Introduction
Leg swelling in patients with paraplegia due to spinal cord injury (SCI) occurs for various reasons, including heterotopic ossification (HO), deep vein thrombosis (DVT), fracture, or cellulitis.
310) Patients with SCI have an increased risk of lower extremity fractures because of decreased bone mass due to disuse atrophy, increased bone resorption, and hypercalciuria.
3) Trivial trauma can cause a fracture that may go unnoticed or may be belatedly diagnosed because of decreased sensation in the lower extremities.
3) Patients with cellulitis may also present with a swollen and erythematous leg.
3) HO is a process of benign bone formation with growth outside of normal skeletal locations and is a complication after SCI.
511) DVT and subsequent pulmonary embolism (PE) remain significant causes of morbidity and mortality in patients with SCI.
13) Unfortunately, the clinical presentations of these conditions may overlap in part or in whole and may occasionally be difficult to distinguish. However, a prompt diagnostic work-up to identify the cause of leg swelling, particularly for DVT, is essential to avoid mortality and morbidity.
We report a case of leg swelling in a paraplegic patient, resulting from HO mimicking DVT and discuss the differential diagnosis.
Go to :

Case Report
A 35-year-old man with C7 tetraplegia (American Spinal Injury Association Impairment Scale B) was admitted for rehabilitation. He had a fall down injury 3 months ago and suffered cervical SCI resulting in tetraplegia. He had a C5 burst fracture with a compressed spinal cord and underwent anterior cervical corpectomy and fusion. Although the pins-and-needles sensations over the arms and motor power in the upper extremities had improved slightly, paraplegia and voiding difficulty remained unchanged after the surgery. He was discharged 1 month after the surgery and was undergoing rehabilitation therapy at other hospital.
His vital signs were stable at the time of readmission to our hospital. One week after readmission, his left leg became swollen, erythematous, and warm, with a 2.5 cm greater left thigh circumference than the right thigh and a 2 cm greater left calf circumference than the right calf. He was afebrile, and vital signs were stable. The laboratory findings showed white blood cell count, 4,620 cells/mm
3 (normal 4,000 to 10,000 cells/mm
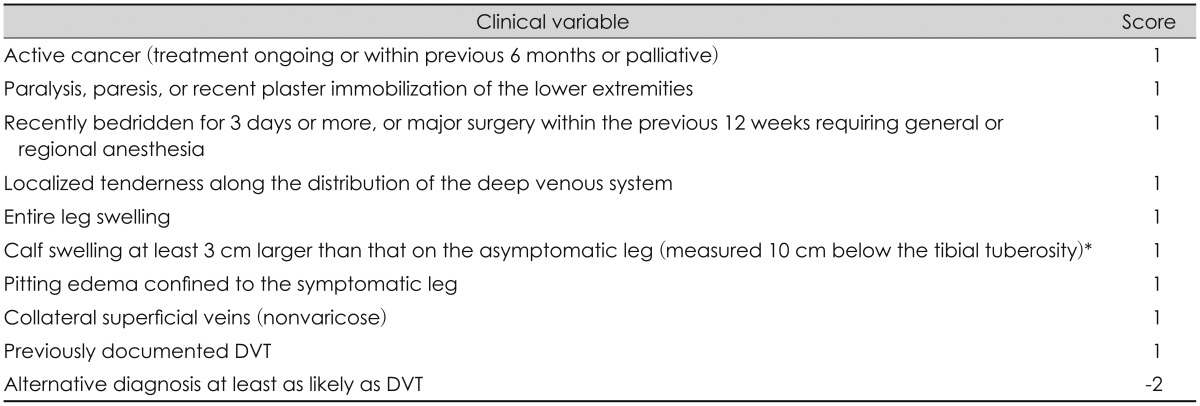
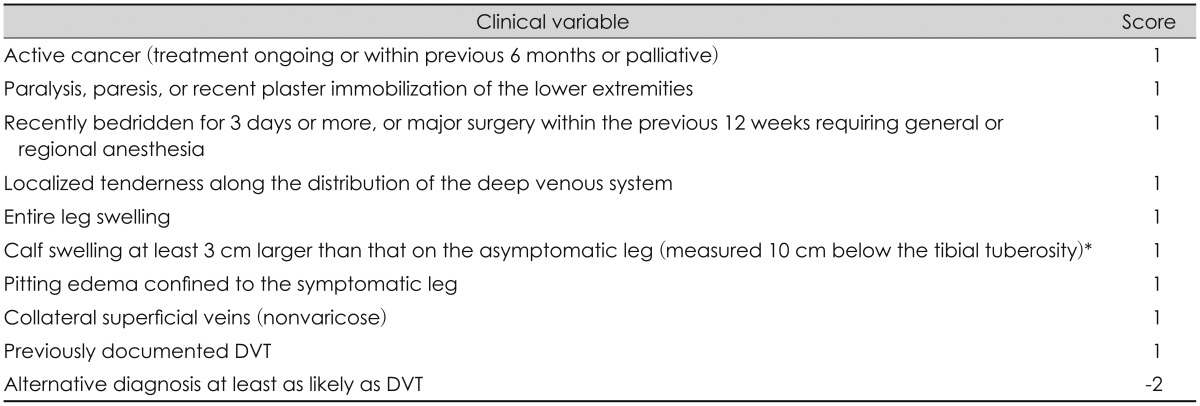
3); erythrocyte sedimentation rate, 46 mm/hr (normal 0 to 9 mm/hr); C-reactive protein (CRP), 2.56 mg/dL (normal <0.5 mg/dL); serum alkaline phosphatase (ALP), 140 U/L (normal 35-129 U/L); serum calcium, 9.2 mg/dL (normal 3.4 to 7.2 mg/dL); and D-dimer, 290 µg/L (normal 0-324 µg/L). Urinalysis revealed no pyuria or bacteriuria. Although CRP was elevated, a urinary tract infection (UTI) was treated with antibiotic and the value was lower compared to the initial one. Initially, we suspected DVT rather than HO or cellulitis because the leg swelling was through the entire unilateral leg, not focal swelling in the involved area. Although the D-dimer level was within the normal range, he had at least moderate probability for DVT according to the simplified clinical model for assessment of DVT by Wells (
Table 1).
