexus occurs in approximately 30% of patients; clinical features are commonly asymmetric in presentation.21) The upper trunk of the brachial plexus is most usually involved, but any part of this plexus can be affected too. Also painless attacks can occur.1721)
In 96% of patients, NA presents with acute, severe pain in the upper extremities, neck and/or trunk, which usually causes the individual to wake up early in the morning. The pain then increases to its maximum severity over the next few hours.21) Typically is the pain relentless, worse at night and is unlikely anything the patient has ever experienced before, with pain scores of at least 7 being assigned on the numerical scale of 0 to 10.19) This initial pain lasts for 4 weeks on average, but disappears in 5% of cases within 24 hours and lasts for at least 2 months in 10% of individuals.21) Subsequently, at least 75% of patients will go on to develop an additional type of pain, possibly because of hypersensitivity of the damaged nerves to mechanical stretch or maintained posture, shooting or radiating pains to the arms or trunk that dissipate over a period of weeks to months. Additionally, two-thirds of individuals develop a musculoskeletal pain at the origin or insertion of the paretic or compensating muscles, especially in the periscapular and cervical-occipital regions.182021)
The treatment of pain and residual sequele of a NA is directed to a supportive management. Adequate analgesia including the use of opiates in the acute painful phase and appropriate physical therapy and rehabilitation for shoulder paresis and glenohumeral instability in the chronic phase are the cornerstones of management.172123) The prognosis of NA was traditionally thought to be positive, with full recovery occurring in 80% to 90% of patients 2 to 3 years following the onset of symptoms.316) However, subsequent studies showed that the overall recovery was less favorable than usually assumed.172123) Persistent pain and paresis was experienced in approximately two-thirds of patients that were followed for 3 years or more, with a marked effect on their daily life and employment.5172123)
SCS is known to be a safe and effective treatment option for selected patients with medically refractory chronic pain syndrome such as failed back surgery syndrome or CRPS, and peripheral neuropathic pain.127121524) SCS involves the placement of electrodes in the epidural space and production of an electrical current by means of a pulse generator. The analgesic mechanism produced by SCS is believed to work by the gate control mechanism and modulation of excitatory and inhibitory neurotransmitter release in the dorsal horn.924) Although SCS has been reported to be effective in various kinds of neuropathic pain,127121524) the effectiveness of SCS was not reported in the treatment of a typical neuropathic pain of NA.
The reason why we performed the trial SCS in this patient is simple; we wanted to relieve an extraordinary prolonged period of severe pain refractory to maximal medical treatment (NRS>7/10). Therefore, we adopted a temporary SCS as a salvage procedure within a desperate condition in our case. This kind of temporary SCS treatment has already been reported in the acute and subacute phase of postherpetic neuralgia.1026) Another reason for temporary SCS was that the typical neuropathic pain nature of NA. Although a typical cutaneous manifestation of CRPS-1, such as edema and sudomotor sign, was absent, the symptoms and signs and some ancillary investigations were comparable to those of typical CRPS-1.8) Further controlled studies are needed to evaluate the efficacy of early SCS in the severe neuropathic pain of NA.
Temporary SCS was effective in achieving an adequate analgesia in the acute phase of NA and chronic SCS was also useful to control the chronic pain. However, NA has been known to spontaneously resolve and we think SCS trial should be limited to selected patients with pain is notoriously refractory to conservative management.
References
1. Bala MM, Riemsma RP, Nixon J, Kleijnen J. Systematic review of the (cost-)effectiveness of spinal cord stimulation for people with failed back surgery syndrome. Clin J Pain. 2008; 24:741–756. PMID: 18936591.

2. Burchiel KJ, Anderson VC, Wilson BJ, Denison DB, Olson KA, Shatin D. Prognostic factors of spinal cord stimulation for chronic back and leg pain. Neurosurgery. 1995; 36:1101–1110. discussion 1110-1111PMID: 7643988.

3. Cruz-Martínez A, Barrio M, Arpa J. Neuralgic amyotrophy: variable expression in 40 patients. J Peripher Nerv Syst. 2002; 7:198–204. PMID: 12365568.

5. Geertzen JH, Groothoff JW, Nicolai JP, Rietman JS. Brachial plexus neuropathy. A long-term outcome study. J Hand Surg Br. 2000; 25:461–464. PMID: 10991813.

6. Grabow TS, Tella PK, Raja SN. Spinal cord stimulation for complex regional pain syndrome: an evidence-based medicine review of the literature. Clin J Pain. 2003; 19:371–383. PMID: 14600537.

7. Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, Molet J, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007; 132:179–188. PMID: 17845835.

8. Merskey H, Bogduk N. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. ed 2. Seattle, WA: IASP Press;1994.
9. Meyerson BA, Linderoth B. Mode of action of spinal cord stimulation in neuropathic pain. J Pain Symptom Manage. 2006; 31(4 Suppl):S6–S12. PMID: 16647596.