17) Because of the higher morbidity associated with DVT and the potentially life-threatening complications of PE, he underwent immediate Doppler ultrasonography (USG), but no evidence of DVT in lower extremity veins was detected. Although the D-dimer level was normal and no DVT was found on USG, computed tomography venography (CTV) was performed because of the moderate to high probability for DVT. HO was located anteromedial to the left femur on CTV and displaced the iliopsoas muscle anteromedially. The diameter of the left external iliac vein (EIV) was narrower compared to the right one (
Figure 1). The EIV was compressed between the displaced iliopsoas muscle and the inguinal ligament, and poststenotic dilatation of the EIV was noted (
Figure 1C).
 | FIGURE 1Computed tomography venography of the lower extremities. A: Coronal source image of venography shows heterotopic ossification (HO) (white arrow) and narrowing of the left external iliac vein (EIV) (black arrow) compared to the right vein (arrowhead). B: Axial source image of venography shows HO (white arrow) located anteromedial to the femur and displaces the iliopsoas muscle anteromedially (asterisk). Narrowing of the diameter of left EIV (black arrow) is noted compared to the right vein (arrowhead). C: Three-dimensional reconstruction image shows HO (white arrows) located anteromedial to the femur. Narrowing of the left EIV (black arrow) compared to the right vein (arrowhead) under the region where the inguinal ligament runs is noted.
|
TABLE 1
Simplified clinical model for assessment of deep vein thrombosis14)

Etidronate (20 mg/kg/day orally for 2 weeks, followed by 10 mg/kg/day orally for 12 weeks) was prescribed under the impression of HO. To prevent the progression of HO, he received radiation therapy with a single dose of 7 Gy to the calcified portion in the CTV and to adjacent soft tissue, lateral part of the pelvic bone, and the femur. Although radiographic regression of HO was not confirmed, his leg swelling improved at the 3 month-follow-up.
Go to :

Discussion
HO is a process of benign bone formation with growth outside of normal skeletal locations, and the exact etiology and pathogenesis remain unknown.
511) Patients with SCI have a high risk of developing HO, with an incidence of 1% to 78%.
15) Patients with associated spasticity and thoracic trauma, complete lesion, pneumonia, presence of tracheostomy, and UTI have a higher risk of developing HO.
5) HO following SCI occurs most frequently within the first 2 to 3 weeks following SCI and occurs below the level of paralysis, and predominantly (up to 97%) in the hip.
1113) HO of the knee and distal femur are less common locations seen in patients with SCI, and the wrists, ankles, hands, and feet are almost never involved.
11) Ossified tissues extend from the pubic symphysis to the anteromedial femoral shaft posterior to the femoral neurovascular structures in cases of HO in the hip, and ossification is seen anteriorly involving the iliopsoas and femoral neurovascular structures, laterally within the gluteus minimus, and posteriorly extending from the ilium to the posterior femur encasing the sciatic nerve.
11) In the present case, HO was located anteromedially to the femur and displaced the iliopsoas muscle anteriorly. The EIV was compressed between the displaced iliopsoas muscle and the inguinal ligament.
HO typically presents clinically before it can be diagnosed radiologically.
11) The clinical presentation of HO is often related to local soft tissue inflammation and may include redness swelling, and local heating sensation in the involved area, and loss of joint mobility at the site of the lesion.