10. Moriyama K. Effect of temporary spinal cord stimulation on postherpetic neuralgia in the thoracic nerve area. Neuromodulation. 2009; 12:39–43. PMID: 22151221.

11. Sathasivam S, Lecky B, Manohar R, Selvan A. Neuralgic amyotrophy. J Bone Joint Surg Br. 2008; 90:550–553. PMID: 18450616.

12. Son BC, Kim DR, Lee SW, Chough CK. Factors associated with the success of trial spinal cord stimulation in patients with chronic pain from failed back surgery syndrome. J Korean Neurosurg Soc. 2013; 54:501–506. PMID: 24527193.

13. Stutz CM. Neuralgic amyotrophy: Parsonage-Turner Syndrome. J Hand Surg Am. 2010; 35:2104–2106. PMID: 21035964.

14. Suarez GA, Giannini C, Bosch EP, Barohn RJ, Wodak J, Ebeling P, et al. Immune brachial plexus neuropathy: suggestive evidence for an inflammatory-immune pathogenesis. Neurology. 1996; 46:559–561. PMID: 8614534.

15. Taylor RS, Van Buyten JP, Buchser E. Spinal cord stimulation for complex regional pain syndrome: a systematic review of the clinical and cost-effectiveness literature and assessment of prognostic factors. Eur J Pain. 2006; 10:91–101. PMID: 16310712.

16. Tonali P, Uncini A, Di Pasqua PG. So-called neuralgic amyotrophy: clinical features and long term follow-up. Ital J Neurol Sci. 1983; 4:431–437. PMID: 6674243.

17. van Alfen N. Clinical and pathophysiological concepts of neuralgic amyotrophy. Nat Rev Neurol. 2011; 7:315–322. PMID: 21556032.

18. van Alfen N. The neuralgic amyotrophy consultation. J Neurol. 2007; 254:695–704. PMID: 17446996.

20. van Alfen N, van der Werf SP, van Engelen BG. Long-term pain, fatigue, and impairment in neuralgic amyotrophy. Arch Phys Med Rehabil. 2009; 90:435–439. PMID: 19254608.

21. van Alfen N, van Engelen BG. The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain. 2006; 129(Pt 2):438–450. PMID: 16371410.

22. van Alfen N, van Engelen BG, Hughes RA. Treatment for idiopathic and hereditary neuralgic amyotrophy (brachial neuritis). Cochrane Database Syst Rev. 2009; (3):CD006976. PMID: 19588414.

23. van Alfen N, van Engelen BG, Reinders JW, Kremer H, Gabreëls FJ. The natural history of hereditary neuralgic amyotrophy in the Dutch population: two distinct types? Brain. 2000; 123(Pt 4):718–723. PMID: 10734003.

24. van Eijs F, Smits H, Geurts JW, Kessels AG, Kemler MA, van Kleef M, et al. Brush-evoked allodynia predicts outcome of spinal cord stimulation in complex regional pain syndrome type 1. Eur J Pain. 2010; 14:164–169. PMID: 19942463.

25. Vriesendorp FJ, Dmytrenko GS, Dietrich T, Koski CL. Anti-peripheral nerve myelin antibodies and terminal activation products of complement in serum of patients with acute brachial plexus neuropathy. Arch Neurol. 1993; 50:1301–1303. PMID: 8257306.

26. Yanamoto F, Murakawa K. The effects of temporary spinal cord stimulation (or spinal nerve root stimulation) on the management of early postherpetic neuralgia from one to six months of its onset. Neuromodulation. 2012; 15:151–154. discussion 154PMID: 22376181.

27. Yu DK, Cho YJ, Heo DH, Hong MS, Park SH. Neuroradiologic and neurophysiologic findings of neuralgic amyotrophy. J Korean Neurosurg Soc. 2010; 48:423–428. PMID: 21286479.

FIGURE 1
Pain distribution and magnetic resonance imaging (MRI) findings of neuralgic amyotrophy. A: A drawing shows the patchy distribution of pain in shoulder, medial forearm, palm, and fingers which corresponded to the sensory abnormality. Dotted areas represent a presence of an allodynia and the gray area indicate an area of dull, crushing, and deep pressure-like pain, and a black area in the left hand had a severe pain combined with an allodynia. B, C: A T2-weighted coronal MRI (B) and a gadolinium-enhanced, T1-weighted coronal image (C) shows diffuse swelling, increased signal intensity of the superior, middle, and inferior trunks of the left brachial plexus and its divisions. In addition, a soft tissue swelling and enhancement of the left deltoid region and a small joint effusion in the shoulder joint were seen. D: Three phase bone scintigraphy showing an increased perfusion in the left hand and fingers (painful area) and decreased perfusion of the right hand and wrist in the blood pooling phase. E: A digital infrared thermal imaging shows a decreased temperature in the left hand and fingers and right fingers.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download