51113) A systematic inflammatory response, such as fever, may also occur.
313) Serum ALP levels increase significantly over the first 6 to 12 weeks after injury in patients who develop HO, and this may be a helpful adjunct in the diagnosis of HO early, particularly in patients who cannot report pain or in whom a physical exam is not possible or practical.
11) However, the predictive value of ALP has not been validated.
13) An imaging study can be helpful. Three-phase nuclear bone scanning is positive during the early phase of HO, with increased uptake of osteotropic radionucleotides.
1113) Nuclear bone scans are more sensitive than plain radiography and can detect HO as early as 2 weeks after symptomonset.
1113) The use of USG has also been assessed to diagnose HO prior to radiographic evidence.
13) A diagnosis of HO generally cannot be made until 3-6 weeks after symptom onset on plain radiography.
11) More recent data suggest that magnetic resonance imaging reveals changes consistent with the formation of HO 1 to 2 days after symptomonset.
11) A computed tomography scan evaluation substantially enhances the understanding of the extent of HO and its three-dimensional relationship with the joint and surrounding neurovascular structures.
1113) Mainstays of management include primary and secondary prevention with radiation, non-steroidal anti-inflammatory drugs, and bisphosphate.
1113) The majority of patients with HO run a relatively benign course without severe complications.
5) Therefore, the diagnosis of HO may not be urgent. However, this is not the case in patients with DVT. Unfortunately, a presentation of HO often overlaps with features similar to DVT, such as warmth, erythema, swelling, and limited range of motion of joint.
310) It may be sometimes difficult to distinguish clinically between HO and DVT, particularly when the patient presents with unilateral leg swelling. In general, edema of the entire leg is the most common clinical signs of an acute DVT.
2) In patients with HO, the swelling is localized or occurs in peri-articular area due to interstitial edema of the soft tissue.
1516) Therefore, we were initially suspicious of DVT rather than HO because the leg swelling was not focal or limited, but was diffuse through the entire left leg. Although CRP was elevated, the value was lower compared to the initial one in the present case. Therefore, we thought cellulitis was less likely to cause leg swelling.
The incidence of DVT in patients with SCI was reported to be greater than 50% in early prospective studies and has been estimated with the incidence as high as 5% with fatal PE.
12) Therefore, a prompt diagnosis of DVT and initiation of anticoagulation therapy are essential. Although only 20% of DVTs extend into the proximal veins, they result in over 80% of symptomatic DVTs.
12) The clinical diagnosis of DVT and PE are often unreliable, and diagnostic testing is necessary to confirm the diagnosis.
12) The D-dimer assay is a rapid, noninvasive, and inexpensive test that measures D-dimers, a fibrin degradation product, as fibrin is the main component of thrombosis.
91217) The D-dimer test is highly sensitive, but not specific because D-dimers are found in other non-thrombotic states, including recent major surgery, hemorrhage, trauma, malignancy, orsepsis.
17) D-dimer levels increase with age and through pregnancy.
17) In general, the D-dimer threshold for a normal test result is less than 500 µg/L, but 25% to 30% patients with normal D-dimer value have DVTs.
68) The simplified clinical model for assessment of DVT by Wells
17) is the first published model and the most widely validated and used. The risk of DVT is 27% for intermediate scores and 66% for high scores.
9) In patients with the Wells score ≤1 point and a normal D-dimer value, it is safe to withhold anticoagulant therapy without further testing.
17) However, patients with a negative D-dimer test combined with moderate or high risk of DVT scores according to Wells is not adequate to exclude DVT.
917) USG is the preferred imaging modality, as venous USG is inexpensive and noninvasive, and can be done as a screen or serially to monitor the patient. Sensitivity is 73% to 75% for distal clots, but 89-96% for the more dangerous proximalclots.
911) In a recent meta-analysis, a pooled sensitivity for CTV was about 96%, with a pooled specificity of about 95%, which are within the range of USG.
614) However, USG is unreliable for diagnosing thrombus below the knee and above the inguinal ligament.
47) CTV could be useful in patients with a suspected DVT in whom USG cannot be performed or is less reliable, such as those with morbid obesity or casts.
4) An important advantage of CTV compared to USG is that CTV can further reveal a thrombus in the iliac or inferior cava vein or large pelvic veins, which may cause major symptomatic DVT.
7) In addition, CTV can be a useful to detect of another causes of leg swelling, such as HO, cellulitis, and fractures at one time, as in the present case.
4) These observations lead us to perform CTV despite the normal D-dimer level and no DVT on USG to rule out thrombus in the veins above the inguinal ligament and other lesions to cause leg swelling. However, contrary to our expectations, HO was found on CTV of the lower extremities. No DVT in the proximal veins, no fracture in a lower extremity bone, and no contrast enhanced lesion in soft tissue, suggestive of cellulitis, were found on CTV.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download